A Practical and Simplified Management Approach of Multiple Myeloma
- 1. Department of Internal medicine and clinical hematology, University Hospital Mohammed VI Oujda, Morocco
- 2. Department of Internal Medicine, University Hospital of Strasbourg, France
Abstract
Significant progress has been made in the pathophysiological understanding, diagnosis and management of multiple myeloma. Therapeutic indications have become more and more codified taking into account a set of clinical and paraclinical parameters currently considered to be the most closely correlated to the prognosis of the disease. In terms of treatment, the triphasic approach based on induction, consolidation and maintenance is actually the gold standard. Autologous stem cell transplantation also remains systematic in eligible patients even in the era of new highly innovative and effective treatment. Finally, residual disease, one of the most powerful predictors of post-treatment evolution, is becoming increasingly important and will be most likely an integral partof the response criteria.
Keywords
- Myeloma
- Autologous transplantation
- Induction
- Consolidation
- Maintenance
- Residual disease
Citation
Serraj K, Alaoui H, Hamaz S, Bachir H, Andres E (2018) A Practical and Simplified Management Approach of Multiple Myeloma. J Chronic Dis Manag 3(1): 1022.
INTRODUCTION
Multiple myeloma has undergone significant advances in physiopathology, diagnosis and therapy over the last 20 years. However, many unanswered questions remain a major challenge for basic and clinical research of the disease [1]. In this article, we will discuss pretreatment approach, indications, prognostic stratification and finally the main therapeutic principles, practical algorithms and future perspectives.
PROGNOSTIC CORRELATIONS AND THERAPEUTIC INDICATIONS
The iconic Durie and Salmon classification has long been the unique and indispensable tool for prognostic stratification and discussion of therapeutic indications for multiple myeloma. The ISS (International Scoring System) with its two parameters serum albumin and beta2-microglobulin arrived later and stood out for its prognostic relevance and simplicity. Regarding treatment, indications were limited only to symptomatic patients. Recently, studies demonstrated that even in completely asymptomatic patients, some subgroups evolved in 80% of cases and in less than 2 years after diagnosis to severe and complicated myeloma. These included patients with medullary plasmocytosis ≥ 60%, those with a serum free light chain ratio> 100 and finally patients with even minimal bone lesion on MRI. These data led to the recent adoption by the International Working Myeloma Group (IWMG) of the new therapeutic criteria that we summarize in Table 1 [2-4].
Table 1: Treatment indications of multiple myeloma
| Hypercalcemia |
| Renal insufficiency |
| Anemia |
| Bone lysis |
| Infections |
| Amyloidosis |
| Hyperviscosity |
| Plasmocytosis ≥ 60% |
| Ratio of serum free light chains ≥ 100 |
| MRI Bone lesion ≥ 0,5 mm |
MAIN PRINCIPLES OF TREATMENT
In both de novo myeloma and refractory/relapsing myeloma (R/R myeloma), a number of “golden rules” deserve to be constantly emphasized. First, it is always essential in a patient with anemia, renal failure or hypercalcemia to rule out all other differential diagnoses and to confirm the specific causal link connecting the myeloma to the complication. Thus, anemia must systematically make seek iron or vitamin deficiency, iatrogenic or hemolytic anemia, while dehydration, drug toxicity, urinary infection and tract obstruction are the most important differential diagnoses before retaining the myelomatous origin [1]. Once this link established and the therapeutic indication validated, the triphasic approach must be the rule with an induction, a consolidation and a maintenance phase. Indeed, the risk of relapse is even lower as the remission is deep and prolonged over time. The recent close correlation between negative residual disease and progression-free and overall survival is a perfect illustration of this finding. It is therefore a question of being as aggressive as possible by favoring synergetic and most often triple pharmacologic combinations while taking into account the performance status and the eligibility or not of patients to autologous hematopoietic stem cell transplantation [5]. For theR/R myeloma, management will be discussed is case-by-case depending on the first treatments, the duration of the previous remission and the evolution in time of the patient with respect to age and comorbidities. It is also important to remember that multiple myeloma is a “multi-monoclonal” diseasewith more and more tumor clones expressed proportionally to duration of disease and number of therapeutic lines. The clinician must always find a fair compromise by proposing therapeutic associations that are sufficiently effective while taking into account the heavy therapeutic history that usuallymakes the patients even more fragile and their disease refractory [6].
FRONTLINE INDUCTION / CONSOLIDATION
In eligible patients for autologous hematopoietic stem cell transplantation, Bortezomib-based regimens are by far the most effective. These are essentially VTD (Bortezomib - Thalidomide - Dexamethasone), VCD (Bortezomib - Cyclophosphamide - Dexamethasone) and PAD (Bortezomib - Doxorubicin - Dexamethasone) and VRD (Bortezomib - Lenalidomide – Dexamethasone) with respective rates of complete and very good partial response of 70%, 62%, 65% and 75% (Figure 1) [7].
Figure 1: Treatment algorithm in Myeloma Transplant eligible patients VTD: Bortezomib – Thalidomide – Dexamethasone; VCD: Bortezomib – Cyclophosphamide – Dexamethasone; PAD: Bortezomib – Doxorubicine – Dexamethasone VRD: Bortezomib – Cyclophosphamide – Dexamethasone; ASCT: Autologous Stem Cell Transplant
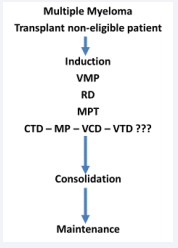
For elderly patients who are not eligible for autologous transplantation, the majority of regimens were validated after beingcompared to the Alexanian protocol. These include the MPT regimen (Melphalan - Prednisone - Thalidomide), VMP (Bortezomib - Melphalan - Thalidomide) and RD (Lenalidomide - Dexamethasone). It was also shown that the comparison between the MPT and MPR (Melphalan - Prednisone - Lenalidomide) regimens does not show significant difference in efficacy, thus justifying the frequent absence of MPR of the recommendations of frontline therapy (Figure 2) [8].
