Spinal Dural Arteriovenous Fistulas: A Rare, Insidious Cause of Progressive Myelopathy
- 1. Department of Anatomy, University of Patras, Greece
- 2. Department of Neurosurgery, University Hospital of Patra, Greece
Abstract
Spinal Dural Arteriovenous fistulas (sDAVFs) represent the most common vascular malformation of the spinal cord accounting for 70% of all cases and are very rare in the general population. Usually, sDAVFs present with symptoms and signs of myelopathy and if left untreated can lead to permanent disability. The diagnosis and characterization of sDAVFs requires high index of suspicion and knowledge of the vascular supply and venous drainage of the spinal cord. The present review highlights the most important pathophysiologic characteristics, clinical findings, diagnostic modalities and treatment options available for spinal DAVFs.
Keywords
Spinal Dural Arteriovenous Fistulas; Myelopathy; Spinal cord vasculature.
CITATION
Klironomos G, Gatzounis G (2016) Spinal Dural Arteriovenous Fistulas: A Rare, Insidious Cause of Progressive Myelopathy. JSM Spine 1(1): 1006.
ABBREVIATIONS
Spinal Dural Arteriovenous Fistula (sDAVF); Digital Subtraction Angiography (DSA); Posterior Inferior Cerebellar Artery (PICA)
INTRODUCTION
SDAVFs represent the most common spinal vascular malformations (80% of all spinal malformations) however they are rare pathologies commonly overlooked. Commonly present insidiously and cause disabling neurological symptoms if left untreated. Presenting symptoms are unspecific and an initial assessment with MRI raises the possibility of this diagnosis only in highly preoccupied clinicians. When the diagnosis of sDAVF is considered further MRI/MRA evaluation is needed. The spinal Digital Subtraction Angiography (DSA) still remains the gold standard for the precise anatomic and hemodynamic description of these vascular malformations as well as for the available treatment options evaluation. The deep understanding of the development, pathophysiology and treatment management of spinal DAVFs is based in a thorough understanding of the embryologic development and detailed anatomy of spinal cord vasculature.
Anatomy and Embryology of spinal cord vasculature
The formation of neural tube starts at 22-23rdgestational day and the closure of the rostral and caudal neuropore happens at 25th and 27th day respectively. By the 10th gestational week the initial spinal cord vasculature has been established [1]. Two interconnecting longitudinal collector vessels (venous system) run the spinal cord in the subarachnoid space at its ventral and dorsal surface forming a venous plexus [2]. This plexus communicates with the epidural venous plexus via the valveless bridging veins which either follow the nerve routes, like the arteries always do (radicular veins) or pierce the dura between adjacent nerve routes.
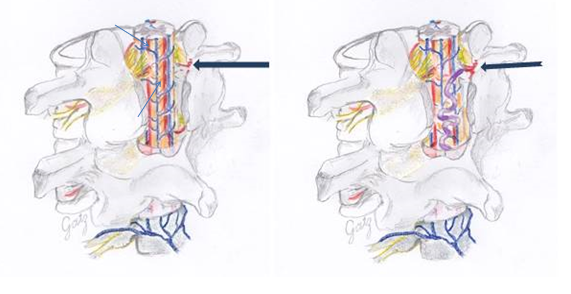
The arterial supply of the spinal cord as seen in adults, comes from the anterior and the paired posterior spinal arteries augmented segmentally by the radiculomedullary and radiculopial arteries [3].The anterior spinal artery originates intracranially from both vertebral arteries and run inside the anterior spinal cord sulcus. The paired posterior spinal arteries originate either from the vertebral arteries or PICA on each side and run on the posterior surface of the spinal cord just medial to the posterior roots. All three arteries travel the whole length of the spinal cord from the foramen magnum to the conus medullaris. The spinal arteries are supplied by the segmental arteries arising from the vertebral and deep cervical arteries at the cervical levels, intercostal at the thoracic levels, lumbar at the lumbar levels and middle sacral, lateral sacral and iliolumbar at the sacral levels. The segmental arteries supply the vertebral bodies and arches, the paraspinal muscles and give off the radicular arteries which enter the intervertebral foramen following the spinal nerve. Each radicular artery gives the radiculo-meningeal artery in all the levels which supply the dura matter and spinal nerve. At some levels the radicular artery provides the anterior and posterior radiculo-medullary arterieswhich follow the anterior and posterior nerve root respectively and reinforce the anterior and posterior spinal arteries and thus participating to the arterial vasculature supplying the spinal cord. Not all segmental arteries give off anterior and posterior radiculomedullary feeders and their location in a particular patient cannot be predicted (Figure 1). The most constant radiculomedullary artery is the radiculomedullary magna or artery of Adamkiewicz which is located on the left side between T8 and L2. The radiculomedullary arteries which travel on the anterior root follow a superior-medial direction, approach the central sulcus and turn inferiorly to reinforce the anterior spinal artery. This route creates a characteristic angiographic configuration resembling a hairpin which is very important, if present, in the treatment decision making.
