Surgical Treatment for Fused Vertebrae Deformity after Old Cervical Spine Fracture Subluxation: A Case Report and Review of the Literature
- 1. Department of Orthopedics, (Division of Spinal Surgery), Zaozhuang mining group central hospital, China
Abstract
Introduction: Fusion deformity of cervical vertebrae resulted from trauma is a rarely reported condition in the literatures. Fewer than 3 case reports have been made. This case represents the first reported case, to our knowledge, of fusion deformity of cervical vertebrae caused after old cervical spine fracture subluxation.
Presentation of case: We present the case of a 44-year-old woman with a history of falling down from the roof of the house and injuring the neck seven years ago, she had a severe pain of the neck, but there was no sensory and motor dysfunction of upper and lower extremities, she stayed home in the bed and rest for 3 months without surgery, but she often complaining about bilateral hands tingling and unsteady for recent one year.
Discussion: Literature review of previously reported cases of fusion deformity of cervical vertebrae resulted from trauma revealed only 2 cases. Anterior approach surgery can eliminate compression factors directly, and it can obtain the excellent effects of the clinical decompression nevertheless, prevention is the most important.
Conclusion: Delayed neurological deficit resulting from fused vertebrae deformity following irreducible old cervical spine fracture subluxation is an extremely rare complication. Instability of cervical spine is the essential and foremost pathogenic factors, and then, leads and aggravates the degeneration of the adjacent segments. We emphasize the importance that finding deformity and instability early and taking effective surgical treatment in a timely manner.
Keywords
Surgery; kyphosis deformity; Fracture, Subluxation; Cervical vertebrae.
CITATION
Xia Q, Sun JM (2017) Surgical Treatment for Fused Vertebrae Deformity after Old Cervical Spine Fracture Subluxation: A Case Report and Review of the Literature. JSM Spine 2(1): 1013.
INTRODUCTION
Fusion deformity of cervical vertebrae resulted from trauma was rarely reported in the literatures, because cervical spine fracture- subluxations often should be obtained reduction and fixation in time. Hereinafter, we present a case of fused vertebrae deformity after old cervical spine fracture subluxation, we also describe the clinical characters and treatment outcomes, and discuss the clinical pathogenic mechanisms and surgical methods and review relevant literatures [1].
CASE REPORT
History and presentation
A 44-year-old woman complaining about bilateral hands tingling and unsteady gait was admitted to the spinal surgical department in our hospital. Seven years ago, she fell down from the roof of the house about 3 meters high and her neck knocked on the ground, at that moment she had a severe pain of the neck, but there was no sensory and motor dysfunction of upper and lower extremities, So she refused to be under treatment in hospital, and preferred to choose to stay home in the bed and rest for 3 months, then walked gradually, but she had often complained about bilateral shoulder girdles pain and neck stiffness, and developed gradually to the bilateral elbows and hands. 1 year ago, she began to had tingling in the bilateral hands, and the tingling in the bilateral ring and little finger were most severely. In latest two months, her tingling deteriorated, and developed numbness and formication on the bilateral hands, bilateral lower extremities couldn’t cross-stand and clumsiness while walking because of accessible to fall down. she denied difficulty in urination and defecation.
Examination
Physical examination showed that she had positive Spurling sign and Eaton test, and when the bilateral upper extremities abducting and stretching beyond the head, her tingling in the hands would relieve instantly, however a few minutes later, the tingling symptom in the hands was sharpened once again,according with symptom of cervical spondylosis radiculopathy. Sensory disturbance was located in the bilateral hands, especially in the medial aspects of the hands, including the medial one and one half finger, and she had positive Hoffmann sign and negative Babinski sign, conform to symptom of cervical spondylosis myelopathy. There were no significant changes about muscle strength and tension.
