Randomized Evaluation of Advantages of IT-Based Clinical Pathways in Surgical Treatment of Spondylodiscitis
- 1. Centre for Spinal Cord Injuries, BG-Kliniken Bergmannstrost, Germany
- 2. Department of Neurosurgery, BG-Kliniken Bergmannstrost, Germany
- 3. Department of Trauma, Friedrich Schiller University, Germany
- 4. Department of Orthopedic and Trauma, Asklepios Clinic Weißenfels, Germany
Abstract
Purpose: Clinical pathways as a tool to organize surgical, interventional or conservative therapies are more and more accepted in the German health care system. Does an IT-based clinical pathway offer advantages in the severity based surgical therapy of spondylodiscitis?
Methods: Based on three severity grades of spondylodiscitis an IT-based working tool has been included in the hospital IT-system. From 01/01/2012 to 12/31/2013 32 patients with spondylodiscitis were randomized at admission and prospectively analysed regarding duration and costs of treatment, pain level and inflammatory markers.
Results: Of the 32 patients treated for spondylodiscitis, who had not been transferred from another facility, 17 (53%) were treated according to a clinical pathway on the basis of three well-established treatment regimens depending on severity. The SponDT, as a parameter for the course of disease, was initially slightly higher in the pathway patient‘s group (6.82), than in the control group (6.2). Compared to the control group (n=15) there were differences in the total duration of stay (17.2 vs. 26.0) and the number of taken blood samples (7 vs.10). No differences could be shown for the extent of documentation, the physical and neurological outcome, and the level of pain and the course of inflammatory markers. The most prevalent germ was Staphylococcus aureus (18.8%). In 43.8% no infectious agent could be detected. Material costs and personnel-costs were significantly reduced in the pathway group (12.076 €) compared to 21.341€ in the control group
Conclusion: An IT-based clinical pathway is routinely applicable for the surgical therapy of spondylodiscitis based on three grades of severity and offers various advantages as a clinical and administrative regulative mechanism. Particularly the cost-effective treatment stands out.
Keywords
Spondylodiscitis , Scoring system , Classification of severity , Clinical pathway
CITATION
Homagk N, Jarmuzek T, Meisel HJ, Hofmann GO, Homagk L (2016) Randomized Evaluation of Advantages of IT-Based Clinical Pathways in Surgical Treatment of Spondylodiscitis. JSM Spine 1(1): 1002.
INTRODUCTION
Clinical pathways give a detailed description of necessary procedures in diagnostic and therapy and are established in hospitals more and more frequently [1,2]. This kind of process optimisation leads to a better patient contentment and increases transparency and comparability of treatment [3,4]. Furthermore, clinical pathways can prevent unnecessary procedures and can be used to plan the budget. Clinical pathways are initiated on admission of the patient and pursued until discharge. When developing a clinical pathway, ways of internal workflow have to be analysed and criteria for in- and exclusion or for a necessary switch to an alternative pathway need to be defined. Hence, a pathway is a tool which envelops occupational and work groups [2]. Furthermore, they are useful for collection and evaluation of qualitative and economic data, which can be used for optimisation of processes [5]. In our hospital of maximum care IT-supported clinical pathways are established since 2009 for numerous surgical, traumatological and endoprothetic treatments, with a focus on optimization of processes and documentation [6].
Spondylodiscitis, an infectious disease of the vertebral bodies, intervertebral discs and adjacent structures, occurs in one of 125.000 people, three times more often in men than in women. The spectrum of the infectious agent is broad, but with a predominance of Staphylococcus aureus [7-9]. In our own group of patients the peak of age was beyond the sixth decade of life. Risk factors are, inter alia, higher age, Diabetes, malnutrition, consuming disease, steroid therapy, immune suppression, rheumatoid diseases, drug abuse and surgical procedures of the spine. The mortality rate is nowadays below 5 percent [7-9]. The pathogenesis of spondylodiscitis is mainly via haematogenous spread, direct inoculation of pathogenic microorganisms during surgery or via continuous spread from an infection of the surrounding soft tissues. The spontaneous spondylodiscitis is caused by haematogenous spread. The main localization of spondylodiscitis is the lumbar spine (60%), followed by the thoracic spine (30%) and cervical spine (10%) [10-12].
