The Burden of Gastroesophageal Reflux Disease on the Cost of Managing Chronic Diseases in Australia. The Need for a New Diagnostic and Management Paradigm
- 1. CNI Molecular Imaging, University of Notre Dame, Australia
- 2. Ryde Medical Centre, Australia.
- 3. Sydney Heartburn Clinic, Concord Hospital & University of Sydney, Australia
- 4. Brisbane Private Hospital, Australia
Abstract
Introduction: Chronic disease poses a major problem for the Australian healthcare system as the leading cost-burden and cause of death. Gastroesophageal reflux disease (GORD) typifies the problems with a growing prevalence and cost. We hypothesise that a new scintigraphic test could streamline and speed up the diagnosis, especially in extraoesophageal disease which is universally problematic.
Materials & methods: Data was collected from 2 groups of patients. Patients undergoing fundoplication for severe GORD (n=30) and those with atypical symptoms (n=30) were studied by scintigraphy and 24-hour oesophageal pH, impedance and manometry in an outpatient setting.
Results: Mean age of cohort was 55.8 years with 40 females and 20 males. Body mass index was a mean of 28.3. DeMeester score was normal in 12/60 with atypical symptoms and abnormal in the rest. Good correlation was shown between scintigraphy and impedance, manometry and distal pH readings. Pulmonary aspiration was shown in 25/60 (15 with atypical symptoms) and LPR in 20/30. Several impedance, manometric and scintigraphic finding were good predictors of lung aspiration of refluxate.
Conclusion: Scintigraphy provides a good tool for screening patients with typical and atypical symptoms of GORD. It is well correlated with the standard methods for the diagnosis and provides visual evidence of LPR and lung aspiration, especially in atypical disease.
Keywords
• GORD
• Reflux disease
• Scintigraphy
• Laryngopharyngeal
• Aspiration
• Impedance
• pH
Citation
Burton L, Beattie J, Falk GL, Van der Wall H, Coman W (2020) The Burden of Gastroesophageal Reflux Disease on the Cost of Managing Chronic Diseases in Australia. The Need for a New Diagnostic and Management Paradigm. J Chronic Dis Manag 4(1): 1024
INTRODUCTION
Chronic diseases are an increasingly prevalent challenge to healthcare systems globally from a financial and societal perspective. This group of diseases are the leading cause of illness and disability, accounting for ~70% of deaths worldwide [1,2]. Global healthcare spending is projected to reach $US10.059 Trillion by 2022, an annual growth rate of 5.4% [3].
Gastro-oesophageal reflux disease (GORD), is an exemplar of the complexities of chronic disease [4]. The changing epidemiology of the Australian population is associated with an increasing prevalence of GORD and other consequent chronic diseases [4-6].
Gastro-oesophageal reflux disease is defined as “a condition which develops when reflux of stomach contents causes troublesome symptoms and/or complications” [7]. The current diagnostic testing regimen is predicated on acid exposure despite the universal definition being devoid of this term. There is increasing evidence for more complex injury from agents such as pepsin and bile constituents [6]. The focus on typical symptoms of heartburn and regurgitation with the interdependence on acid exposure time (AET), underestimates disease in individuals with atypical symptoms. Diagnostic efficacy is impaired as the symptoms span a multitude of disparate specialities [8].
The true economic cost of GORD may be approximated from data extracted from the Pharmaceutical Benefits Schedule (PBS) and the Medicare Benefits Schedule (MBS). There has been a reduction in the cost of anti-reflux medications from AUD$500M in 2012-2013 to AUD$264M in 2018-2019 [9,10]. Nevertheless, Esomeprazole (Nexium) and Pantoprazole (Somac) are consistently amongst the top 10 most prescribed drugs in Australia [11]. A recent multi-centre trial has reported that that up to 30% of patients may be inappropriately treated with PPIs [12]. Diagnostic procedures for GORD under the MBS increased from AUD$67.2M in 2012-2013 to AUD$80.3 in 2018- 2019 [13,14].
We hypothesise that a validated simple scintigraphic reflux study can screen for local and extra-oesophageal manifestations of GORD, thereby expediting the diagnosis and reducing costs.