The intrinsic vascular network of the spinal cord is consisted of central perforating arteries, branches of the anterior spinal artery, supplying the anterior 2/3 of the spinal cord including most of the gray matterup to the base of the posterior horn, the corticospinal and spinothalamic tracts. The posterior 1/3 of the spinal cord is supplied by the posterior spinal arteries. The periphery of the spinal cord and most of the white matter is supplied by the vasocorona consisting of perforating branches of the anterior and paired posterior spinal arteries.
The intrinsic spinal cord veins are arranged in radial fashion and drain to the superficial longitudinal highly anastomosing veins. Transmedullary anastomoses also exist. This perimedullary venous plexus communicates with the epidural and paraspinal venous plexuses via valveless bridging veins and these plexuses finally drain to the azygos/hemiazygos venous systems. The bridging veins follow the nerve roots inside the dura sleeve (radicular bridging veins)or pierce the dura matter in an area between two adjacent nerve roots. This type of anastomosis is not reflux resistant and this is very important in the pathophysiology of myelopathy caused by sDAVFs.
Classification of spinal cord vascular malformations
There are many schemes classifying vascular malformations of the spinal cord based on genetics characteristics and inheritance (Table 1), location of the malformation, flow of the shunt and type of feeding vessels [3].The evolution of imaging and interventional techniques the last decades has dramatically improved our understanding of the pathophysiology of these lesions. This has prompts the development of more accurate classification systems based on anatomic, topographic and pathophysiologic criteria (Table 2), [4,5]. Spinal cord Arteriovenous Malformations (AVMs) are usually fed by intrinsic or pial spinal cord arteries that normally feed neural tissue [6]. They are located inside the spinal cord matter or at the pial surface, are high flow vascular malformation and thus they usually present with intramedullary hemorrhage (type II vascular malformation, also known as “nidus” or ‘glomus” AVMs). Rarely AVMs might be located in the subarachnoid space, epidural space or extended in both intra and extradural compartment (type III vascular malformations). Fistulous-type AVMs (also known as type IV vascular malformation or pial fistulas) are less common. They are fed by pial vessels which directly drain to perimedullary veins without the nidus interposition and commonly located at the conus medullaris and filum terminale area. On the
Figure 1 Left: Normal vascular anatomy of the spinal cord. The radiculomedulary and radiculopial arteries follow the anterior and posterior root respectively (thin arrows). The radiculomeningeal artery supplies the dura at each level (thick arrow). Right: A spinal DAVF developed between the radiculomeningeal artery and the radicular vein (arrow).