Spondylodiscitis usually presents unspecific symptoms such as malaise, low fever, fatigue, varied back pain and weight loss. This causes a delay of the correct diagnosis up to several months [9,11]. Besides taking the past and present medical history, initial diagnostic tools are physical and neurological examination, taking the temperature and blood analysis, followed by diagnostic imaging. Often the exact diagnosis is only possible with the help of a histological examination and the direct verification of the infectious agent [7,13]. When there is a compression of the spinal cord with neurological symptoms and in case of destructive lesions with imminent spinal instability or abscess formation the treatment should be surgically [14,15]. The aim of surgery should be the radical and complete debridement of the whole infectious and necrotic area and to restore the stability of the spine. Depending on the size of the defect, eligible materials for repair are mono- or bicortical pelvic bone grafts or autologous fibula or today more frequently foreign implants like titan cages [8,9,15]. Minimally invasive methods are increasingly put into practice [16-18].
The aim of this study was to show an improvement of treatment quality and documentation by translating the severity based treatment of spondylodiscitis into an IT-based clinical pathway, which determines treatment algorithms and allows a respective evaluation including economic aspects.
MATERIALS AND METHODS
In our institution about 13.500 in patients are treated per year. When developing a clinical pathway for these verifies adapted therapy of spondylodiscitis, we could revert to existing IT routines. All relevant treatment components, starting on admission with medical history and evaluation of risk factors, then diagnostic measures, surgery and after care are implemented in the pathway, also called planning sheet [19]. Medical guide lines and internal standards provide the basic concept. Following the development of the planning sheet, every single process is reviewed and verified by all occupational groups involved for a general consensus. The spondylodiscitis pathway was electronically translated in to the IT-system, which allows intern work stations data protected access [6].
The practical application of the clinical pathway starts with admission of the patient. It then shows, which work steps are completed and which are still to be carried out by whom (Figure 1).
Figure 1 Page1ClinicalPathwaySpondylodiscitis (ORBIS, Fa. Agfa).
The implementation of the randomization was done during the admission process. The further therapy with or without pathway was carried out in different departments.
The main users are physicians and nurses. But staff members of other professions such as physiotherapy, anesthesiology, radiology and social service have access to the pathway as well. All treatment steps with the corresponding measures, information and forms are available for the authorized staff. Thus, the following procedures can be used within the pathway:
- taking medical history
- Automatic registration for all necessary procedures (e.g. X-ray, laboratory testing, ECG, surgery, physiotherapy)
- Automatic generation of directions and consultations (e.g. medication, auxiliaries, food orders)
- Integration of all results into the patient’s electronic file - Automatic generation of the patient’s medical record
- Documentation for quality assurance
- Documentation of daily round and pain level
Further relevant data for all these procedures are available as well [6]. The documentation of pain level is also realized within the hospitals IT-system on the basis of the numeric rating scale (NRS), ranking from 0=no pain to10=Imaginable [19]. The cost-cost-analyses is used in this study compares the treatment with and without pathways assuming an equivalent medical outcome [20]. For the compared groups all costs are recorded regarding cost centre and cost element. This is followed by a cost-effectiveness analysis [21]. The advantage of the pathway treatment is also described by additional criteria, which are defined in medical and therefore non-monetary values. Additionally, the SponDT as a course monitoring tool was developed [15]. It summarizes the clinical; Para clinical and morphological extend of spondylodiscitis (Table 1).
|
Table 1: Spondylodiscitis scoring system for diagnosis and therapy control using Spon DT [15].
|
||||
|
Score value |
0 |
1 |
2 |
3 |
|
CRP(mg/dl) |
<10 |
11-50 |
51-150 |
>150 |
|
Pain(NRS) |
<3 |
3–5 |
6–8 |
>8 |
|
MRI |
none/residuals |
discitis |
spondylodiscitis |
Spondylodiscitis with abcess |
According to the SponDT score value and the Spondylodiscitis severity code the grades of severity could be determined. The classification of severity resulted in respective therapies such as non-operative or minimal invasive internal dorsal fixation in grade one. The two- stage ventral repair of thoracic or lumbar spine incase of instability or failure of fusion in grade 2 and the spinal decompression with early ventral repair in grade3 (Table 2).