METHODS
Population
The two patient groups consisted of consecutive patients referred for laparoscopic fundoplication for failed therapy with proton pump inhibitors (PPIs), or that remained undiagnosed after 8 weeks of investigation and classified according to the reflux symptom index criteria of Belafsky et al. [15]. The second group comprised patients with atypical symptoms of GORD presenting to otolaryngologists or other specialists. All patients underwent 24-hour oesophageal impedance/pH/manometry studies. Major symptoms included heartburn, globus and regurgitation or extra-oesophageal symptoms such as cough, sore throat, recurrent throat clearing, voice change, laryngospasm and aspiration. Scintigraphy was used to prospectively evaluate extra-oesophageal refluxate and the possibility of pulmonary aspiration of refluxate. These patients had failed maximal therapy and underwent these investigations after cessation of PPI therapy. Clinical data and body mass index (BMI) were prospectively collected using a standardized proforma and entered into a database.
24-hour impedance study
24-hour impedance study with two channel 24-hour pH was performed on all patients as has been described elsewhere [16]. Briefly, a trans-nasal catheter with 2 level impedance rings and 2 level pH electrodes connected to an external monitoring device was inserted into the oesophagus. Impedance rings were set at 5 and 15 cm above the upper border of the lower oesophageal sphincter (Zephyr device, catheter ZAI-BD31, Sandhill Co, Highlands Ranch, Colorado, USA). Reflux was classified by the consensus on impedance and pH monitoring [17].
Manometry
Standard stationary manometry was obtained with a water perfused dent sleeve 8 channel catheter (Dent Sleeve International, Mississauga, Ontario, Canada) as described elsewhere [16]. Data was recorded with a multichannel recording system (PC polygraph HR Medtronics, Synectics Medical, Minneapolis, Minnesota, United States) and analysed using the PolyGram software program (Medtronics, Synectics Medical, Minneapolis, Minnesota, United States). Motility was graded by modification of Kahrilas et al., method [17,18].
Scintigraphy
Patient preparation involved a 6 hour fast and 24-hour cessation of anti-reflux medication prior to the test. The patient was administered 60-100MBq of Phytate in 50mL of water followed by a further 50mL to clear the oropharynx and oesophagus. Dynamic images were acquired upright for 2 minutes then supine for 30 minutes on a Hawkeye 4 gamma camera (General Electric, Milwaukee, United States), with the mandible and stomach in the field of view.
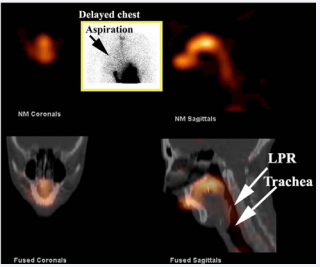
Delayed static imaging was obtained 2hrs later for assessment of lung aspiration of refluxate (Figure 1).
Figure 1: SPECT/ CT and delayed image of lungs (inset). The inset image shows a delayed study of the anterior chest at 2 hours. There is aspiration of refluxate into the right lung (arrow). The SPECT/ CT image shows the scintigraphic image in the upper panel and the fused image with the CT study in the lower panel. There is significant contamination of the laryngopharynx (LPR) and trachea by refluxate.
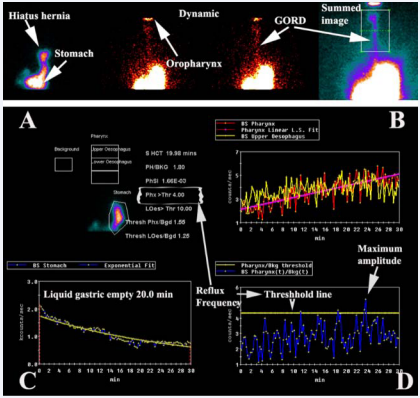
Images analysis is shown in Figure 2.
Figure 2: Analysis of the dynamic study. The upper panel shows the dynamic study which allows visualisation of any hiatus hernias and GORD to the level of the pharynx (arrows). The summed dynamic image clearly shows evidence of GORD to the level of the pharynx. The panel below illustrates the analysis of the pattern of reflux in the pharynx/laryngopharynx (upper box) and upper oesophagus (middle box) in A. B shows the pattern of activity in the pharynx/ laryngopharynx (red curve with fitted pink line) and oesophagus (yellow curve) over 30 minutes of acquisition. The liquid gastric emptying (C) is calculated by an exponential fit to the activity over the stomach region of interest in A. Frequency and amplitude of reflux is calculated from the pharyngeal/ laryngopharyngeal curve in B after taking into account background activity (Threshold line) in D.
A subgroup of the 30 patients with extra-oesophageal symptoms underwent single photon emission computed tomography (SPECT), which was fused with x-ray computed tomography (CT) on the same instrument (Figure 1).
