Cutaneous Spindle Cell Squamous Cell Carcinoma of the Lateral Cheek in an 87 Year Old Woman
- 1. Department of dermatology, Sun Patrol Skin Cancer Clinic, Australia
- 2. Department of dermatology, Dorevitch Pathology, Australia
Abstract
We present a case report of a cutaneous spindle cell squamous cell carcinoma on the lateral cheek of an87 year old woman. Clinical, dermatoscopic and dermatopathologic images are presented. A search of the literature has discovered no previously published dermatoscopic images of spindle cell squamous cell carcinoma. The dermatoscopic appearance of this tumour is compared with that of conventional poorly differentiated squamous cell carcinoma and atypical fibroxanthoma.
Keywords
Dermatoscopy, Dermoscopy, Spindle cell squamous cell carcinoma
Citation
Inskip M, Pinczewski J (2016) Cutaneous Spindle Cell Squamous Cell Carcinoma of the Lateral Cheek in an 87 Year Old Woman – A Case Report With Histopathology and Dermatoscopy. J Dermatolog Clin Res 4(1): 1062.
INTRODUCTION
Cutaneous spindle cell squamous cell carcinoma (SpSCC) is a rare malignant variant of squamous cell carcinoma (SCC) first described by Martin and Stewart in 1935 [1]. SpSCC usually presents as an eroded pink papule or raised nodule, most often on the photo damaged skin of the head and neck of elderly white males [2]
Some older studies portray SpSCC as an aggressive, poorly differentiated tumor with a higher rate of recurrence and metastatic spread than conventional SCC [3,4]. However it appears these studies were not controlled for known risk factors such as tumor size, depth, location and immune suppression. Thus Sp SCC arising from photo damaged skin may be no more aggressive than conventional SCC. SpSCC arising in skin that had been previously subjected to radiotherapy is associated with more aggressive behaviour however [5].
Histological SpSCC infiltrates the dermis as single atypical spindle cells with elongated nuclei but with no signs of the keratinisation associated with conventional SCC. In many cases the entire tumour is composed of atypical spindle cells. It may be difficult to tell SpSCC apart from other cutaneous spindle cell tumours including spindle cell (desmoplastic) melanoma, atypical fibroxanthoma, leiomyosarcoma and malignant myoepithelioma.
The diagnosis of SpSCC can only be established with certainty by the use of immunohistochemistry [2,6].
CASE PRESENTATION
An 87 year-old woman presented to a primary care skin cancer clinic in Melbourne, Australia with a 3 week history of a rapidly growing firm, pink, domed nodule on her left lateral cheek. She had no previous history of melanoma or non melanoma skin cancers. Examination showed Fitzpatrick skin type 2 and significant actinic damage of the face with multiple solar lentigines and small scattered actinickeratoses. The lesion of concern was a pink, smooth nodule measuring 10mm x14mm. There was no ulceration. Digital clinical and dermatoscopic images were taken with a Medicam 800 Fotofinder non-polarizing camera (Fotofinder Systems GmbH, Aichner, Birnbach, Germany) the dermatoscopy images being at 20 x magnification (Figures 1,2).

Figure 1 Rapidly growing 10 x14 x 4mm pink nodule on the lateral cheek of an 87 year old woman. The lesion had reached this size in just 3 weeks.
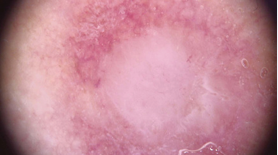
Figure 2 Dermatoscopic image of the lesion shown in figure 1 dominated by a central pale structure less zone with a few fine serpentine vessels.
Dermatoscopy revealed a non-pigmented lesion dominated by a pale pink structure less area with a few fine serpentine vessels.
Differential diagnosis included an inflamed epidermal cyst, cutaneous metastatic deposit, desmoplastic /amelanotic melanoma, Merkel cell carcinoma, atypical fibroxanthoma and leiomyosarcoma. Application of the “EFG rule,” which recommends excision of any skin lesion with the clinical features of elevation, firmness and growth required this lesion to be removed promptly [7]. An excisional biopsy was performed using an elliptical excision and the specimen was submitted for assessment by a specialist dermatopathologist.
Histology
Microscopic examination was consistent with a large nodular dermal malignant neoplasm which extended from the papillary dermis, without a Grenz zone, to the sub cutis (depth of invasion approximately 4mm) (Figures 3,4).
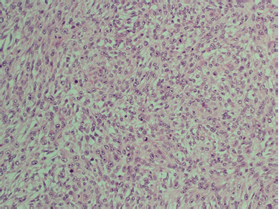
Figure 3 Hematoxylin and eosin (H&E) stained section taken at 40 x magnification. The image highlights the poorly differentiated, plump spindled cells densely packed within the neoplasm.
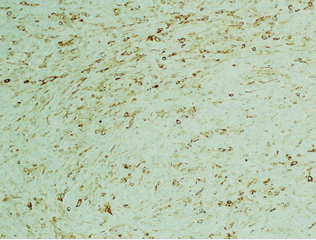
Figure 4 40 x magnification. The cells were focally positive when stained with a 34BE12 (high molecular weight cytokeratin) immunostain. Other keratinocytic markers were negative, as was the melanoma marker S100. The findings therefore supported a diagnosis of a poorly differentiated spindle cell squamous cell carcinoma.
The neoplasm was composed of atypical appearing spindled cells that were pleomorphic and mitotically active. The atypical cells had strong positive nuclear staining with P63 and also stained focally with the keratin markers AE1/AE3 and 34BE12 (high molecular weight cytokeratin) [8]. They were negative for the melanoma markers S100, SOX10 and melan-A. CD10 was negative, excluding an atypical fibroxanthoma. The neuroendocrine marker CD56 was negative. The staining pattern favoured a spindle cell squamous cell carcinoma8. The lesion appeared fully excised in the sections examined.
DISCUSSION
A search of the literature has not discovered any previously published dermatoscopic images of a SpSCC. However one study has addressed the dermatoscopic features of poorly differentiated SCC [9]. This study concluded the presence of a predominantly red colour; vessels in more than 50% of the tumour’s surface, a diffuse distribution of vessels and bleeding were significantly associated with poor differentiation. Despite being poorly differentiated the SpSCC we present demonstrated none of the dermatoscopic features of conventional poorly differentiated SCC described in this study. It is postulated that the atypical dermatoscopic appearance of this SpSCC may be due to its histological composition of densely packed atypical spindle cells and the absence of keratinisation associated with conventional SCC.
The dermatoscopy of atypical fibroxanthoma, another spindle cell carcinoma, was described by Lallas et al in 2013 [10]. Five atypical fibroxanthomas were studied which were ‘typified by reddish and whitish areas in combination with a polymorphous vascular pattern consisting of various combinations of linear, dotted, hairpin and highly tortuous vessel irregularly distributed over the surface of the lesion’. Again this is inconsistent with the dermatoscopic appearance of the SpSCC we present.
CONCLUSION
In conclusion we believe this is the first published dermatoscopic image of a SpSCC. The dermatoscopy of the SpSCC we present appears inconsistent with both conventional poorly differentiated SCC and atypical fibroxanthoma. Further published images and descriptions/case series are needed before the dermatoscopic diagnostic features of this condition can be stated with any confidence.
REFERENCES
1. Martin HE, Stewart FW. Spindle Cell Epidermoid Carcinoma. Am J Cancer. 1935; 24: 273-297.
3. LeBoit PE, Burg G, Weedon D, et al. World Health Organization Classification of Tumors: Pathology and Genetics of Skin Tumors. Lyon: IARC Press, 2006: 22.









































































































































