Prevalence of Complications Following Cervical Unilateral Open-Door Laminoplasty in Cervical Spondylosis Patients: Systematic Review and Meta Analysis
- 1. Department of Neurosurgery, Udayana University, Indonesia
Abstract
Background: Cervical spondylosis is a degenerative diseaseresulted from multi factorial degenerative changes. It can manifest as neck pain, radiculopathy and/ or myelopathy. Cervical laminoplasty is considered as one of the safest technique to treat cervical spondylosis. However, this technique also has several complications following the surgery. It is important for neurosurgeon to know the complications of this technique. Objectives: To determine the prevalence of complications following cervical unilateral open-door laminoplasty in cervical spondylosis patients through systematic review and meta-analysis.Methods: This review includes all full-text articles that examine cervical unilateral open-door laminoplasty in cervical spondylosis patients. PubMed Central, BioMed Central, and Public Library of Science database were searched using keyword “cervical laminoplasty”. Included article was assessed for risk of bias. Results: The prevalence of axial pain was 21%, C5 palsy was 6%, CSF leakage was 3%, hematoma was 2%, infection was 3%, Dural tear was 3%, and kyphosis was 10%. There was high heterogeneity between studies. Conclusions: The complication with highest prevalence was axial pain with 21% while hematoma was the lowest prevalence with 2%.
CITATION
Mardhika PE, Putra MB, Mahadewa TGB (2018) Prevalence of Complications Following Cervical Unilateral Open-Door Laminoplasty in Cervical Spondylosis Patients: Systematic Review and Meta Analysis. JSM Spine 3(1): 1016.
INTRODUCTION
Rationale
Cervical spondylosis is multifactorial degenerative changes that contribute to spinal canal and neural foramina narrowing of cervical spine. The presentation of this condition can be asymptomatic or symptomatic. There are 3 types of cervical spondylosis symptom, which are neck pain (acute or chronic), cervical radiculopathy and/or cervical myelopathy [1].
Cervical radiculopathy is sign of spinal nerve root problem. Symptoms can include weakness, atrophy, paresthesia, hyperesthesia, or hyperlagesia. It can be caused by herniated nucleus pulposus (HNP) or osteophytic lesion [1].
Cervical myelopathy is sign of spinal cord problem. Symptoms of myelopathy include neck and shoulder pain, sensory or motor changes. The sensory changes can be electrical shock sensation, numbness, and paresthesias. The motor changes can be spasticity, reduce of dexterity, and spastic gait. The classic clinical findings of myelopathy are hyperreflexia, increased muscle tone, atrophy in distal of stenosis level, fasciculation, sphincter dysfunction and presence of pathological reflex [1].
The basic pathogenesis of cervical spondylosis is started with static mechanical factors. They include congenital canal stenosis, disc herniation, degenerative osteophyte growth, ligamentumflavum hypertrophy, andossification of posterior longitudinal ligament (OPLL). These static factors can compress the neural structure directly and manifest as radiculopathy and/or myelopathy sign and symptoms. However, they also can compress the vascular structure, which cause apoptosis of the neural structure and manifest as the same [1,2].
Laminoplasty is one of posterior approach techniques to treat cervical spondylosis. Hirabayashi was first described unilateral open-door laminoplasty with suture fixation in 1981[2,3]. The goal of laminoplasty is to provide decompression of the spinal cord by widening the spinal canal while preventing instability and scar in-growth after decompression [3].
Laminoplasty has been considered as safe technique to treat cervical spondylosis. However, this technique also has several complications following the surgery. Complications following the intervention are important to know for neurosurgeon. It is used to advice and to get consent from the patient before the surgery. Based on that, we would like todetermine and stratify the frequency of complications following cervical unilateral opendoor laminoplasty in cervical spondylosis patients by systematic review and meta-analysis
Objectives
The objective of this study is determining prevalence of complications following cervical unilateral open-door laminoplasty in cervical spondylosis patients by systematic review and meta-analysis.
METHODS
Eligibility criteria
Type of studies: This review will include all studies that provide full-text article examining cervical unilateral open-door laminoplasty in cervical spondylosis patients and report the complications following the surgery. However, we will exclude general review, systematic review, and meta-analysis study. Anatomic studies including computer analysis, mathematical analysis, and cadaveric study will be excluded too. If article made by same author at same institution is found, sample evaluation will be conducted to prevent sample duplication.Qualitative and economic studies will be excluded, because of irrelevant topic.