|
Table 2: Spondylodiscitis severity code (SSC) [15]. |
|||
|
SSC |
Spon DT |
Neurological deficit? |
Destruction? |
|
Grade 1 |
< 3 |
No |
No |
|
Grade 2 |
3–6 |
No |
Yes |
|
|
|
Yes |
|
Statistics was done by the Kruskal-Wall is test as a statistical test for differences in the central tendency of rank data with more than 2 groups. Paired comparisons were performed using Turkey’s HSD. For the questions of frequency, the test was performed by Monte Carlo exact test. The correlation questions were answered by Cramer’s Vasa measure of the relationship between two discrete variables.
A positive ethical approval of the University of Jena is existent.
RESULTS
From 01/01/2012 to 12/31/2013 42 patients with spondylodiscitis underwent surgery. Of these, 32 patients could be included in our prospective study, 17 were treated according to an electronic clinical pathway. Criteria for exclusion of 10 patients were transfer to another facility or necessary treatment of co-morbidities.
9 of a total of 14 male patients and 8 of 18 female patients were treated within the pathway group. The average age was 65.9 years. Patients of the pathway group were 65.7 years on average. There were no differences in the prevalence of comorbidities.
For example there were 3 patients with Diabetes mellitus in each group. It took 48.3 days from the first symptom of spondylodiscitis to hospitalisation, for the later pathway patients even medially 51.9 days.
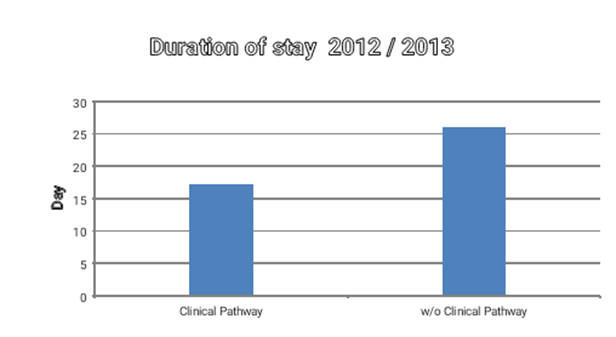
64% of all patients have had no spondylodiscitis-specific treatment at the time of admission. The duration of stay differentiated significantly between pathway treatment (17.2 days) and 26.0 days without pathway (Figure 2).
Figure 2 Duration of stay by subgroups, *=p < 0.05.
Despite thorough diagnostics by means of laboratory testing, biopsy, CT- and MRI scans no origin of spondylodiscitis could be found in 58.1% of all cases.
A previous sepsis was causative in 19.4%, foregone spine surgery in 16.1%, vertebral body fracture in 3.2% and systemic diseases in 3.2%. Predominant germs were Staphylococcus aureus (18.8%), E. coli (12.5%) and Staphylococcus epidermidis (9.4%). Other infectious agents were found in 12.5% and MRSA in 3.1%. Despite a ct-guided or intraoperative biopsy- and/or blood culture rate of 100%, there was no proof of germs in 43.8%. All patients received a calculated or resistogram adjusted antibiotic therapy. Clindamycin was chosen in 43.3%, ciprofloxacin in 20.0%, linezolid in 3.3% other antibiotics in 26.7%and multiple combinations with clindamycin in 6.7%. Application was made at first intravenously and after decrease of inflammatory parameters per os. The most frequent localisation of spondylodiscitis was the lumbar spine in 22 cases, the thoracic spine was affected in 10 cases and the cervical spine in 3 cases. Furthermore there were 3 patients with a multilocular spondylodiscitis.