Imaging
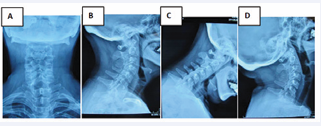
The patient underwent radiologic evaluation via plain cervical spine radiographs (posterior- anterior, lateral and dynamic flexion-extension views), cervical spine CT scans and 3-dimension reconstruction and magnetic resonance imaging. The posterior anterior and the lateral radiography can be obtained by traction on arms. Radiography of the patient showed C7/T1 bilateral facets luxation, spinal process intervertebral was bigger, and local kyphosis deformity. Dynamic plain radiographs demonstrated C6/C7/T1 deformity was fixed, and the change of C5/C6 intervertebral body angle was approximately 15° indicating that C5/C6 vertebrae were unsteady (Figure 1A-D).
Figure 1: Radiography disclosing C6/C7/T1 fixed fusion and kyphosis deformity. A: poster anterior radiography showing C7/T1 spinous process intervals enlarging and bilateral C7/T1 facet subluxation; B: lateral radiography demonstrating anterior cervical fusion (C6/C7/T1) and C7/T1 spinous process intervals enlarging; C D: flexion extension radiography demonstrating C6/7/T1 rigidity and C5/6 instability.
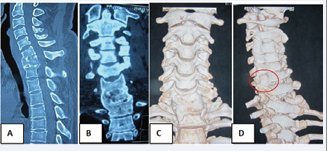
Sagittal and coronal computed tomography (CT) reconstruction scans of her neck revealed that C6/C6/T1 vertebral body were fused completely and formed local kyphosis deformity with the angle of the Cobb about 30° . Posterior wall of the C7/T1 intervertebral body took into angular kyphosis shape and resulted to cervical spine stenosis. 3-dimension CT reconstruction of the cervical spine shows bilateral facets of the C7/T1 was subluxated, and the bilateral lower facets of C7 displaced upward (Figure 2A-D).
Figure 2: CT scans and 3-dimension reconstructions of the cervical spine. AB:sagittal and coronal CT reconstruction demonstrating C6/C7/T1 vertebral body fusion and C7/T1 posterior junction projecting; CD: anterior view of 3-dimension reconstructions demonstrating C6/C7/T1 intervertebral body and normal C6-C7 vertebral body configuration disappeared, lateral view of 3-dimension reconstructions demonstrating bilateral C7/T1 facet subluxation.
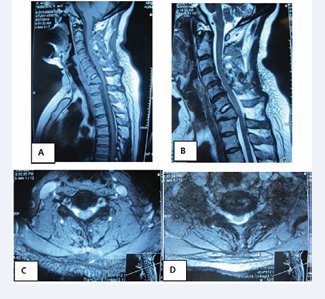
A magnetic resonance imaging displayed a focal spinal cord compression at C7-T1 level due to spinal stenosis resulted from kyphosis deformity, and there was a severe compression at C5-C6 level because of disc herniation. The entire cervical disc displaced varying degrees of degeneration on the T2WI (Figure 3A-D).
Figure 3: MRI imaging studies obtained in the illustrative case. A B: preoperative sagittal MRI (T1-weighted and T2-weighted) demonstrating fixed kyphosis deformity, C6/7 and C7/T1 disc variation and degeneration, and C7/ T1 disc herniation and posterior junction projecting; C: axial MRI (C5/6 level) demonstrating extruded disc herniation; D: axial MRI (C7/T1 level) projected sclerotic.
Operation
The surgery was performed via anterior approach to the cervical spine. The patient was carefully placed to the supine position on the operating table with a small sandbag between the shoulder blades to ensure extension of the neck after successful general anesthesia, and localize the lower cervical spine levels. The patient could then be prepped and draped in the standard fashion.
A standard transverse skin crease incision at the appropriate 1 transverse finger level above the right clavicle, such an incision has an extreme cosmetic advantage. Identify the anterior border of sternomastoid muscle, cutting the omohyoid, and gently separate carotid sheath and visceral sheath using the fingers while protecting recurrent laryngeal nerve, trachea, and esophagus. Using cautery, split the longus colli muscle longitudinally over the midline of the vertebral body that need to be exposed, then dissect the muscle subperiosteally with the anterior longitudinal ligament and retract each portion laterally to expose the anterior surface of C5-T1 vertebral body. After identifying and exploring the level correctly with a needle marker, we carried out sub-total resection of the C7 vertebral body with abrasive drilling and Kerrison rongeur, managing the cartilage endplates and undermining decompression of the posterior inferior part of C6 vertebral body and the posterior upward part of T1 vertebral body. Then accomplish discectomy of C5/6, and prepare the adjacent cartilage endplates using the same way. Finally, Cage and titanium mesh combining with the allograft bone were placed in the corresponding vertebral body clearance, and the anterior cervical plate and screws were used at C5 and T1 vertebral body under the C-arm guidance. During the entire procedure, the retractors were intermittently released to avoid damaging of the recurrent laryngeal nerve, trachea, and esophagus. Routine closure was carried out and drains were left.