Studies published in English and Bahasa will be included. However, if we find article in other language, we will translate the article using Google translates and the author will decide whether it will be included or not. There will be no restriction regards to the year of publication.
Types of participants: This review will include studies with adult participants (age 18 years or older) of both genders who have suffered cervical spondylosis. Cervical spondylosis will be defined as condition caused by degenerative of vertebrae such as intervertebral disc herniation, cervical spondylotic myelopathy and/or radiculopathy, OPLL, and hypertrophy of ligamentumflavum. Participants in all settings and of all nationalities will be included. Studies that included children under 18 years old and participants with other condition such as spinal cord injury, tumor, and vascular problem will be excluded. Studies that include patients with history of other cervical surgery for same disease also will be excluded.
Types of interventions: The intervention under investigation is cervical unilateral open-door laminoplasty. In this context, cervical unilateral open-door laminoplasty will be considered as expanding cervical spine canal by elevating the lamina of unilateral side and use other side of lamina as hinge. All the technique to maintain the opened lamina such as suturing, miniplate, titanium plate, ceramic spacer and etc. will be included to the review.
We will exclude studies that not describe the surgical technique and combine unilateral open-door laminoplasty with other technique.
Types of outcomes: The outcome that will be examined is complications following the surgery. We will divide complications into several categories, which are “axial pain”, “C5 palsy”, “duraltear and CSF leakage”, “kyphosis”, “hematoma”, and”infection”. However, we will describe other complication that we found narrative.
Information sources
.Search strategy must be established to perform comprehensive and systematic search. Initially, we will perform systematic search using keywords “cervical laminoplasty” in major databases, which are PubMed Central, BioMed Central, and Public Library of Science. We will also perform electronic search using search engine such as Google Scholar and Directory of Open Access Journal using same keywords..
Study selection
The selection process of studies will be done by two authors (EM and BP) to reduce the possibility of discarding relevant reports. If there is disagreement whether a study should be included or not, decision of third author will be used.
The result of systematic search will be merged and duplicate record will be removed. On first stage, titles and abstracts will be examined and irrelevant studies such as off topic report, case report, review, and anatomic studies will be removed. Second stage, full article of potentially relevant studies will be retrieved and examined for compliance with eligibility criteria of the review. Studies that will be included in this review have to comply the inclusion and exclusion criteria. Final stage, included studies will be assessed for their quality and then will be decided for including in this review.
Data collection process
Electronic data collection form will be used to collect data by each author. The collected data by each author will be merged and be managed with software Review Manager 5.3.
Data items
We will collect several items from the included studies. The data items are author’s name, year of publication, method, sample size, diagnosis of participant, age (mean), surgical technique within the study, and complication data.
Risk of bias in individual studies
After the completion of the literature search, studies that meet the inclusion criteria of the review will be assessed for their quality to determine their internal and external validity and reliability. This will involve the critical appraisal of the identified studies that will be done independently by two reviewers using standardized critical appraisal tools. This review will use Joanna Briggs Institute (JBI) critical appraisal tool based on study design.
It will involve two reviewers to increase the validity of the results and reduce the possibility of selection bias and minimize the possibility of rejecting relevant studies. If disagreements occur between two reviewers and no conclusion can be reached, the decision of third independent reviewer will be sought. Following the critical appraisal, justifications for including or excluding the studies will be discussed.
To determine quality of the study, we use cut off point from the total score of JBI critical appraisal form. Low quality is defined as below half of the total score, while good quality is upper half of the total score
Synthesis of results
All the found complication data will be included in the narrative synthesis. However, in quantitative analysis, the complication data will be divided into several categories, which are “axial pain”, “C5 palsy”, “dural tear and CSF leakage”, “hematoma”, “infection”, and “kyphosis”. Included studies that reported complication of same category will be pooled and analyzed. Meta-analysis of prevalence will be conducted using MetaXL for Microsoft Excel Software and will be presented in forest plot diagram. The MetaXL software used double arcsine method to perform Meta analysis. In this study, we will conduct random effect pool analysis because high heterogeneity of the studies.