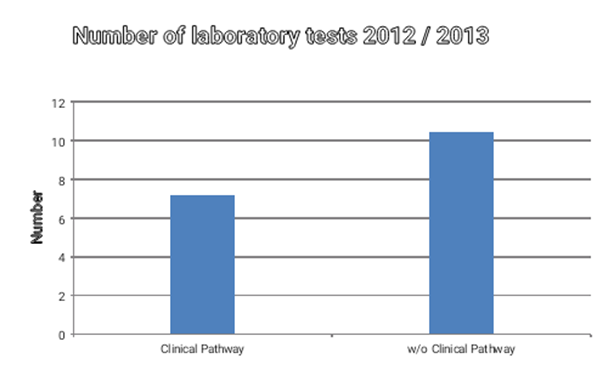
In the period of stay there were no differences regarding the extent of documentation or frequency of blood cultures testing or intraoperative biopsies. Also the point of time of the initiation of further rehabilitative treatment has not been significantly different. The number of laboratory tests in the pathway group was 7.2 examinations per stay, according to the requirements of the planning sheet. Thus, there were significantly less laboratory tests, compared to the group without pathway (Figure 3).
Figure 3 Frequency of lab testing by subgroups, *=p < 0.05.
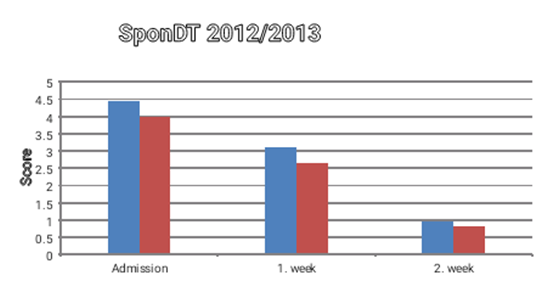
The subjective pain level or the course of inflammatory markers (CRP, white blood count) showed no difference between the two groups. The subjective pain level (NRS) decreased from 6.6 on admission to 3.7 at discharge. The CRP dropped from 118.6 mg/dl to 30.1 mg/dl. It cannot be assumed that pathway patients had been in a better state of health, since the SponDT as parameter for the course of spondylodiscitis was not different, the pathway patients even showed higher values (Figure 4).
Figure 4 SponDT as parameter for the course of spondylodiscitis by subgroups, *=p < 0.05.
Furthermore, the ASA-classification was identical in both groups (2.4). Nevertheless, 4 patients of the non-pathway group did require intensive care after surgery.
The pathway patients underwent surgery 3.4 days after admission; control group patients after 8.8 days.30 patients underwent a dorsal stabilization with an internal fixator. In case of neurological symptoms, which were present in 3 pathway patients and 4 non-pathway patients, we additionally performed a decompression. Two patients, whose cervical spine was affected, initially underwent a ventral approach. Due to instability 7 patients received a two-stage dorso-ventral surgery. In case of a second ventral stabilisation, the point of time varied between 31.5 and 37.5 days. 75% of the patients were treated according to severity grade 1 and 25% according to grade 2.
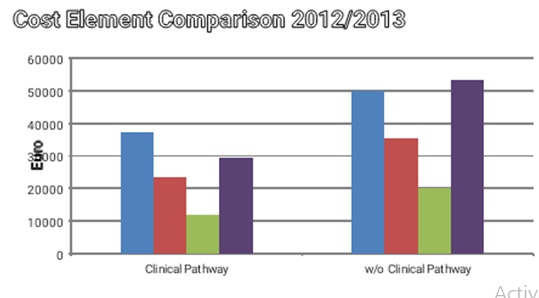
Within the cost-effectiveness analysis the following types of costs were compared:
• personnel expenses for medical staff (physicians and nurses)
• employees of medical and functional service,
• material costs for drugs, implants, other medical requirements,
• personnel and non-personnel costs of the medical infrastructure (e.g. maintenance and repair, nursing management, pharmacy),
• non-medical infrastructure (e.g. building expenses, accommodation and energy costs, costs for insurances and administration)
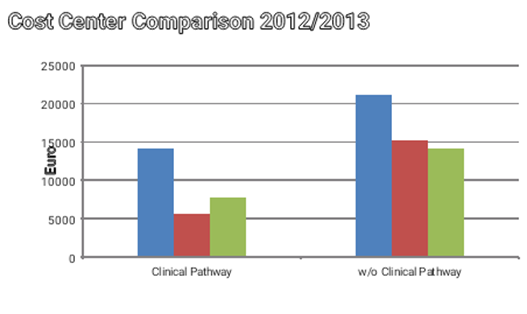
The group of pathway patients showed a significant cost reduction in the area of personnel expenses (Figure 5).
