Reactive thrombocytosis leading to stent thrombosis
- 1. Department of Cardiology, JJ Hospital, India
Abstract
Percutaneous coronary intervention is associated with much complication and stent thrombosis is most feared amongst them. Common etiology of stent thrombosis includes high angiographic thrombus burden, inadequate antiplatelet dosing, total stent length, diabetes, and renal disease. Rarely can it be associated with thrombocytosis. We are reporting a rare case of stent thrombosis associated with reactive thrombocytosis. Although acute coronary events have been documented due to essential thrombocytosis but very few cases of reactive thrombocytosis leading to acute Coronary syndrome (ACS) are reported. Thrombocytosis as a possible etiology is suspected when other risk factors including antiplatelet resistance is ruled out .In these cases adequate treatment of both stent thrombosis and thrombocytosis need to be administered simultaneously and possible etiology of thrombocytosis sorted out and treated.
Keywords
Acute Coronary syndrome, Stent thrombosis, Reactive thrombocytosis
Citation
Kalantri P, Kaushik A, Singla R, Bade A, Bansal NO (2020) Reactive thrombocytosis leading to stent thrombosis. J Cardiol Clin Res 8(1): 1151.
ABBREVIATIONS
LAD: left anterior descending; RCA: right coronary artery; ACS: acute coronary syndrome; PCI : Percutaneous coronary intervention; CAG : Coronary angiography; DES : Drug eluting stent
INTRODUCTION
Stent thrombosis is a most feared complication of coronary stenting because of its immediate morbidity and mortality. Etiology is multifactorial commonly like high angiographic thrombus burden ,total stent length ,diabetes, renal insufficiency, preprocedural inadequate thienopyridine administration and there is rare possibility with thrombocytosis. Here we report a case of acute stent thrombosis in patient who developed stent thrombosis within 24 hours of Left anterior descending artery (LAD) stenting associated with reactive thrombocytosis despite of adequate antiplatelets therapy with aspirin and Clopidogrel.
CASE PRESENTATION
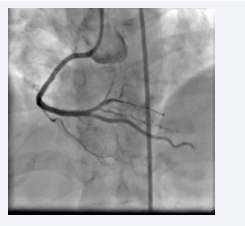
A 37 year old female patient non hypertensive ,non diabetic was admitted to our hospital with chest pain for last 2 hours with ST segment elevation in inferior leads, and reciprocal changes in anterior leads with quantitative troponin T value of 540 pg/ml and no other associated risk factors. Her routine investigation was unremarkable except for Hb =9.0 g/dl with platelet count being 1.68 lakhs/mm3 of blood. After loading with aspirin , Clopidogrel along with Atorvastatin patient was considered for urgent Coronary angiography (CAG) which showed Right coronary artery (RCA) 100% thrombotic occlusion (Figure 1)
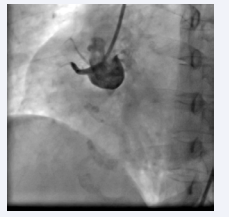
Figure 1: Angiography showing proximal RCA- total occlusion.
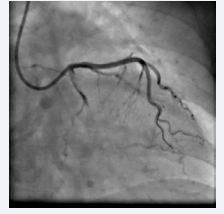
and LAD 80 % lesion across diagonal (Figure 2).
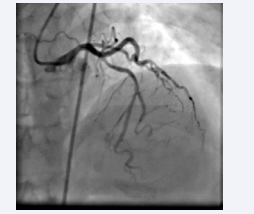
Figure 2: Angiography showing proximal LAD 80 % lesions
Primary angioplasty was carried out to RCA with 3.5 x 48 mm DES (drug eluting stent) from proximal to mid RCA with TIMI III flow (Figure 3)
and LAD percutaneous coronary intervention (PCI) decided to be carried out at later stage, patient was given 600 mg Clopidogrel and 5000 IU heparin according to bodyweight. On second stage after one week PCI to LAD was carried out with 3.5 x 43 mm DES with good result TIMI III flow (Figure 4)
(under cover of required dose of heparin and antiplatelets). On the second day of the LAD PCI about 20 hours from the procedure patient developed sudden chest pain with profuse sweating with ST elevations in anterior leads and quantitative Trop T of around 6000 pg/ml reflecting acute anterior wall myocardial infarction . Patient was rushed to cath lab where left shoots showed acute LAD stent thrombosis (Figure 5).
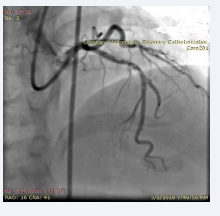
Figure 5: LAD instent thrombus.