RESULTS
Study selection
The search strategy results a total of 1038 publications and 38 articles were selected for full text review. On screening stage, we excluded 818 articles because of off topic titles. Abstract screening resulted in exclusion of 77 articles, which are case reports, reviews, systematic review and meta-analysis, anatomic studies, and less than 10 samples study. Studies that examined other technique, spinal cord injury (SCI) and spinal cord ischemia patients were also excluded. (Table 1) On eligibility stage, 54 articles were excluded due to several reasons.
| Table 1. Abstract screening. | |
|---|---|
| Reason for exclusion | Number |
| Review article | 16 |
| Anatomic study | 7 |
| Systematic review and meta-analysis | 19 |
| Case report | 11 |
| Irrelevant technique | 14 |
| Irrelevant samples | 8 |
| < 10 samples | 2 |
| TOTAL |
77 |
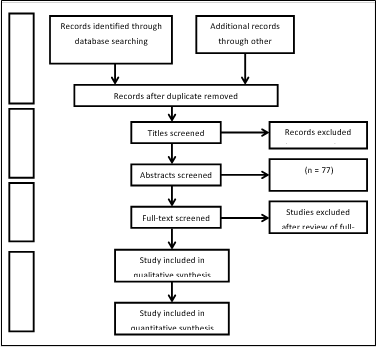
(Table 2) The study selection process with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowcan is seen in (Figure 1). We excluded 2 study for quantitave synthesis because these
| Table 2. Full-text eligibility. | |
|---|---|
| Reason for exclusion | Number |
| Irrelevant samples | 1 |
| No complication data | 11 |
| Combined technique | 8 |
| No diagnosis data | 3 |
| No diagnosis data | 12 |
| No age description | 1 |
| Irrelevant technique | 15 |
| History of cervical surgery before | 2 |
| Mixed intervention group | 1 |
| TOTAL | 54 |
Figure 1: PRISMA flow diagram of study selection process.
Studies reported complication other than determined category for meta-analysis.
Study characteristics
In this study, we include 38 full-text articles, which are 19 cohort studies, 14 before-after comparison studies, and 5 case control studies. Complete study characteristic is detailed in appendix 1. Overall, year of publication varied from 2004 until 2018 and mean age varied from 51.2 to 82.9 years old.
Risk of bias within studies
We analyzed risk of bias within studies using JBI critical appraisal checklist for cohort, quasi-experimental and case control studies. Each checklist form has different total score value. Score of each study by each reviewer can be seen in appendix 2-10
From the analysis, 37 articles were in good quality while 1 article was in low quality.
Result of individual studies
The result of individual studies can be seen in appendix
1. Overall, the reported complications vary from clinical, radiological, and hardware complication.
Synthesis of results
In this systematic review, basically we divided the complications into 3 groups. They are clinical, radiological and hardware complication
Clinical complication
The clinical complications of cervical unilateral open-door laminoplasty for cervical spondylosis patients are axial pain, C5 palsy, C6 root injury, wound infection or poor wound healing, CSF leak, hematoma, dural tear, recurrent stenosis, persistent radiculopathy, and delirium [4-6].
One case of C6 root injury was reported by Mandal et al.[7]. in study with 60 samples. Recurrent stenosis and persistent radiculopathy were reported by Woods et al. [8]. with one case each in 39 samples.
Delirium was described and reported in 3 articles with total incidence was 12 of 245 total samples [4-6]. Other clinical complications will be presented in meta-analysis section.
Radiological complication
The radiological complications of this technique for cervical spondylosis patients are lamina reclosure, kyphosis,hinge fracture,unhealed hinge, and vertebral slippage.
Lamina reclosure was described in 6 articles [9,10,10,12,13,14], however only 2 articles [13,14] reported 2 case of lamina reclosure. The total incidence of lamina reclosure in this systematic review was 2 of 614 samples.
Hinge fracture and unhealed hinge were described in 5 articles [15,16,17,18,19]. Hinge fracture was reported in 2 articles [15,17] with total incidence was 19 of 72 total samples, while unhealed hinge was reported in 2 articles [17,18] with total incidence was 12 of 137 total samples.
Vertebral slippage was only reported in 1 article with total incidence was 3 of 65 total samples [14]. Kyphosis will be presented in meta-analysis section.
Hardware complication
In this systematic review, there were nohardware complications reported, such as plate dislodged, screw back out, screw looseness, screw shifting, hardware break, loss of fixation, dislocation of hardware, and loosening anchor [9,20,7,16,21,22,23].