Statistical analysis
Data was analysed by nonparametric statistical methods as much of the analysis was of ordinal data. Standard ANOVA statistics and 2-tail Spearman (non-parametric data) and Pearson correlation coefficient (parametric data) with significance levels of 0.05 were utilised. Receiver operating characteristic (ROC) analysis was also undertaken where appropriate. Statistica V8 software (Statsoft, Oklahoma, United States) package was used for data analysis.
RESULTS
Population
Sixty consecutive patients (40M, 20F) were entered into the database approved by the University of Notre Dame Ethics Committee (No. 015149S). Average age was 55.8 years (Range: 18-87, Median: 58 yrs). Thirty patients gave a history of predominantly atypical symptoms and 28 a history of typical heartburn and regurgitation with overlap in 2.
The BMI in this cohort ranged from 19.8 to 47.9 kg/m² , with a mean of 28.3 and median of 27.4. Twenty seven of the 60 patients had a BMI in excess of 30.0 kg/m² (Normal: 18.5 to 24.9). No patient had a BMI below the normal range.
DeMeester scores: The DeMeester score[19], was normal in 12 of 60 patients, being less than 14.7. These patients were in the group with atypical symptoms.
Hiatus hernias. A hiatus hernia was diagnosed in 24 patients based on endoscopic criteria.
Manometry
Oesophageal motility: Normal oesophageal motility was present in 13 patients. Mild abnormality was found in 9, mild to moderate in 12, moderate in 13 and severe in 13 patients. In the Kahrilas et al. [20], classification system this would have been normal in 22, moderate in 12 and severe in 26 patients.
Mean LOS pressure 6 mm Hg (Range: 0-29, Median: 4). Normal was considered to be above 26 mm Hg [21]. LOS pressure was normal in only 4 patients.
Impedance
The times for impedance to return to its pre-bolus level after a fall during the reflux event are shown in Table 1.
Table 1: Impedance: Times for impedance to return to baseline after reflux event.
| Bolus clearance (secs) | Mean | Median | Range |
| Upright | 15.6 | 14.0 | 0-74.0 |
| Recumbent | 16.5 | 10.0 | 0-167.0 |
| Total | 13.0 | 10.5 | 1.0-74.0 |
Resting impedance is typically ~ 2200 Ω and falls to ~500 Ω during a reflux event [22,23]. Normal bolus clearance has been reported as less than 5 seconds [22]. Total bolus clearance was abnormal in 48 of the 60 patients.
pH/ Impedance. Acid exposure times are shown in Table 2.
Table 2: pH: Percentage acid exposure times.
| Acid exposure | Mean | Median | Range |
| Proximal | 8.1 | 6.0 | 0-46.0 |
| Distal | 38.5 | 30.3 | 0-56.0 |
Thirty eight patients had an acid exposure time in excess of 6.3% [24]. Proximal total reflux events (acid+non-acid), were a mean of 27.5% in 24 hrs (Median 24.0, Range 2.0-104.0). Normal reflux frequency (≤ 31 in 24 hrs) [24], of all events (acid and nonacid) was found in 13 patients in the proximal oesophagus. Ten of these 13 patients were in the group of 30 with atypical symptoms in which the scintigraphic studies were abnormal and 3 were in the group undergoing fundoplication of which 2 showed aspiration of refluxate into the lungs.
Scintigraphy
No scintigraphic evidence of GORD was shown in 12 of the 60 patients. The primary symptom of these 12 patients was chronic cough without heartburn or regurgitation. Scintigraphic parameters are presented in Table 3 The time-activity curve analysis for the pharynx/ laryngopharynx and upper oesophagus are presented in Table 4.
Table 3: Scintigraphic parameters (n=60).
| Scintigraphy | Mean | Median | Range |
| Frequency (in 30 min) | 14.0 | 10.0 | 0-43 |
| Amplitude Ratio | 5.5 | 2.2 | 0-36 |
| AUC Ratio | 2.2 | 1.9 | 0-20 |
| Liquid gastric empty (min) | 20.1 | 11.3 | 15.0-45.5 |
Table 4: Scintigraphic curve analysis for upper oesophagus and pharynx/ laryngopharynx.
| Region | Grade 0 | Grade 1 | Grade 2 | Grade 3 |
| Upper Oes Up | 12 | 2 | 6 | 21 |
| Upper Oes Sup | 12 | 21 | 7 | 20 |
| Pharynx Up | 12 | 13 | 7 | 28 |
| Pharynx Sup | 12 | 12 | 2 | 34 |
The mean liquid gastric emptying time was 20.1 minutes and 23 of the 60 patients were within the normal range (Normal < 19 minutes).