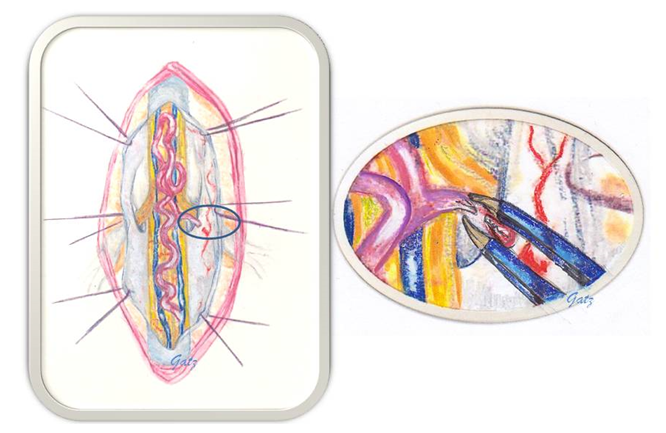
Figure 2 Intradural surgical disconnection of the spinal DAVF.
other hand, sDAVFs represent arteriovenous shunts between radiculomeningeal arteries (correspond to the cranial meningeal arteries) and bridging veins. The shunting zone is usually located dorsally to the root and drain through the radicular bridging veins to the perimedullary venous plexus. This causes reflux to the perimedullary venous plexus, arterialization of the perimedullary veins and congestion of the venous drainage from the spinal cord. The increase in venous pressure causes stasis and spinal cord edema. In chronic, untreated situations ischemia may lead to spinal cord atrophy. In cases of DAVFs located in the epidural space with the shunting zone between a dura artery and a vein usually do not cause myelopathy. In rare cases can cause myelopathy due to blood steel phenomena or due to compression of the spinal cord from varices.
Classification of spinal DAVFs
GeibprasertS et., all in their publication in Stroke 2009 propose a new classification system based on the embryologic development of the dura mater and the surrounding structures into ventral, dorsal and lateral epidural groups [7,8]. The ventral epidural DAVFS drain to veins creating the basilar vertebral venous plexus that normally drain structures derived from the notochord such as vertebral bodies. This plexus
|
Table 1: Classification of vascular malformation based on genetic characteristics. |
|
|
Genetic hereditary |
Compromise of vascular cells at the germinal stage leads to the development ofAVMS, fistulas and telangiectasia. Hereditary hemorrhagic telangiectasia (Osler Weber Rendu syndrome) is a characteristic autosomal dominant disorder. |
|
Genetic non hereditary |
Very early vascular cells compromise in their embryonic evolution leads to multiple shunts development in many organs. May share metameric links (Cobb syndrome). No hereditary pattern. |
|
Single lesions |
Single lesions AVMs or AVFs. No genetic component has been shown. |
|
Table 2: Spinal vascular malformations, Anson-Spetzler’s classification system. |
|
|
Neoplastic vascular lesions |
1. Hemangioblastomas |
|
2. Cavernous malformations |
|
|
Aneurysms |
|
|
Arteriovenous malformation |
Type I. Dural AVF. Most common spinal vascular malformation (70%).Diagnosed predominately in men between 5th and 8th decade. Fistula is located between the radiculo-meningeal artery and the radicular vein usually near the spinal nerve root. Most common location: thoracolumbar spine. Most common presentation is myelopathy due to venous hypertension and spinal cord edema hypo-perfusion and hypoxia. Hemorrhage rarely occurs. |
|
Type II. Glomus or nidus-typed AVMS located inside the spinal cord although superficially located nidus can reach the subarachnoid space. Multiple feeding vessels from the anterior and/or posterior spinal artery supply the AVM. The venous drainage is to the perimedullary venous system. This type represents about 20% of all spinal vascular malformation and the commonest intramedullary located vascular malformation.Commonly located in cervicomedullary junction. Most common in younger patients. Most common presentation is acute neurologic deterioration due to intramedullary hemorrhage |
|
|
Type III. Juvenile arteriovenous malformations.Typically found in young adults and children. Arteriovenous malformations, usually extensive,intradural and or extradural in location fed by multiple vessels. |
|
|
Type IV. Also known as pial AVFs, ventral or perimedulary AVF and areintradural extramedullary malformations located on the spinal cord surface. The fistulous connection is created between a spinal artery and spinal vein on the surface of the spinal cord without nidus creation. There are 3 sub-types: a) small, b) large and c) giant. |
|
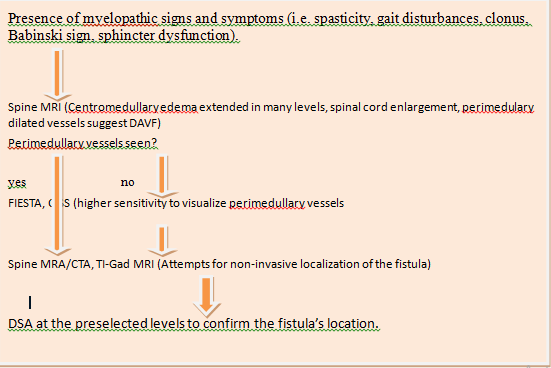
Table 3 Diagnostic algorithm for spinal DAVFs.