Patient was thrombolysed with intracoronary reteplase with establishment of TIMI III flow (Figure 6)
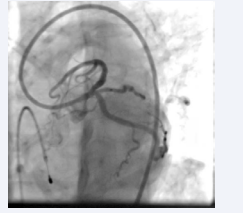
Figure 6: Post intracoronary thrombolysis, LAD showing TIMI III flow.
and LAD patency with good result. Patient resistance to clopidogrel was tested which was negative .Patients platelet trend as shown (Table 1)
Table 1: Table showing variation in platelets count.
| No of days | Admission | 7th day | 8th day Stent Thrombosis | Therapy started | 14th day | Follow up after 6 weeks |
| Haemoglobin | 9.2 | 10 | 10.1 | 10 | 12 | 13.4 |
| White blood cells | 10,800 | 13700 | 26,400 | 20600 | 11300 | 7600 |
| Platelets | 1,68,000 | 4,44,000 | 9,86,000 | 8,48,000 | 3,13,000 | 1,40,000 |
was suggestive of reactive thrombocytosis on the day of stent thrombosis which subsequently resolved thereafter after giving cytoreductive therapy along with antibiotics. Patient was observed for 48 hours in ICCU and subsequently discharged after 2 week with normal platelet count.
DISCUSSION
Stent thrombosis [1] is one of the fatal complications of the percutaneous coronary intervention if it occurs acutely. Stent thrombosis is defined based on the timing of the stent thrombosis and the level of certainty of the event.
Based on timing of event acute stent thrombosis occurs between zero to 24 hours after coronary stent implantation. The subacute stent thrombosis occurs between 24 hours to 30 days after coronary stent implantation. Late stent thrombosis occurs between 30 days to one year after coronary stent implantation. Finally, very late stent thrombosis occurs 1 year after coronary stent implantation
Based on certainty of event Definite stent thrombosis is confirmed when there is angiographic confirmation of stent thrombosis. The presence of a thrombus that originates in the stent or the segment 5 mm proximal or distal to the stent, and the presence of at least one of the following criteria within a 48-hour period:
• Acute onset of ischemic symptoms at rest
• New ischemic ECG changes
• Typical rise and fall in cardiac biomarkers
• Nonocclusive thrombus
• Intracoronary thrombus
• Occlusive thrombus
• TIMI 0 or TIMI 1 flow intrastent or proximal to a stent up to the most adjacent proximal side branch or main branch.
Stent thrombosis has multifactorial etiology and one of rare etiology is thrombocytosis which should be suspected when all other common etiologies are ruled out .As our patient belongs to acute stent thrombosis category and was not having other risk factors like excessive thrombus burden, stent landing zone on plaque ,dissection etc we looked for possible etiology as thrombocytosis as platelet count was 9.86 lakh when patient had stent thrombosis.
Based on etiology thrombocytosis can be of two types [2] Essential (primary thrombocytosis) and Reactive thrombocytosis (Secondary). Essential thrombocytosis is a rare disorder is associated with abnormal megakaryocytes in the circulation [3- 5]. It is associated with events like strokes, transient ischemic attacks, retinal artery or retinal vein occlusions, digital ischemia, and acute coronary syndrome. Only few case reports of coronary artery thrombosis associated with essential thrombocytosis have been previously described in the literature.
Reactive thrombocytosis is caused by elevated thrombopoietin level and other cytokines, such as interleukin-6 [2]. Patients with reactive thrombocytosis do not usually require cytoreductive medication or antiplatelet treatment [4], but, in some circumstances may require antiplatelet treatment given the potential risk of acute coronary syndrome, stroke, pulmonary embolism, or pulmonary hypertension. Our literature search identified very few case report describing reactive thrombocytosis following the episode of myocardial infarction [6,7] leading to recurrent acute coronary syndrome. In our case patient might have developed reactive thrombocytosis due to Iron deficiency anemia and Urinary tract Infection.
It is well documented that essential thrombocytosis is a predilection to myocardial infarction [2]. Our patient might have developed another episode of acute coronary syndrome (ACS) from reactive thrombocytosis. So pathophysiology of stent thrombosis in this case is probably not from atherosclerosis or plaque rupture but due to elevated platelet count from reactive thrombocytosis resulting in a second myocardial infarction. Another possibility is that he might had primary resistance to clopidogrel so we did a enzyme resistant assay which turn out to be negative. In this scenario, the reactive thrombocytosis appears to be the culprit agent. We decided to substitute clopidogrel with a newer antiplatelet medication, ticagrelor and therapeutic doses of Enoxaparin was started to treat recurrence of acute coronary syndrome. Hydroxyurea, aspirin, and ticagrelor were initiated on consultation with hematologist. Antibiotics were given for treatment of Urinary Tract Infection. Enoxaparin and hydroxyurea were discontinued when his platelet count returned to his baseline. This case highlights the potentially underrecognized danger of reactive thrombocytosis and stresses need for comprehensive evaluation of the pathophysiology, consequences, and management of reactive thrombocytosis.
CONCLUSION
Reactive thrombocytosis can be a rare cause of acute coronary syndrome including stent thrombosis. A thorough vigilance for thrombocytosis as possible etiology should be sorted to not miss it especially if patient is not having other cardiac risk factors.
ACKNOWLEDGEMENT
I am deeply indebted to Dr Narendra Omprakash Bansal, Head of Department, Department of cardiology, Sir J.J groups of Hospitals for helping and guiding us in this study. This article has been read by all authors and it represent a honest work