Meta-analysis
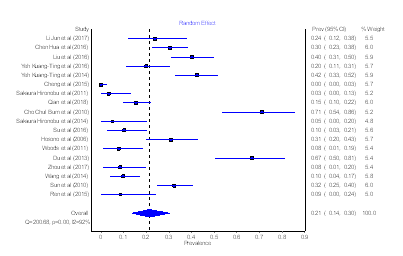
Axial Pain: We included 18 articles in prevalence metaanalysis of axial pain, which are 11 cohort, 1 case control, and 6 before-after comparison studies. There are total 1188 samples included in this meta-analysis (Table 3).
| Table 3: Study included for axial pain analysis. | ||
|---|---|---|
| Study (Year) | Case | Total Sample |
| Li Jun et al4 (2017) | 10 | 42 |
| Chen Hua et al5 (2016) | 39 | 129 |
| Liu et al6 (2016) | 41 | 102 |
| YehKuang-Ting et al7 (2016) | 13 | 65 |
| YehKuang-Ting et al8 (2014) | 44 | 104 |
| Cheng et al9 (2015) | 0 | 60 |
| Sakaura Hironobu et al15 (2011) | 1 | 31 |
| Qian et al17 (2018) | 21 | 137 |
| Cho Chul Bum et al19 (2010) | 22 | 31 |
| Sakaura Hironobu et al20 (2014) | 1 | 20 |
| Su et al22 (2016) | 5 | 49 |
| Hosono et al23 (2006) | 20 | 65 |
| Woods et al27 (2011) | 3 | 39 |
| Du et al29 (2013) | 24 | 36 |
| Zhou et al32 (2017) | 3 | 36 |
| Wang et al33 (2014) | 8 | 83 |
| Sun et al39 (2010) | 44 | 136 |
| Ren et al40 (2015) | 2 | 23 |
| Total | 301 | 1128 |
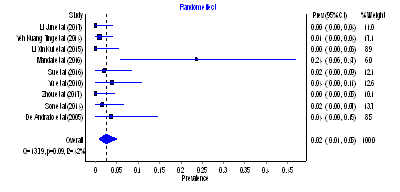
There was high level of heterogeneity across the included studies (I2 = 92%, p=0.00). The random effect pooled prevalence of axial pain was 21% (95% CIs = 14 – 30) (Figure 2).
Figure 2: Forest plot of axial pain prevalence.
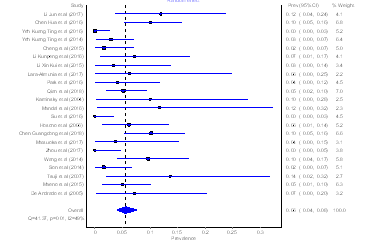
C5 Palsy: There are 22 articles that are included in C5 palsy prevalence meta-analysis. They are 12 cohort, 1 case control, and 9 before-after comparison studies. There are total 1301 samples included in this meta-analysis (Table 4).
| Table 4: Study included for C5 palsyanalysis. | ||
| Study (Year) | Case | Total Sample |
| Li Jun et al4 (2017) | 5 | 42 |
| Chen Hua et al5 (2016) | 13 | 129 |
| YehKuang-Ting et al7 (2016) | 0 | 65 |
| YehKuang-Ting et al8 (2014) | 3 | 104 |
| Cheng et al9 (2015) | 1 | 60 |
| Li Kunpeng et al10 (2016) | 3 | 42 |
| Li Xin-Kui et al12 (2015) | 1 | 30 |
| Lara-Almunia et al13 (2017) | 1 | 16 |
| Park et al14 (2016) | 2 | 49 |
| Qian et al17 (2018) | 7 | 137 |
| Kaminsky et al18 (2004) | 2 | 20 |
| Mandal et al21 (2016) | 2 | 17 |
| Su et al22 (2016) | 0 | 49 |
| Hosono et al23 (2006) | 4 | 65 |
| Chen Guangdong et al24 (2018) | 12 | 118 |
| Matsuoka et al26 (2017) | 1 | 27 |
| Zhou et al32 (2017) | 0 | 36 |
| Wang et al33 (2014) | 8 | 83 |
| Son et al34 (2014) | 1 | 62 |
| Tsuji et al37 (2007) | 3 | 22 |
| Maeno et al38 (2015) | 5 | 100 |
| De Andrado et al41 (2005) | 2 | 28 |
| Total | 76 | 1301 |
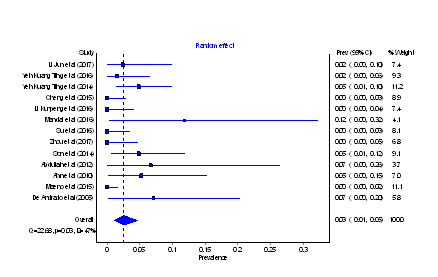
There was moderate level of heterogeneity across the included studies (I2 = 49%, p=0.01). The random effect pooled prevalence of C5 palsy was 6% (95% CIs = 4 – 8) (Figure 3).
