Intertriginous Linear Iga Bullous Dermatosis Treated with Colchicine
- 1. Department of Dermatolgy, Tel Hashomer Hospital, Israel
- 2. Department of Dermatopathology, Tel Hashomer Hospital, Israel
Abstract
Background: Linear IgA dermatosis (LAD) is considered to be one of the rare autoimmune mucocutaneous bullous dermatosis characterized histologically by the presence of subepidermal bullae with IgA autoantibodies directed against different antigens in the basement membrane visualized on direct immunofluorescence microscopy.LAD occurs in adults and children and can develop on the background of drug exposure, trauma, infectious process, vaccinations, malignancies and autoimmune diseases but in most patients, the inciting factor is unknown.
Main observations: We report a case of intertriginous LAD followed by contact with methyl alcohol. Direct immunofluorescence (DIF) revealed linear deposition of IgA and weak C3 along the basement membrane zone (BMZ). The patient was initiated on prednisone and colchicine and responded promptly to therapy.
Conclusions: Only limited cases of LAD have been described in the literature being triggered by irritant contact dermatitis with a predilection to the intertriginous areas.
Keywords
Linear IgA, Bullous Dermatosis, Intertriginous Areas, Colchicine, Irritant Contact Dermatitis, Treatment
Citation
Sakka N, Yahia KH, Volcon A, Brazilai A, Baum S (2015) Intertriginous Linear Iga Bullous Dermatosis Treated with Colchicine. J Dermatolog Clin Res 3(1): 1040.
INTRODUCTION
Linear IgA dermatosis (LAD) is considered to be one of the rare acquired autoimmune sub epidermal bullous dermatosis characterized immune pathologically by the presence of linear deposition of IgA along the dermoepidermal junction. The reported incidence is of only 0.5 per 100 individuals per year in Western Europe [1,2] and 0.22 and 0.69 cases per million per year in Germany[3] and Kuwait [4], respectively .
The disease has bimodal age onset, one in early childhood (also referred to as chronic bullous dermatoses of childhood) with a peak age of 4–5 years and one later in adulthood presenting between the 40th and 60th decades of life.
Several precipitating factors have been implicated as triggers or aggravating factors. Drug exposure has been strongly correlated with adult LAD and less likely to occur in childhood [5]. Vancomycin has been the most frequently reported culprit but diverse drug classes have been incriminated and include phenytoin, amiodarone, captopril, non-steroid inflammatory agent, carbamazepine, penicillin, amoxicillin, moxifloxacin, PUVA, furosemide, oxaprozin, IL-2, interferon (IFN)-α, statins, tea tree oil, angiotensin receptor antagonists and glibenclamide [6-12].
In some cases LAD has been associated with internal malignancy, paraproteinemia, infectious diseases or ulcerative colitis [13-16]. Sporadic reports have linked single cases with dermatomyositis, rheumatoid arthritis, lymphoma, acquired hemophilia, and multiple sclerosis, although these may be fortuitous associations [13,14,16-20].
Other exogenous factors implicated with LAD include vaccinations such as HPV and influenza [21] but also ultraviolet radiation [22]. The association between skin irritation as an aggravating factor is not well documented. In the case presented herein, we describe an unusual case of LAD induced by irritant contact dermatitis with a predilection for the intertriginous sites treated and remained under remission with colchicine.
CASE REPORT
A 59-year-old caucasian man with the background of hypertension, type 2 diabetes, benign prostatic hyperplasia and polymyalgia rheumatica under oral corticosteroid treatment, presented with a bullous eruption of a few days duration.
he appearance of the eruption was preceded by intense pruritus. In order to relieve the discomfort, the patient applied a solution containing methyl alcohol to the pruritic areas that was followed by blistering formation within hours after the application. The blisters appeared primarily on the skin folds; of the axillae, groins and the inframammary regions. He denied any symptoms suggestive of neither gluten enteropathy nor recent initiation of new medications. Our patient was not consuming any of the known enlisted culprit drugs.
Physical examination revealed an erythematous eruption consisting of urticarial plaques and tense, clear-filled bulla on the back, axillae, inguinal and inframammary skin folds. Figure 1A,1B Nikolsky sign was not elicited. Involvement of the oral, ocular and genital mucosal was spared.