communicates with the cavernous sinus cranially. These ventral epidural space DAVFs normally do not cause myelopathy because the veins in this area do not drain spinal cord but bony structures. In rare case when a venous thrombosis happens or in case of high flow shunts perimedullary veins reflux develops and myelopathy symptoms may occur.
The dorsal epidural DAVFs are extremely rare and drain to veins that normally drain the spinous processes and vertebral laminae. They correspond to the cranial DAVFs drain to the superior sagittal and transverse sinus but these vessels aren’t developed in the spinal level. They usually present with spontaneous epidural hematoma and don’t cause myelopathy.
The most common spinal DAVFs belong to the lateral epiduralgroup. The shunting zone is usually located dorsal tothe nerve root and is related to the bridging vein which connects the perimedullary venous plexus to the epidural plexus. These fistulas cause blood reflux to the perimedullary veins, venous hypertension, venous arterialization and spinal cord edema [9]. In chronic, untreated cases the spinal cord ischemia leads to atrophy and permanent neurological deficits.
Epidemiology and clinical presentation of sDAVFs
SDAVFS are the commonest vascular malformation of the spinal cord representing around 80% of all spinal vascular malformation [10]. Usually encounter around 50-60 yo and affect commonly men. They are very uncommon in young ages (1% of sDAVFs cases are seen before 30y.o). The most common location is the thoracolumbar area T6-L2 (>80%), followed by sacral area (5%), upper cervical area (2%) and very rarely lower cervical area. SDAVFs are considered to be acquired lesions and possible etiologic factors are trauma, previous venous thrombosis or previous spine operation.
Initial symptoms are not specific. These may include motor symptoms such as difficulty with climbing stairs and gait disturbances [11,12]. Sensory symptoms like paresthesia, sensory loss and back pain or radicular pain are common. Symptoms indicating autonomic dysfunction like erectile dysfunction, inadequate bladder control and fecal incontinence may occur late in the course of the disease. In some cases symptoms of upper and lower motor neuron dysfunction may coexist in the same patient resembling amyotrophic lateral sclerosis and the presence of disturbed sensory function is critical for the differential diagnosis. Many patients with sDAVFs present with conus medullaris symptomatology even if the fistula is located in higher level. This probably happens because the thoracolumbar area harbors relatively less bridging veins and also due to the rostro-caudal movement of the spinal cord edema. Often the symptomatology of DAVFs is very insidiously progressing and if left untreated permanent neurological deficits establish. Hemorrhage is not common in sDAVFs and its presence should raise suspicion for the existence of an AVM.