Figure 3: Forest plot of C5 palsy prevalence.
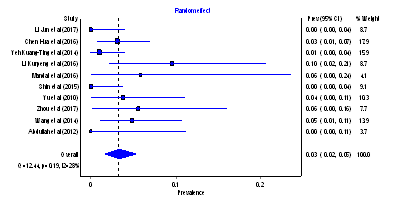
Dural Tear and Cerebrospinal Fluid (CSF) Leakage: We decided to merge dural tear and CSF leakage analysis considering that CSF leakage could happen because of dural tear. In dural tear and CSF leakage prevalence meta-analysis, we included 10 articles. They are 4 cohort, 2 case control and 4 before-after comparison studies. There are total 566 samples included in this meta-analysis (Table 5).
| Table 5. Study included for dural tear and CSF leakageanalysis. | ||
| Study (Year) | Case | Total Sample |
| Li Jun et al4 (2017) | 0 | 42 |
| Chen Hua et al5 (2016) | 4 | 129 |
| YehKuang-Ting et al8 (2014) | 1 | 104 |
| Li Kunpeng et al10 (2016) | 4 | 42 |
| Mandal et al21 (2016) | 1 | 17 |
| Shin et al25 (2015) | 0 | 45 |
| Yu et al28 (2010) | 2 | 53 |
| Zhou et al32 (2017) | 2 | 36 |
| Wang et al33 (2014) | 4 | 83 |
| Abdullah et al35 (2012) | 0 | 15 |
| Total | 18 | 566 |
There was low level of heterogeneity across the included studies (I2 = 28%, p=0.19). The random effect pooled prevalence of dural tear and CSF leakage was 3% (95% CIs = 2 – 5) (Figure 4).
Figure 4: Forest plot of dural tear and CSF leakage prevalence.
Hematoma: We included 9 articles in prevalence metaanalysis of hematoma, which are 3 cohort and 6 before-after comparison studies. There are total 421 samples included in this meta-analysis (Table 6).
| Table 6. Study included for hematomaanalysis. | ||
| Study (Year) | Case | Total Sample |
| Li Jun et al4 (2017) | 0 | 42 |
| YehKuang-Ting et al5 (2014) | 1 | 104 |
| Li Xin-Kui et al12 (2015) | 0 | 30 |
| Mandal et al21 (2016) | 4 | 17 |
| Su et al22 (2016) | 1 | 49 |
| Yu et al28 (2010) | 2 | 53 |
| Zhou et al32 (2017) | 0 | 36 |
| Son et al34 (2014) | 1 | 62 |
| De Andrado et al41 (2005) | 1 | 28 |
| Total | 10 | 421 |
There was moderate level of heterogeneity across the included studies (I2 = 42%, p=0.09). The random effect pooled prevalence of hematoma was 2% (95% CIs = 1 – 5) (Figure 5).
Figure 5: Forest plot of hematoma prevalence.
Infection: We included 13 articles in infection prevalence meta-analysis. They are 5 cohort and 8 before-after comparison studies. There are total 648 samples included in this metaanalysis (Table 7).