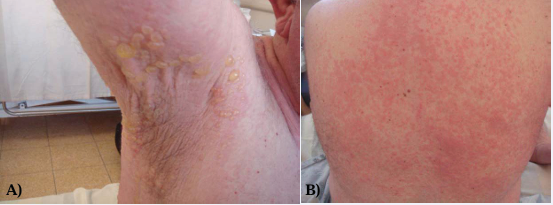
Figure 1 Figure demonstrating tense clear filled bullae on the background of erythematous plaque on the axillae (A) and inframammary region (B) urticarial papules and plaques on the back.
A skin biopsy was obtained from an intact blister and revealed subepidermal blistering with many neutrophils, nuclear dust and fibrinoid material. Direct immune fluorescence from skin demonstrated continuous linear deposition of IgA, complement C3and weak IgG along the basement membrane zone (Figure 2A,2B).
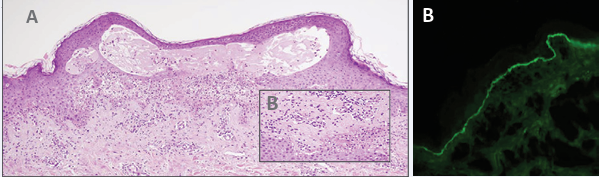
Figure 2 (A) Cutaneous biopsy demonstrating subepidermal blistering formation with distended papillae and nuclear dust (H&E X100) (B) Higher magnification showing neutrophils and subepidermal spilt (H&E X400)(C) Direct immunofluerences showing continuous linear deposition of Ig A along the basement membrane zone.
A search for circulatingantibodies was not performed. Based on the clinical presentation and immune histochemistry results, the diagnosis of LAD with predilection to the intertriginous areas was rendered with the eruption most likely being exacerbated by irritant contact dermatitis to methyl alcohol.
Routine laboratory studies revealed microcytic anemia (Hg-10.2 g/dl, MCV 76 f/l) and mildly deranged liver enzyme tests (gamma-glutamyltransferase-126 U/L range 0-65 U/L, lactate dehydrogenase-155 U/L range 0-125 U/L, alanine aminotransferase-137 U/L range 0-40 U/L). Further investigations such as anti endomysial antibodies test, bone marrow biopsy and computed tomography of pelvis and abdomen was performed and was found within normal range.
Because of patient’s background of microcytic anemia he was not considered a candidate for treatment with dapsone (avlosulfon). The patient was initiated with oral prednisone at a dose of 1mg/kg/day and colchicine 1.5 mg /day as a steroid sparing agent. Within 3 weeks of treatment, complete remission was achieved and steroids were tapered without any rebound effect. He maintained treatment on colchicine 1.5 mg/day for 2 months without any flare-up of his eruption. During follow-up period of 4 months no relapse was noted and colchicine was also discontinued.
DISCUSSION
The association between skin irritation as an aggravating factor of LAD is not well documented. Pellicanoet al. reported a patient who developed LAD after a chemical dermatitis caused by contact with sodium hypochlorite, suggesting a possible relationship with skin irritation [23]. Giraoet al. reported a case of LAD that occurred at the periphery of a cicatricial area caused by boiling methyl alcohol [24]. Godfrey et al. also described the association between trauma and cutaneous burns that could have possibly triggered the disease [14]. This emphasizes, in addition to our case presented herein, that physical trauma and irritant contact dermatitis may play a significant role in the aetiology of LAD.
The clinical features of LAD can be heterogeneous and imitate other blistering diseases.In adults, LAD can present with a broad spectrum of cutaneous manifestations ranging from vesicles, resembling dermatitis herpetiformis, to bullae mimicking bullous pemphigoid and toxic epidermal necrolysis (TEN) [24]. Lesions tend to appear as tense bullae and erythematous patches most frequently on the trunk and extremities but also on the buttocks and face [25,26]. In children, it often presents with grouped tense bullae arranged in an annular distribution resembling a string or cluster of pearls [5,21,27,28] and this clinical appearance represents the most characteristic clinical feature of LAD. Most often lesions are pruritic, resulting in numerous crusted papules on presentation. Classic sites of linear IgA bullous dermatosis of childhood are the trunk and iliosacral region; further regions such as the legs, face, or anogenital area can also be affected [5]. In our case, lesions appeared on intertriginous areas. LAD does not commonly manifests on body folds, thus this case represents an uncommon variant.In up to 50% of cases, there is mucous membrane involvement [5,29] especially of the oral mucosa [30] Ocular, genital, and pharyngeal manifestations are considered very rare [28,30].