Pulmonary Aspiration of refluxate was shown in 25 of 60 patients, with 15 of the 25 giving a history of atypical symptoms.
Statistical comparisons of oesophageal physiology and scintigraphy
All positive correlations between manometry and impedance pH are shown in Table 5.
Table 5: Correlations of manometry and impedance/ pH with scintigraphy.
| Correlates | Correlation coefficients | p values |
| Manometric oesophageal motility & rising Scintigraphic curves for pharynx/ laryngopharynx & upper oesophagus | Spearman 0.35 (up) 0.61 (sup) | 0.02 (up) 0.00 (sup) |
| Manometric peristalsis & Scintigraphic amplitude of reflux | Pearson 0.48 | 0.01 |
| Manometric motility & Scintigraphic amplitude (negative correlation – as motility worsened amplitude increased) | Pearson 0.45 | 0.02 |
| Impedance/ pH All recumbent reflux events (acid +non-acid) & Scintigraphic reflux frequency for the laryngopharynx/ pharynx | Pearson 0.50 | 0.00 |
| Impedance/ pH All distal reflux events (acid+non-acid) & Scintigraphic reflux frequency for laryngopharynx/ pharynx | Pearson 0.17 | 0.03 |
There was no correlation between liquid gastric emptying and any manometric, impedance, pH measures or lung aspiration of refluxate in the scintigraphic studies.
All positive correlations with lung aspiration are shown in Table 6.
Table 6: Correlations with lung aspiration in the scintigraphic study.
| Correlates | Correlation coefficients | p values |
| Manometric oesophageal motility & aspiration | Spearman 0.72 | 0.00 |
| Impedance Total bolus clearance & aspiration | Spearman 0.63 | 0.00 |
| Impedance/pH All reflux events (acid+non-acid) & aspiration | Spearman 0.45 | 0.04 |
| Scintigraphic Rising pharyngeal/oesophageal curves & aspiration | Spearman 0.41 (up) 0.38 (sup) | 0.04 (up) 0.00(sup) |
If the normal values of proximal reflux events (acid +non-acid) in 24hr impedance studies were utilised (≤ 31 events in 24 hours), 2 patients would not have been suspected of reflux with involvement of pulmonary aspiration in the cohort of 30 patients with atypical symptoms.
No acid reflux event in the distal or proximal oesophagus had a significant relationship with lung aspiration.
SPECT/ CT
The 30 patients who underwent SPECT/ CT studies of the head and neck showed refluxate contamination of the larynx and pharynx (LPR), and nasopharyngeal reflux in 20 cases. Eight of these patients demonstrated maxillary sinus contamination by refluxate and CT evidence of soft tissue disease in the sinuses. Middle ear contamination was seen in 2 patients. Moderate correlation was demonstrated between LPR / nasopharyngeal contamination of refluxate in the SPECT/ CT studies and lung aspiration (Spearman correl coeff =0.36, p=0.04).
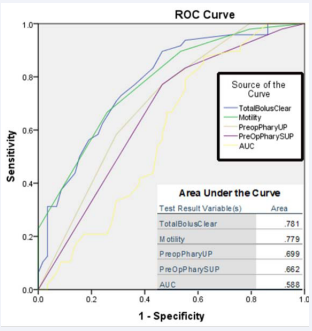
The receiver operating characteristic (ROC), curve analysis illustrates total bolus clearance, oesophageal motility, scintigraphic pharyngeal upright and supine curves and ratio of area under the curve for pharynx to background to be the best predictors of pulmonary aspiration of reflux (Figure 3).
Figure 3: ROC curve for the best predictors of aspiration of refluxate into the lungs. Total bolus clearance by impedance and oesophageal motility are the best predictors of aspiration of refluxate into the lungs.
DISCUSSION
The patients in this study illustrate a mixture of the extreme end of the GORD spectrum those with atypical symptoms such as chronic cough. It reflects the complexity and heterogeneity of disease processes under the diagnostic umbrella of GORD. The incidence of GORD is growing across the Australian population up to the age of 70 years, with the greatest increase in the 30 to 39 year age bracket [5]. This adds to the burden of disease with 50% of Australians affected by one and 23% affected by two or more chronic conditions [25,26].