| Table 7. Study included for infectionanalysis. | ||
| Study (Year) | Case | Total Sample |
| Li Jun et al4 (2017) | 1 | 42 |
| YehKuang-Ting et al7 (2016) | 1 | 65 |
| YehKuang-Ting et al8 (2014) | 5 | 104 |
| Cheng et al9 (2015) | 0 | 60 |
| Li Kunpeng et al10 (2016) | 0 | 42 |
| Mandal et al21 (2016) | 2 | 17 |
| Su et al22 (2016) | 0 | 49 |
| Zhou et al32 (2017) | 0 | 36 |
| Son et al34 (2014) | 3 | 62 |
| Abdullah et al35 (2012) | 1 | 15 |
| Ahn et al36 (2010) | 2 | 38 |
| Maeno et al38 (2015) | 0 | 100 |
| De Andrado et al41 (2005) | 2 | 28 |
| Total | 17 | 648 |
Prevalence of Complications Following Cervical Unilateral Open-Door Laminoplasty in Cervical Spondylosis Patients: Systematic Review and Meta Analysis
There was moderate level of heterogeneity across the included studies (I2 = 47%, p=0.03). The random effect pooled prevalence of infection was 3% (95% CIs = 1 – 5) (Figure 6).
Figure 6: Forest plot of infection prevalence.
Kyphosis: In CSF leakage prevalence meta-analysis, we included 7 articles. They are 1 cohort, 2 case control and 4 beforeafter comparison studies. There are total 614 samples included in this meta-analysis (Table 9)
| Table 8. Study included for kyphosis analysis. | ||
| Study (Year) | Case | Total Sample |
| YehKuang-Ting et al8 (2014) | 10 | 104 |
| Cheng et al9 (2015) | 0 | 60 |
| Cao et al11 (2017) | 21 | 194 |
| Lee Jun Seok et al16 (2017) | 27 | 49 |
| Qian et al17 (2018) | 19 | 137 |
| Mandal et al21 (2016) | 2 | 17 |
| Yu et al28 (2010) | 0 | 53 |
| Total | 79 | 614 |
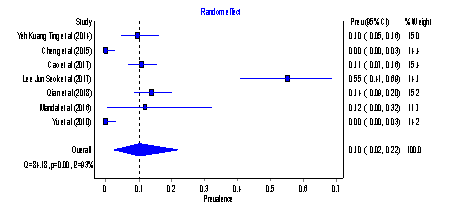
There was high level of heterogeneity across the included studies (I2 = 93%, p=0.00). The random effect pooled prevalence of kyphosis was 10% (95% CIs = 2 – 22) (Figure 7).
Figure 7: Forest plot of kyphosis prevalence.
DISCUSSION
Summary of evidence
Cervical unilateral open-door laminoplasty is one of several techniques to decompress the cervical spinal cord. The most common complication of this technique is axial pain. In this study, the highest pooled prevalence was axial pain with 21% of prevalence with high heterogeneity.Axial pain was reported as pain and stiffness on nuchal, [4,9,10,24-27] shoulder, [4,24] and scapular region [9,10,25,27] that can limit the neck motion [24]. In this article, we found several technique modification which contribute to decreasing of axial pain incidence.
The modified technique to reduce axial pain are C7 muscle insertion preservation, [10,14,25-27] careful repair of the semi spinal iscervicis muscle and nuchal ligament, [28,29] in situ reconstruction of extensor muscle insertion on the C2 spinous process, [20]and fixation using miniplate [24,20].Several studies also suggested that axial pain was caused by loss of cervical curvature [24,30] and Du et al. [30], suggested that restoring lordosis and strengthening the cervical stability could reduce the incidence of axial pain. Mini plate fixation could reduce axial pain because it interferes less with facet joint and reduce micro movement and muscle stimuli by non-union hinge [24]. Based on this analysis, cervical unilateral open door laminoplasty with preservation of C2 and C7 muscle insertion and mini plate fixation could reduce axial pain prevalence. Moreover, preoperative lordosis could prevent postoperative axial pain.
C5 palsy also is a common complication of cervical laminoplasty. In this study, C5 palsy was 6% of pooled prevalence. C5 nerve is a short nerve and located at the apex of cervical lordosis [7]. C5 palsy may happen because of overly wide opening of lamina that result in excessive cord shifting cause posterior rami injury and nerve root traction [10,28,11,13,7].Moreover, Several studies concluded that narrower preoperative foramina [11] and high degree anterior compression of the cord [31] were risk factor for C5 palsy incidence [32]. Several studies suggested that creating bilateral gutter more medially could reduce C5 palsy incidence [10,28].Kaminsky et al did careful elevation of lamina to prevent excessive shifting of the cord[13].
