Dual Loop Reconstruction after Pancreaticoduodenectomy for a Previous Roux-En-Y Biliodigestive Anastomosis: A Case Report
- 1. Department of radiology, Mahmoud El Matri Hospital, Ariana, Tunisia
INTRODUCTION
Reconstruction modalities after pancreaticoduodenectomy is still debated since pancreatic fistula constituted the main reason for mortality and morbidity [1]. Deliberate dual loop reconstruction was chosen in order to reduce the consequences of pancreatic fistula by separating the pancreaticojejunostomy from hepaticojejunostomy and gastrojejunostomy [2, 3]. It was used in other cases separating pancreaticojejunostomy and hepaticojejunostomy from gastrojejunostomy to avoid gastric emptying disorders leading to pancreaticojejunostomy fistula by high pressure [4]. Sometimes, as in our case, this type of reconstruction wasn’t deliberate but implied by a previous Rouxen-Y biliodigestive anastomosis. The work has been reported in line with SCARE criteria [5].
PATIENT AND OBSERVATION
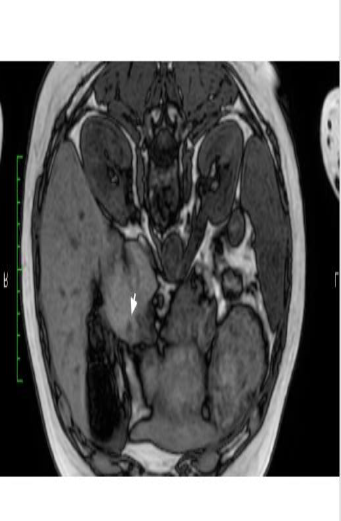
A 62-year-old woman presented to the outpatient department for epigastria pain lasting for two months. She had a laparoscopic cholecystectomy for symptomatic cholelithiasis 20 years ago. She was operated on for breast cancer four years ago. She had a Roux-en-Y biliodigestive anastomosis via right subcostal incision three years ago for a main bile duct cyst type Ib. No pancreaticnodule was shown in the performed biliary magnetic resonance imaging. The anatomopathological exam concluded to the absence of malignancy. Physical examination was normal. The CA19-9 level was within normal range. Computed tomography didn’t reveal any abnormalities. Magnetic resonance imaging revealed a hyperintense mass of 1cm in diameter, localized in the pancreatic head (Figure 1). In order to determine the nature of this pancreatic nodule, an endoscopic ultrasound with biopsies was done. The anatomopathological exam concluded to acinar adenocarcinoma. Hence, a pancreaticoduodenectomy was indicated for a resect able non metastatic pancreatic adenocarcinoma. Since a biliodigestive anastomosis was already done, the multidisciplinary consultation meeting recommended a dual loop reconstruction with an isolated pancreaticojejunostomy. This procedure was performed via a bucket-handle incision. The postoperative course was uneventful especially no pancreatic fistula or gastric emptying disorder. The anatomopathological exam showed a well-differentiated pancreatic adenocarcinoma, localized at a distance from the papilla and the wirsung canal. All the margins were safe. It was classified pT1CN0. No relapse was observed after six months.
Fig 1: Magnetic resonance imaging showing a hypo-intense nodule at the pancreatic head (White arrow).
DISCUSSION
Our case illustrated a rare case of implied dual reconstruction by a previous Roux-en-Y biliodigestive anastomosis. At one hand, undo and redo a new hepaticojejunostomy in order to have a conventional reconstruction manner could have been challenging since the first procedure was performed nearby the superior biliary convergence roof. At the other hand, dual loop reconstruction with isolated pancreaticojejunostomy allowed to reduce the consequences of pancreatic fistula and to reduce the gastric emptying disorder leading to pancreatic fistula [2-4]. Avoiding the mixing of pancreatic secretions with bilio-intestinal content reduced pancreatic biliary reflux and hence minimizing pancreatic fistula consequences even though the fistula rate wasn’t significantly diminished [2]. The superiority of dual loop reconstruction in comparison with single loop reconstruction wasn’t proved with a strong recommendation grade A [6, 7]. That’s why well-conducted trials are still needed to prove either equivalence or non-inferiority reconstruction.
CONCLUSION
Reconstruction modalities after pancreaticoduodenectomy are still controversial with no consensus. Dual loop reconstruction could be implied in some particular cases. Further trials are needed to clarify the place of each technique in order to embitter the prognosis.
ACKNOWLEDGEMENTS
For all authors, no COI/Disclosure and Funding/Support to declare. I have received no funding for this study.
PATIENT CONSENT
A writing informed consent was obtained from the patient to public this report in accordance with the journal’s patient consent policy.
REFERENCES
- Adekoya P, Obirieze A, Onwugbufor M, Cole M, Cornwell EE, Frederick WA. The impact of complications after pancreaticoduodenectomy in elderly patients: a review of the nationwide inpatient sample database. Am Surg 2014; 80: 1175-1178.
- Erdem H, C?etinku?nar S, Aziret M, Reyhan E, So?zu?tek A, So?zen S, et al. Can isolated pancreaticojejunostomy reduce pancreas fistula after pancreaticoduodenectomy with Roux-en-Y reconstruction? Ulus Cerrahi Derg. 2016; 32: 248-251.
- Ke S, Ding XM, Gao J, Zhao AM, Deng GY, Ma RL, et al. A prospective, randomized trial of Roux-en-Y reconstruction with isolated pancreatic drainage versus conventional loop reconstruction after pancreaticoduodenectomy. Surgery. 2013; 153: 743-752.
- Ben-Ishay O, Zhaya RA, Kluger Y. Dual loop (Roux en Y) reconstruction with isolated gastric limb reduces delayed gastric emptying after pancreatico-duodenectomy. World J Gastrointest Surg. 2019; 11: 93- 100.
- Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A, Orgill DP, SCARE Group. The SCARE 2018 Statement: Updating Consensus Surgical Case Report (SCARE) Guidelines. Int J Surg. 2018; 60: 132-136.
- Shrikhande SV, Sivasanker M, Vollmer MC, Friess H, Besselink MG, Fingerhut A, et al. Pancreatic anastomosis after pancreatoduodenectomy: A position statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2016; 161: 1221- 1234.
- Klaiber U, Probst P, Knebel P, Contin P, Diener MK, Bu?chler MW, et al. Meta-analysis of complication rates for single-loop versus dual-loop (Roux-en-Y) with isolated pancreaticojejunostomy reconstruction after pancreaticoduodenectomy. Br J Surg. 2015; 102: 331-340.