Postoperative course
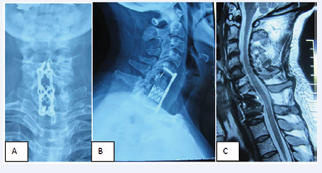
The patient was immobilized in Philadelphia cervical collar during the 3 months of the post operation. Plain cervical spine radiography and magnetic resonance imaging evaluation were done at postoperative 1 week (Figure 4A-C).
Figure 4: Imaging of post operation. A B: poster anterior and lateral radiography showing the placement of plate, screws, cage, and titanic mesh was quietly suitable; C: magnetic resonance imaging showing cervical canal decompression was excellent.
In this case, the patient obtained immediate postoperative relief of his tingling in the bilateral hand, but numbness of the right hand existed. She could cross-stand and her gait subsequently normalized. Her neurological examination at the 3-month followup revealed no sensory or motor deficit, and the solid bone fusion was confirmed.
DISCUSSION
Lower cervical spine fracture-subluxations were usually associated with neurological deficits, so they could be timely and effectively treated with surgical treatment [1,3,5,6,7]. Lower cervical spine fracture-subluxation untreated were extremely rare, and the fusion deformity of cervical vertebrae resulted from Lower cervical spine fracture-subluxations and their outcomes were rarely reported as far as we know [3,5,6].
Before, lower cervical spine fracture-subluxation, especially C7, is extremely liable to be misdiagnosed because of sheltering from superimposition of shoulders, if there were no neurological deficits [3,4,6,7]. The patient in this report stayed in home rather than hospital after she had fallen down from the roof of the house, because she had only neck and shoulder pain without numbness and weakness of the extremities, especially her poverty. After many years, she had to inquire with doctors for the sensory and motor abnormality of the extremities resulted from cervical canal stenosis. In our department, we also have a case of 47-year-old female with fused vertebral deformity after 17 years untreated C5/C6 fracture-subluxation, she was admitted in hospital because of complaining of the numbness of the right extremities for 1 month, unfortunately she denied surgery and auto-discharged. Srivastava et al. [1], present a case of a middle aged male who developed a bilateral facet dislocation but only sought treatment 14 months post injury when he experienced pain and deformity in the cervical spine, Computed tomography and MRI demonstrated a fused (bony) bilateral facet dislocation at C4/5, a cervical spine reconstruction consisting of a posterior-anterior-posterior approach was performed to address both the deformity and the pain, at 32-month follow-up, the patient remains well with no neurological symptoms, minimal neck pain and successful fusion. Yamazaki et al. [2], report that a 56-year-old man was diagnosed with an irreducible fracture dislocation at the C6-C7 level 2 months after a motor vehicle accident, He showed torticollis, and complained of severe pain in his neck and left upper arm, radiographic examinations revealed that the C6 vertebra was translated anteriorly and laterally to the C7 vertebra, and a bony union had progressed at the fracture site, showing rigid cervicothoracic kyphoscoliosis. (Table 1)
Table 1: Characteristic data of the patients. |
|||||||
authors |
Characters |
||||||
gender |
age |
history |
Traumatic segment |
cause |
Clinical manifestation |
Surgical protocol |
|
Xia |
F |
44 |
7 years |
C7/T1 |
Falling accident |
Tingling and numbness of bilateral hands, weak of bilateral lower extremity |
Decompression via anterior approach |
Srivastava |
F |
42 |
14 months |
C4/C5 |
Falling accident |
Pain of neck |
cervical spine reconstruction consisting of a posterior-anterior-posterior approach |
Yamazaki |
M |
56 |
2 months |
C6/C7 |
motor vehicle accident |
Pain of Neck and left upper arm |
circumferential corrective osteotomy at the C6-C7 level |