Studies that we found described dural tear and CSF leakage separately. However, in this study we decided to mergedural tear and CSF leakage analysis because CSF leakage could happen only because of dural tear. Dural tear in laminoplasty could happen because of incidental trauma, and usually dural repair is performed intraoperative directly [28,7,22].
In this review, we find studies which described hematoma thatvaried from “epidural hematoma” [32,7,16,22] to “hematoma” [28,12,19,5,33]. However, all study did not describe the definition of hematoma itself. Yeh et al performed C3-7 unilateral open door laminoplasty with titanium miniplates and miniscrew and reported 1 case of hematoma and conducted reoperation to evacuate the hematoma immediately [28]. Su et al., reported 1 case of epidural hematoma and still suffered partial limb paraplegia after evacuation [16].Yu et al., also reported 2 case of epidural hematoma and evacuated rapidly without any sequelae [22].
Infection is an issue of cervical unilateral open-door laminoplasty also. In this review, several studies reported poor wound healing because of infection. Yeh et al., reported 5 cases of poor wound healing because of diabetes mellitus type 2 [28]. Other studies did not describe possibility of cause of infection. Post operative infection was treated with debridement [10,28,23,34], maintenance of instrumentation [23] and antibiotic [28,7,34]. Overall, the infection treatment made good result. However, Ahn et al., reported 2 case of infection without improvement of Japanese Orthopedic Association (JOA) score [34].
Woods et al. reported 1 case of persistent radiculopathy and recurrent stenosis. Recurrent stenosis occurred because of large anterior osteophyte and persistent radiculopathy occurred because of development of uncovertebral spurs. Both of the patients had revision surgery [8] Several studies also reported delirium occurrence [4,5,6].Delirium occurred in elderly people who undergone laminoplasty for cervical spondylosis [5,6].
Kyphosis was the second highest pooled prevalence with 10% of prevalence. Kyphosis is already known as common complication of cervical laminoplasty. Kyphosis could happen because of disrupted dorsal ligament structure, compromised extensor musculature, and force from less mobile segment8 [28]. Another articles concluded that preoperative C2-7 sagittal vertical axis, destroyed facet joint and cephalad vertebral level undergoing laminoplasty (CVLL) also associated with postoperative kyphosis [35]. However, miniplate fixation could reduce possibility of destroyed facet joint and resulted in decreasing postoperative kyphosis incidence [35].
Lamina reclosure is a complication of laminoplasty. It occurs because of loose fixation of lamina. In this review, we found 2 articles that reported lamina reclosure case [13,14]. They performed laminoplasty with suture fixation [13] and another one performed laminoplasty with wire to fixate the lamina [14]. Other studies that performed laminoplasty with plate fixation reported 0 case of lamina reclosure [9,10,11]. Based on this, laminoplasty with plate fixation is a good technique to prevent lamina reclosure
.Incidence of hinge fracture in this review is 19 of 72 total samples. Park et al reported 3 cases of hinge fracture and immediately performed internal fixation using titanium miniplate [15] Incidence of unhealed hinge was 12 of 137 total samples. Unhealed hinge was described as “pseudoarthrosis”[16] , “not healed hinge” [17], “non fusion hinge” [18], and “non union” [19] across the found studies.
Hardware complications were not reported in all studies that describe hardware failure such as plate dislodged, screw back out, screw looseness, screw shifting, hardware break, loss of fixation, dislocation of hardware, and loosening anchor.
Limitation
This review searched in 3 databases only with search strategy that had been test before, so there may be possibility other relevant article in other database was not included. We also did not undertake search on grey literature, so other relevant article that unpublished was not included..
From the search result, we did not found randomized controlled trial study design. We only found cohort, casecontrol, and before-after test comparison study. However, it will reduce the strength of this systematic review and meta-analysis. There was no standardized tool for measuring risk of bias in observational studies. In this review, we use JBI critical appraisal tool to measure risk of bias.
CONCLUSION
The complication with highest prevalence was axial pain with 21% while hematoma was the lowest prevalence with 2%. However, there was high heterogeneity between studies in this meta-analysis so the result should be interpreted with caution.
REFERENCES
1. Mullin J, Shedid D, and Benzel E. Overview of Cervical Spondylosis Pathophysiology and Biomechanics. WScJ. 2011; 2: 89-97.
3. Steinmetz MP and Resnick DK. Cervical laminoplasty. The Spine Journal. 2006; 6: 274-281.