Why is It Still Taboo to Talk about Vaginismus? The Importance of Early Diagnosis
- 1. Universidade Federal do Piauí (UFPI), Brazil
Abstract
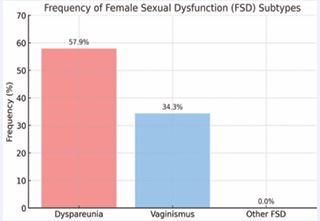
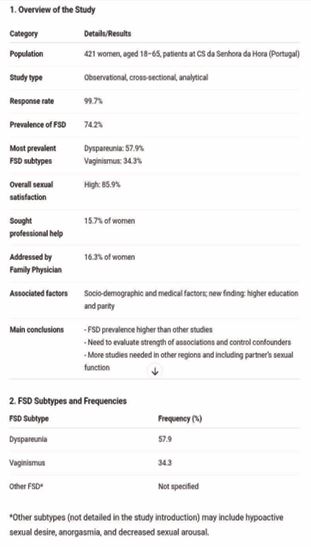
Vaginismus is a female sexual dysfunction characterized by the involuntary contraction of the pelvic floor muscles, which hinders or prevents vaginal penetration. Despite being relatively common, the condition is still surrounded by taboo, shame, and misinformation, causing many women to suffer in silence. This article discusses the consequences of silence — including emotional impact, low self-esteem, and relationship difficulties — and emphasizes the importance of early diagnosis. Specialized interventions in female sexuality, pelvic physiotherapy, and psychology are essential for effective treatment. Breaking the taboo through information, dialogue, and experience sharing is crucial to promote autonomy, empowerment, and well-being for affected women. Observational studies in Portugal show a high prevalence of female sexual dysfunction, with 74.2% of women evaluated presenting some type of dysfunction, most commonly dyspareunia (57.9%) and vaginismus (34.3%). Despite the high prevalence, only 15.7% sought professional help, and the topic was addressed by family physicians in only 16.3% of cases highlighting the need for greater attention to early diagnosis and professional support.
Keywords
• Vaginismus; Female sexual dysfunction; Early diagnosis; Prevalence; Dyspareunia; Primary care
Citation
de Sousa Araujo S (2025) Why is It Still Taboo to Talk about Vaginismus? The Importance of Early Diagnosis. JSM Sexual Med 9(5): 1169.
INTRODUCTION
Vaginismus is a female sexual dysfunction marked by involuntary contraction of the pelvic floor muscles, which hinders or prevents vaginal penetration [1]. Although it affects a significant portion of the female population, the condition remains surrounded by taboo, silence, and misinformation, causing many women to suffer privately, carrying shame, fear, and guilt [2].
Social stigma and lack of adequate sexual education contribute to underreporting of vaginismus, even among healthcare professionals [3]. Beyond physical impact, the condition affects self-esteem, relationships, and self- perception. Studies indicate prevalence ranges from 1% to 6% among sexually active women, while sexual dysfunction related to pain may reach 42%, demonstrating its clinical and social relevance [4,5].
Recent data from Portugal reinforce this reality: in a sample of 421 women attending primary care, 34.3% presented vaginismus, highlighting the high frequency of the problem and the low rate of seeking professional help (15.7%) [3]. International research shows similar prevalence, ranging from 11.7% to 42% among women with sexual dysfunction [5,6], emphasizing the need for greater awareness and early diagnosis (Figure 1).
Figure 1 Subtypes of Female Sexual Dysfunction (FSD) and their frequencies in the study sample.
Early diagnosis is essential, as the sooner women understand the condition, the more effective the treatment [7], Specialized interventions — such as pelvic physiotherapy, psychology, sexual therapy, and medical follow-up — can relieve pain, restore sexual function, and improve quality of life [8,9]. Breaking the taboo, encouraging dialogue, and disseminating reliable information are fundamental steps to transform vaginismus from an invisible pain to a comprehensible and treatable condition [10,11].
