Recurrent Ventricular Tachycardia Associated with Vasospastic Angina Effectively Managed with Implantable Cardioverter Defibrillator
- 1. Department of Medicine, Cardiovascular Division, Section of Electrophysiology, University of Pennsylvania, USA
Abstract
Introduction: There is a paucity of data regarding the use of implantable cardioverter defibrillators (ICDs) in cases of vasospastic angina associated with ventricular tachycardia (VT). We present a case supporting their use in this clinical scenario.
Case: A 66 year-old male with recurrent nonexertional chest pain was found to have repetitive bursts of VT on inpatient telemetry monitoring. After an ICD was implanted, the patient experienced further VT, terminated by an ICD shock.
Conclusion: This case illustrates that ICD therapy may prevent fatal ventricular tachycardia associated with vasospastic angina.
Keywords
Electrophysiology, Ventricular tachycardia, Implantable devices, Ventricular tachycardia/fibrillation, Vasospastic/Prinzmetal/Variant angina
Citation
Fields AV, Mehta NN, Simson MB, Lin D (2015) Recurrent Ventricular Tachycardia Associated with Vasospastic Angina Effectively Managed with Implantable Cardioverter Defibrillator. J Cardiol Clin Res 3(1): 1043.
CASE
There is a paucity of data regarding the use of implantable cardioverter defibrillators (ICDs) in cases of vasospastic angina associated with ventricular tachycardia (VT). A six-year study of sixty patients with vasospastic angina found a 25% incidence of sudden death in those with (n=8) compared to those without (n=52) polymorphic VT [1]. We present a case supporting the use of ICD for recurrent VT associated with vasospastic angina.
A 66 year-old man presented with recurrent nonexertional, substernal chest pain. The baseline ECG was normal, except for sinus bradycardia. Cardiac enzymes, exercise stress test, and echocardiogram were normal. On the first night, he awoke with chest pain followed by repetitive bursts of nonsustained ventricular tachycardia, which spontaneously resolved. Cardiac catheterization revealed minimal atherosclerotic disease. An electrophysiology study demonstrated no inducible ventricular arrhythmias, and metoprolol was initiated. He awoke with chest pain the next night, and telemetry revealed ST segment elevation followed by rapid ventricular tachycardia (Figure 1).
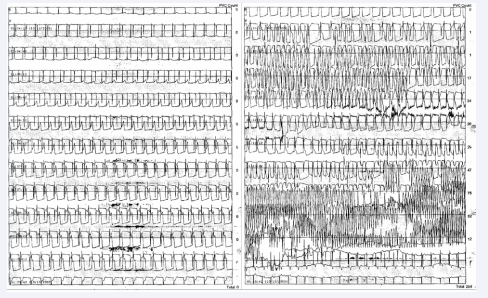
Figure 1: Telemetry monitoring demonstrated ST segment elevation followed by rapid VT.
Vasospastic angina was diagnosed and management was changed to nifedipine extended-release (ER) 90 mg daily. An ICD was implanted. One day after discharge, the patient experienced chest pain followed by palpitations and an ICD shock. The ICD electrogram showed rapid ventricular tachycardia at 267 BPM (Figure 2).
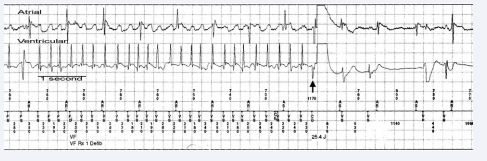
Figure 2: ICD electro gram showed rapid VT at 267 BPM effectively terminated by 25.4J ICD shock
The rhythm following the shock was sinus with frequent PVCs. The patient’s nifedipine ER dose was increased to 60 mg twice daily. The patient has had no chest pain or ICD events at one year follow-up.
In cases of vasospastic angina, it is important to consider the presence of factors that have been shown to predict sudden cardiac death when choosing therapy. Such factors include presence of polymorphic ventricular tachycardia and ventricular fibrillation [1-3]. In addition, angina-associated syncope is associated with increase risk of sudden death these patients [4- 6]. The risk of sudden cardiac death has also been shown to be increased in patients without significant coronary stenoses. In our patient with minimal atherosclerotic disease, we implanted an ICD because of the malignant nature of the arrhythmia and inability to test effectiveness of medical therapy in preventing recurrence. This case illustrates that ICD therapy may prevent fatal ventricular tachycardia associated with vasospastic angina.









































































































