Figure 2: Treatment algorithm in Myeloma transplant non-eligible patients VMP: Bortezomib – Melphalan – Prednisone; RD: Lenalidomide – Dexamethasone; MPT: Melphalan – Prednisone – Thalidomide; CTD: Cyclophosphamide – Thalidomide – Dexamethasone; MP: Melphalan – Prednisone; VTD: Bortezomib – Thalidomide – Dexamethasone; VCD: Bortezomib – Cyclophosphamide – Dexamethasone
MAINTENANCE TREATMENT
Several molecules have been evaluated in maintenance treatment of multiple myeloma. The results obtained with dexamethasone and thalidomide was disappointing with an unfavorable long-term tolerance profile. In contrast, the encouraging data of lenalidomide and Bortezomib have positioned them as treatments of choice in this indication. Two large studies evaluated lenalidomide and found a significant improvement in progression-free survival (18 months) and overall survival. On the other hand, Bortezomib demonstrated a particular contribution in patients with unfavorable cytogenetic profile, with a progression-free survival curve that was made to overlap with standard-risk patients. These data led to the adoption by several US and European centers of a maintenance approach using lenalidomide in standard-risk patients and bortezomib in those with intermediate and high risk. [9].
WHAT ABOUT R/R MYELOMA?
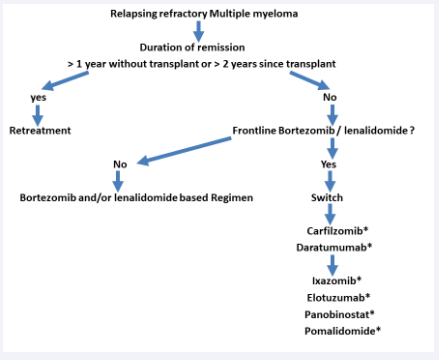
Advances in the pathophysiological understanding of multiple myeloma have led to the identification of new and increasingly effective targets and treatments. Retreatment is a perfectly valid alternative when the relapse is late. In several clinical trials, the response to a second autograft in previously autografted patients may be close to 90% with significantly better results in patients in whom the duration of initial remission would exceed 2 years. In patients who are refractory despite highly effective first-line treatments such as bortezomib and lenalidomide, the use of all new molecules becomes a major necessity. Of all the new treatments that have been evaluated in R/R myeloma, by far daratumumab and carfilzomib have taken a real step ahead. Daratumumab, which had a significant response rate as monotherapy, was comparedin the POLLUX study in combination with lenalidomide-dexamethasone (DRD) versus RD alone. In this study, DRD obtained rapidly negative minimal residual disease (MRD) in50% of patients with a dramatic improvement in progression-free survival and overall survival. About carfilzomib, very promising results were obtained in the ASPIRE and ENDEAVOR studies that comparedrespectively KRD (carfilzomib - lenalidomide - dexamethasone) versus RD and KD (carfilzomib - dexamethasone) versus VD (bortezomib - dexamethasone). Finally, the main other treatments validated in R/R myeloma after at least 2 previous therapeutic lines are Elotuzumab, Ixazomib, Pomalidomide and Panobisnostat, with for the last 3 treatments a great advantage of convenience due to their oral route of administration (Figure 3) [6,10].
Figure 3: Treatment algorithm of refractory relapsing myeloma *Molecule Based regimen
ACTUALITIES IN THE MANAGEMENT OF MYELOMA-RELATED COMPLICATIONS
After long years of monopoly of zoledronic acid, bone disease of myeloma has actually another therapeutic alternative. Denosumabat much higher dosages in myeloma than in osteoporosis is at least equally effective to zoledronic acid and particularly useful, especially in patients with renal insufficiency [11]. Regarding anemia, erythropoietin is certainly an attractive alternative to reduce transfusion dependence but should be avoided when the treatment of myeloma is based on thalidomide due to a very high risk of thromboembolism, which is not reducible by usual thromboprophylaxis [12]. Infections are also a common problem and a major source of morbidity and mortality in myeloma. A study presented at the last congress of the American Society of hematology reported a 50% reduction in the number of severe infectious episodes and infection-related deaths in patients who received daily 500 mg levofloxacin prophylaxis for a total duration of 12 weeks [13].
FUTURE AND PERSPECTIVES
A possible autograft is an indispensable autograft in patients with multiple myeloma. Indeed, the legitimate question of the usefulness of autologous transplantation in the era of new molecules has been the subject of a recent trial, which compared the outcome of autograft versus no autograft in patients who receivedinitial VRD induction (Bortezomib - Lenalidomide - Dexamethasone) the achievement versus failure to perform autologous hematopoietic stem cell transplantation. Obvious superiority has been found in the “autograft” arm [14]. The optimization and increasing efficacy of the treatments have also resulted in a large fraction of patients having a negative residual disease that correlated with a significant improvement in progression-free survival and overall survival. However, the temptation to rapidly integrate MRD into the criteria for therapeutic response still faces persistent questions about the standardization of techniques and the possible impact of negative MRD on the subsequent therapeutic approach [15].