Histologically, in both adult and childhood cases, there is subepidermal blistering formation with variable lymphocytic and neutrophilic infiltrate and sometimes even intra papillary micro abscesses are present, making it indistinguishable from dermatitis herpetiformis [5]. In drug-induced LAD, it appears more atypical and severe with presence of focal necrotic keratinocytes but not the typical full-thickness epidermal necrolysis of TEN [2,25].
Cutaneous biopsy combined with direct immune fluorescence (DIF) remains an essential tool to establish the correct diagnosis. Tissue-bound auto antibodies are detected by DIF in perilesional skin that demonstrates linear deposition of IgA and sometimes of IgG, IgM and complement (C3) at the dermal-epidermal junction [25,29,31].
In the majority of patients serum, indirect immune fluorescence microscopy (IIF) detects circulating IgA auto antibodies reactive with the epidermal side of 1 molNaCl saltsplit skin and immune electron microscopy has localized the immuno reactants to the sub laminadensa; however, in some, combined sub laminadensa and lamina lucida pattern has also been described [5,28,32].
Several target antigens have been identified during the last few years with immune blotting and are highly sensitive and specific in detecting auto antibodies in autoimmune blistering diseases and serve as serological confirmatory tests. In LAD there is a broad spectrum of target antigens and these include LAD285 [26,33-35], BP180 (collagen XVII), LABD-97 and LAD-1 ( LAD-1 and LABD-97 are both fragments of the shed extracellular domain of BP180 localized in the lamina lucida), BP230 and rarely, collagen VII [29,30,32,36] The variety of target antigens involved and location may explain the heterogeneous clinical and immune pathologic characteristics of LABA.
Treatment of LAD varies with the degree of involvement and identification of inciting factors. When an offending drug agent is identified, withdrawal of that agent alone often results in gradual resolution of skin findings within several weeks [5]. In spontaneous LAD the primary therapy remains dapsone [26,30,31], a leprostatic agent, with the most common encountered adverse effects being hemolysis in glucose-6-phosphate dehydrogenase–deficient patients and methemoglobinemia. In some patients with LAD, they may require a low dose of prednisone initially to suppress blister formation. Based on the fact that our patient was suffering from anemia and had extensive bullae formation he was initiated on oral corticosteroids and colchicine. The specific mechanism of action of colchicine is not known. It appears colchicine inhibits microtubule polymerization and interferes with the intracellular assembly of the inflammasome complex that mediates activation of interleukin-1beta in neutrophils and monocytes and thus exerts its anti-inflammatory effects by impeding leukocyte chemotaxis, phagocytosis and lactic acid production [37,38]. As it inhibits neutrophil adhesion to the epidermis it is often being used for treating neutrophilic dermatoses but also because is a welltolerated anti-inflammatory drug with a low side-effect profile [38-40]. Colchicine has been previously used as a therapeutic agent in a small number of cases [38,41-43] for LAD, and even prescribed in children [38], with good therapeutic response and minimal reported side effects.
CONCLUSION
No comparative studies have assessed between different treatments modalities for the LAD mainly because of the rarity of the disease. Nevertheless, based on the excellent safety profile and high response rate, we recommend colchicine to be considered as one of the first line agents for treating LAD. Additionally, we suggest that when evaluating patients with LAD, an irritant factor needs to be assessed. Our patient responded to treatment and remained free of symptoms even after all treatments remedies was ceased .This also supports our assumption that LAD can be induced by irritant contact dermatitis given the fact that in the absence of the triggering factor, the patient remained under complete remission.









































































































