Figure 5 Cost Center Comparison by subgroups, *=p < 0.05.
Cost Element Comparison by subgroups, *=p<0.05, Legend: 2- PK-PFLD medical staff costs
3- PK-MTD /FD personnel costs of medical and functional service
7- PK / SK-MISpersonnel and material costs of medical infrastructure 8- PK / SK-NMIS personnel and material costs not medical infrastructure
Moreover, there were significantly higher costs for an aesthesiological services and laboratory testing as well as additional diagnostics when treated without pathway (Figure 6).
From the economic point of view it remains to be said, that a treatment of spondylodiscitis according to an IT-based pathway results in a total surplus of 11.529 €. Without pathway the surplus is reduced to 8.705€. The economic condition and increase of quality can be described by the Incremental Cost-Effectiveness Ratio (ICER) based on clinical parameters. This is an important parameter for the result of a cost-effectiveness analysis, which defines the differences in expenses and outcomes of both alternatives. Here, it shows for non-monetary parameters, such as the duration of stay and subjective pain perception, a positive value when treated according to the pathway.
DISCUSSION
The implementation of IT-based pathways for the surgical therapy of spondylodiscitis has been widely accepted among nurses and physicians and is now established as a common tool in the medical care routine [4]. However, the study situation in the German-speaking area is of a modest quantity, compared to the Anglo-American region and the effect of IT-based pathways on process and treatment quality remains underrepresented in literature [22]. An optimization of treatment quality by the use of clinical pathways remains scarcely scientifically proven, since most studies concentrate on economic aspects, resulting in a costreduction by the use of pathways for both simple and complex procedures [6,23-25].Clinical pathways are more frequently established for standardised treatment regimens [19]. The complex surgical treatment of spondylodiscitis is often based on certain treatment strategies, which are very variable [15,24,26]. The main focus of this study was the implementation of an ITbased pathway for the surgical treatment of spondylodicitis including the analysis of quality and economic aspects.
For the complex therapy of spondylodiscitis, consisting of diagnosis, surgery, antibiotic treatment, regular follow-ups and physiotherapeutic measures, a structured approach is advisable [24,25]. Often the clinical picture of spondylodiscitis is quite heterogeneous and the patients impairment disparate, even with symptoms of paraplegia [27]. For this reason three grades of severity were determined based on current scientific insights and with the help of the SponDT, in preparation of the implementation of the IT-based pathway. These three severity grades are represented by separate pathways, each recommending a differentiated surgical approach. Since the former classification of severity already gave explicit instructions, a further increase of treatment quality by the implementation of pathways was not anticipated [15]
All patients with spondylodiscitis underwent a biopsy and antibiotic treatment according to resistogram, if available, with close documentation of all measures [28]. A shorter duration of stay and less laboratory analyses for the pathway patients, lead to cost reduction without a lower quality of healthcare. The subjective pain perception was unchanged. Also, the more frequent intensive medical care in the comparison group, despite equal ASA-classified patients, indicates an improvement by the pathway [29,30]. The optimization of the treatment is also reflected by the accelerated preoperative diagnostics. IT-based pathways also allow the automatic recording of all relevant treatment parameters [31-33]. However, although they offer obvious advantages, IT-based pathways are only reluctantly accepted for daily routine. Our own experience shows the necessity of a high level of cooperation and understanding between software developers and medical staff [6, 19].
From the economic point of view a hospital needs to operate cost-covering. A general calculation of costs or proceeds based on the number of cases is not helpful, since every case is brought to account differentially, which has been considered by this study. There, it turned out, that a longer duration of stay leads to distinctly higher personnel costs, which cannot be entirely taken into account by the DRG reimbursement system. The same circumstance applies to the additional laboratory testing’s and diagnostic measures. This shows the economic advantage of electronic based pathways, which enable a sufficient evaluation and optimization of operational processes [6,19].