The causes of fused vertebrae deformity, we think, were instability of the cervical spine of post-trauma, and the patient also failed to come for his follow-up visits. Cervical spine fractures and/or facet joints subluxation must lead to instability of the focal part of the cervical spine, and the instability would result in bone hyperplasia and bone drop formation, at the end, adjacent vertebral bodies and facet joints gave rise to circumferential bony fusion around the deformity [6,8,9]. C6-C7-T1 fusion of the patient we presented arose basing on this cause. But beyond that, maintain contact and tender moving were essential factors for vertebrae fusion, because in the circumstances of the opposite status, pseudo arthrosis proned to come into being. This is why fused vertebra developed in the flexion-compression of sub axial cervical spine, however dislocation of the upper cervical spine, for instance, old odontoid process fracture associated with atlantoaxial dislocation, rarely presented bony fusion even after many years. We encountered a case of mid ages female with old odontoid process fracture associated with atlantoaxial dislocation, she still displays atlantoaxial instability and dislocation after 30 years .
As soon as the fused vertebra deformities form, it will bring about and exacerbate degeneration of the adjacent segments because of the change of stress. Adjacent disc of the patient in this paper had significant signal changes and herniation in the imaging of MRI (Figure 3). And the patient had numbness of radial part of the bilateral hands, according to the damage of the C6 nerve roots. In the operation, we handled C5/6 disc together, and the numbness of the hands disappeared immediately postoperation. So fixed kyphosis deformity should be corrected in theory, otherwise it will bring about a series of problems [1,5,8,9].
Is it necessary to correct about the fixed or rigid kyphosis deformity one stage when the cervical canal was decompressed on earth? Just as mention hereinbefore, fixed kyphosis deformity is easier to give rise to the degeneration of adjacent segments, in theory, correction surgery should be carried out. This is involves in anterior approach, posterior approach and anteriorposterior approach surgery. According to the theory we known, only total resection or sub-total resection of the apical vertebral body, the posterior borders of the adjacent vertebral body will become a new compressive factors of the spinal cord and the nerve roots, therefore, the effects of decompression are limited or unthoroughly via anterior approach surgery alone. Because the compressive factors of rigid kyphosis deformity are located in the front of the spinal cord and nerve roots, posterior approach correction surgery alone is very complicated and challenging. If cut open bilateral facet joints with abrasive drilling via posterior approach surgery firstly, and then perform anterior approach surgery, cervical spine may obtain excellent deformity correction theoretically, but during the actual operation, deformity correction need to complete via anterior distraction and posterior compression, this manipulation is difficult to come true during the changing of the surgical position. In theory, anterior approach surgery can eliminate compression factors directly, and there are a lot of advantages, for example, simple manipulation and thorough compression. So how is the effect of anterior compression alone on earth? The case we presented proved effectiveness of the anterior approach surgery by means of postoperative MRI imaging and clinical outcome. MRI demonstrated postoperative cervical spine sequence excellent and compression factors of circumference of spinal cord was disappeared (Figure 4A-C). We analyze that the cobb angles of the posttraumatic kyphosis deformity of the lower cervical spine tends to be lesser, not exceeding 45 degrees generally, and not angular kyphosis, as a consequence, we reckon that the treatment of kyphosis deformity resulted from fused vertebra accomplish merely through anterior approach surgery [9].
CONCLUSION
Delayed neurological deficit resulting from fused vertebrae deformity following irreducible old cervical spine fracturesubluxation is an extremely rare complication, and commonly seen in the lower cervical spines. Instability of cervical spine is the essential and foremost pathogenic factors, and then, lead to and aggravate the degeneration of the adjacent segments. Anterior approach surgery can eliminate compression factors directly, and it can obtain the excellent effects of the clinical decompression. But anyway, prevention is the most important, we emphasize the importance that finding potential trauma and instability early and taking effective surgical treatment in a timely manner.