Taboo and Emotional Impact
Vaginismus is a silent pain, often invisible, loaded with shame, fear, and guilt [2]. Lack of information and social stigma lead many women to suffer alone, feeling “defective” or “incapable.” The condition also affects relationships due to communication difficulties [1]. Breaking the silence is crucial, as discussing vaginismus involves not only physical pain but deep emotional experiences [10]. Sharing information and personal accounts helps demystify the condition, encourages women to seek support, and creates a culture of empathy [11].
Causes and Treatment
Vaginismus may have physical, emotional, or combined causes, including trauma, rigid upbringing, anxiety, and misinformation about the body [6]. Beyond a physical problem, it impacts self-esteem, relationships, and self perception [2].
Effective treatment relies on early diagnosis and follow-up by professionals specialized in female sexuality. Pelvic physiotherapy, psychology, sexual therapy, gradual desensitization, and individualized medical support provide safe conditions for sexual function recovery and emotional strengthening [7,8]. Research indicates that vaginal dilators and, in some cases, Botox with local anesthetics can complement therapy [9].
Brazilian research with 51 women diagnosed with primary vaginismus showed most were aged 29–39, had completed higher education, and were in stable unions. Many associated vaginismus with rigid upbringing. While 68% were followed by gynecologists and 57% by pelvic physiotherapists, 35% were still in the diagnostic phase, and 37% in treatment, highlighting the need for more effective professional support. The interval between initial complaints and diagnosis was up to one year for 45% of participants, and over half (53%) expressed dissatisfaction with time to cure. Vaginismus impacted self-esteem in 47% of women, though 70% reported partner support during treatment [2].
These findings reinforce that vaginismus compromises sexual function and self-esteem, highlighting the importance of timely, integrated professional interventions [1].
CONCLUSION
Discussing vaginismus is an act of courage and a fundamental step toward transforming silent pain into a comprehensible and treatable experience. Information, dialogue, and courage allow women to recover intimate health, strengthen self-esteem, and build healthier relationships. National and international data show that, despite high prevalence, the condition remains underreported and little discussed [3,4]. Breaking the taboo promotes greater awareness of female health and encourages seeking professional support, enabling effective treatment and the well-being of affected women [7].
REFERENCES
- Aveiro MC, Garcia APU, Driusso P. Efetividade de intervenções fisioterapêuticas para o vaginismo: uma revisão da literatura. Fisioter Pesq. 2009; 16: 279- 283.
- Lima IS, Sousa MLP, Carvalho MQ, Macedo SR. Implicações do vaginismo no cotidiano das mulheres. Revista Brasileira de Sexualidade Humana.2020; 31: 28-37.
- Disfunção sexual feminina: Prevalência e fatores relacionados.Revista Portuguesa de Medicina Geral e Familiar. 2006; 22: 701-720.
- Pithavadian S. Prevalence of vaginismus in Denmark. PMC. 2023
- Bulbuli S, Vaishnavi AK. Prevalence of vaginismus in reproductive age group: observational study. ResearchGate. 2024; 16: 198-201.
- Yavuzkir S. Association between vaginismus and anxiety disorders: a biopsychosocial approach. SAGE J. 2024.
- Maseroli E, Scavello I, Rastrelli G, Limoncin E, Cipriani S, Corona G, et al. Systematic review of interventions for vaginismus: sexual therapy and desensitization. 2018; 15: 1752-1764
- Tamara Melnik, Keith H, Hugh MG. Therapeutic strategies for vaginismus: sexual therapy and desensitization. PMC. 2012.
- Pacik P. Use of vaginal dilators, Botox, and anesthetics in vaginismus treatment. Science Direct. 2017.
- El País. Quando o sexo com penetração provoca dor: visibilidade dovaginismo. 2025.
- Cadena SER. Visibilizando o vaginismo na Espanha: importância do diagnóstico precoce.2025