In this study the ICER was positive for the level of pain, the documentation of treatment and the duration of stay for the pathway group. The higher the ICER the more efficient is the alternative treatment compared to standard therapy [34]. Nevertheless, the statement of a study should not result from an ICER-value alone, but should also be seen in the context of other evaluative methods of health economy such the costcost- or cost-efficiency-analysis mentioned above [35]. Even so, this study shows the advantage of IT-based clinical pathways, which are eligible for routine use and are established as clinical and administrative management tool [6,19]. It has to be noted, that the personnel and temporal expenditure for the pathway implementation itself has not been considered [36].
Because of the inhomogeneous patient cohort and the large treatment variance there are no coherent therapy guidelines. The current opinion of treating spondylodiscitis is the immobilization of the affected spinal section and antibiotic therapy. Occasionally a standardized treatment is suggested but there is a lack of prospective randomized controlled trials and the evidence level of current treatment recommendations remains low [9,14,15]. Our aim was to establish a manageable standard of care, which combines the advantages of several own concepts, considers economic demands of hospital treatment and takes the current treatment opinion into account. The latter vary greatly depending on the extent of the disease [9,14,15].
An only conservative treatment is possible, in higher levels of severity it should be reserved to high-risk patients [9,14,15]. Relevant literature shows that surgically treated patients can expect a better quality of life and a higher level of patient satisfaction since they pass through a shorter period of immobilisation and hospitalisation [14,15] and state a lower level of pain. For these reasons a surgical treatment of spondylodiscitis should be favoured [15].
A ventral debridement of the affected segments and their reconstruction was the predominant surgical treatment suggestion for spondylodiscitis. Today also dorso-ventral or only dorsal procedures are established [12,13]. Hence, for severity grade 1 spondylodiscitis without initial bone destruction an only dorsal stabilisation is recommended.
An additional ventral stabilisation should be considered in cases of remarkable bone defects or progressive segmental kyphosis according to severity grade 2 [15]. This is the most common form of therapy, since osteolytic destruction of the vertebral bodies is often found in spondylodiscitis. But a dorso-ventral approach should not be seen as the stand-alone procedure, due to its higher invasiveness, except for the cervical spine. Furthermore there is a higher risk of osseous loosening of the ventral instrumentation in osteoporotic bones [8,14,15]. With the advance of the technical development of ventral stabilisation procedures, the implantation of extraneous materials such as titanium cages or PEEK prevailed [8,15,24]. We observed this development in our own patient collective, so now expandable titanium cages are more frequently used than bone grafts
For the treatment of severity grade 3 spinal decompression is the focus of therapy. Besides an immediate surgical therapy, a swift further treatment in a centre for paraplegia is of decisive importance for the neurologically impaired patient [15,27,28]. The following complex secondary surgical treatment is recommended within a standardized clinical pathway [15]. The recommended antibiotic therapy is diverse in literature. Ground-breaking studies underline the good permeation of bone and intervertebral discs. Depending on microbiological analyses mainly fluoroquinolones, lincosamides and nitroimidazoles are recommended, often combined [7,9,28]. For the avoidance of biofilm and problem germs like MRSA and VRE combinations of daptomycin and rifampicin or teicoplanin and fosfomycin are suggested [9].The recommended duration of antibiotic therapy varies between 2 and 12 weeks [28].The treatment of spondylodiscitis based on clinical pathways can be seen as common consensus with optimal use of resources. By the standardisation of essential treatment steps the quality and documentation of therapy can be increased significantly [6].The SponDT is useful for diagnosing and following-up spondylodiscitis. Together with the SSC it can be implemented in an IT-based clinical pathway.
SUMMARY
Clinical pathways are a multi-professional consensus on the workflow and documentation when treating a particular disease. As a clinical and administrative management tool it enables the optimal utilization of resources and defines responsibilities. An IT-based form can be implemented in continuation of already existing treatment principles. The previous process and result quality remains unaffected. An economization of the treatment process can be achieved as well as a complete and legally safe documentation in the patient’s electronic health record.
Moreover, transparency is improved, which facilitates the initial training of new staff members, especially in hospitals with a high turnover of employees. Since IT-based pathways are an easy and practical tool for the evaluation of quality and economic efficiency, potential for improvement becomes apparent at an early stage.
For this reason, hospitals should implement IT-based clinical pathways within the hospital information system to optimize treatment processes.