Radiologic characteristics of spinal DAVFs
See Table 3 for a diagnostic algorithm. The diagnosis of spinal DAVFs requires high index of suspicion and MRI T2WI, and T1-Gad are the initial choice for radiologic evaluation. The combination of centromedullary, not well defined hyperintensity on T2, extended in many levels, accompanied by spinal cord enlargement and perimedullary enlarged vessels is indicative of sDAVF. The centromedullaryhyperintensity on T2 represents edema and is often accompanied by a rim of hypointensity which probably represents deoxygenated hemoglobin due to venous congestion and hypoxia[13-16]. T1WI with Gad shows enhancement in chronic disease due to spinal cord-blood barrier breakdown which may be accompanied by spinal cord atrophy. The dilated tortuous perimedullary vessels appear as flow voids in T2. Contrast enhanced T1 or heavily weighted T2 sequences such as fast imaging employing steady state acquisition (FIESTA) or constructive interference in steady state (CISS) display higher sensitivity in revealing perimedullary vessels and may be useful in early disease or in case of low flow shunts [17]. The establishment of the presence of spinal DAVF on MRI is followed by attempts to localize the fistula. Neither the spinal cord edema nor the location of dilated vessels correlates with the location of the shunt. The localization of the shunt may be challenging. Selective DSA is necessary to confirm the site of the fistula and to evaluate the treatment options. Because of the high dose of radiation and increased amount of iodine contrast exposed, noninvasive techniques to localize the fistula and restrict the need of selective catheterization in specific levels could be very useful in the diagnostic algorithm of spinal DAVFs. Contrast enhanced MRA is helpful in localizing the shunt and can direct the selective angiography to specific levels in order to confirm the diagnosis. The first passage gadolinium enhanced MRA technique can demonstrate early vein confirming the presence of the shunt and in most cases indicatesits site [18-21].
Treatment
The aim of the treatment is the occlusion of the shunt which is achieved by the distal occlusion of all the arterial feeders and the proximal part of the draining vein. There are two treatments modalities available for sDAVFs: The surgical disconnection and the embolization of the fistula [22-26]. The surgical treatment aims to the identification and disconnection of the vein draining the fistula (Figure 2). It is relatively safe procedure and its success rate is very high achieving complete occlusion in 98% of cases. The endovascular treatment aims to embolization with liquid material of both the feeding arteries branches of the radiculomeningeal artery and the proximal segment of the draining vein. Failure to pass the embolic material to the draining vein can cause early recanalization due to the development of new collaterals feeders. The success rate of endovascular treatment varies between 25-75% [27]. Incomplete occlusion or inadequate passage of the embolic agent into the draining vein increases the risk of early recanalization and clinical deterioration [28,29]. In these cases early surgical intervention is recommended. Endovascular treatment is contraindicated if the angiogram reveals the presence of a radicullomedulary artery at the same level with the fistula. This situation increase dramatically the risk of spinal cord infract with devastating consequences as the embolic agent may occlude the raidiculomedulary artery. Some centers avoid endovascular treatment in cases where an anterior perimedullary artery arises from an adjacent or contralateral intervertebral foramen. Surgical treatment is the treatment of choice in these cases.
Prognosis
The duration of the disease and the clinical situation before treatment usually determine the prognosis. Disconnection of the fistula results in hold of the disease’s progression. Post-treatment clinical improvement depends on the type of presenting symptoms: two thirds of the patients with motor symptoms (spasticity, gait difficulties) display improvement in some extent but only one third of patients with sensory symptoms show improvement. Pain may persist for a long time after treatment. Symptoms indicating autonomic dysfunction such as urinary and fecal incontinence, erectile dysfunction have the smallest chances to improve. Patients with longstanding disease display poor outcome [30].
CONCLUSIONS
Myelopathy caused by spinal DAVFs is a rare disease. Highindex is required by the clinicians and the radiologists in order to include tis entity in the deferential diagnostic list of myelopathies. Early identification of the DAVF, using all the available diagnostic modalities, is critical. Prompted therapeutic intervention can stop the myelopathy progression, reverse the neurologic symptomatology and result in the avoidance of devastating neurologic consequences.
ACKNOWLEDGES
To Anna Gatzounis for her contribution in figures drawing.