The diagnostic algorithm for GORD in the presence of heartburn and regurgitation is established and validated [27]. The hierarchical diagnostic model [28], involves a PPI trial in patients whose symptoms are refractory and gastroscopy to exclude oesophagitis or other sinister pathology [27,29,30]. Endoscopy has a low diagnostic accuracy for detection of GORD with questionable utility as 50-70% of patients will have a normal study [4,28, 31]. Next in the sequence is oesophageal pH/ impedance/ manometry testing [27,29]. This diagnostic model is suitable for local oesophageal disease but sensitivity and specificity diminish with extra-oesophageal symptoms [6, 30]. It is in this group that the complexity of the medical response proliferates with an associated escalation in cost. A shift in the anatomical geography of the disease invokes referrals to otolaryngoligists, respiratory physicians and others. GORD then transmutes into a new lexicon with terms such as “laryngopharyngeal reflux” and “airways reflux”. While 24-hour oesophageal impedance/ pH monitoring with pharyngeal probes has shown promise, its reproducibility for predicting LPR has been questioned and remains an indirect investigational technique for pharyngeal or pulmonary exposure to refluxate [32].
The scintigraphic test integrates the diagnosis of oesophageal and extra-oesophageal disease by direct visualisation of refluxate at these sites. It has been validated against the current standards for detecting GORD [16,33,34], and is endorsed by Medicare.
There is a notional belief that the fundamental pathophysiology of gastro-oesophageal reflux disease is acid in spite of evidence to the contrary [35,36]. Consequently, individuals with atypical or silent reflux are relegated to alternative pathways and the risk of further chronic diseases such as pulmonary infection and fibrosis [37]. This problem is well illustrated by the cohort in this study in which 30 of 60 patients gave an atypical history of GORD. Many of these patients had normal DeMeester scores and although the mean acid exposure was 8.1%, only 38% had pH exposure above the normal cut-off level of 6.3% [24]. The preoccupation with acid exposure time(AET), is illustrated by the disparity between the distal and proximal acid exposures with a majority having significant acid exposure distally (Mean 38.5, Median 30.3, Range 0-56.0%) and only 12% recording a proximal acid exposure (pH<4.0), above 1.2% [38]. There is limited veracity in the quality of data regarding proximal AET due to variability in electrode placement [32,38,39]. It suggests significant neutralisation of acid in ascent, gaseous reflux or predominantly low-grade reflux that does not reach the proximal oesophagus [40]. The impedance data favours the former explanation as total proximal reflux (acid + non-acid) greater than 31 episodes in 24 hours [24], was recorded in 68%. These finding confirm previous work pertaining to the short-comings of oesophageal pH monitoring [41,42]. The atypical patient group may also help to explain the normality of the DeMeester scores in 12 of 30, a finding resulting from non-acid reflux events that has been reported by others [43].
Dissecting the costs involved in the detection and treatment of GORD in the Australian Healthcare system is problematic. Estimates of the prevalence are based on the typical symptoms of heartburn and regurgitation and exclude atypical symptoms [27,44].
The MBS and PBS provide the quantity and cost of GORD in the Australian population utilising publicly available Government data. There has been a marked fall in the number of prescriptions for anti-reflux medications with a disproportionate fall in the costs involved. (Graph 1)
Graph 1: Data derived from Pharmaceutical Benefits Schedule (PBS) 2012-2019 [9,10].
This variation is attributed to a series of factors:
(1) Rescheduling (prescription to over-the-counter availability) [45-48].
(2) Expiry of drug patents, resulting in a decrease in cost [45- 48].
(3) A global shift from PPI use. The frequency of reported side-effects has been questioned, but caution in long-term PPI use has been recommended [49,50].
There has been an increase in quantity and cost of diagnostic procedures from 2012-2019 (Graph 2).
Graph 2: Data derived from the Medicare Benefits Schedule (MBS) 2012-2019 [13,14].
The increase signifies the diagnostic justification of GORD within an individual [4] as recommended in Bettering the Evaluation and Care of Health (BEACH) program in 2014 [51]. Gastroscopy accounts for 84% of diagnostic expenditure despite questionable diagnostic accuracy in GORD [31].
The cost and quantity of surgical procedures have followed an incremental uniform increase over the period. Graph 3 illustrates surgical procedures over the period. Endoscopic dilatation has been excluded due to the changed classification under Medicare.
Graph 3: Data extracted from Medicare Benefits Schedule 2012-2019 [13,14].
Gross data suggests an increased prevalence of the GORD. Co-morbidities that increase the prevalence of GORD include older age, male sex, race, analgesic consumption, consumption of alcohol, smoking and BMI in conjunction with numerous other lifestyle related factors [5,52-54]. Worryingly, 67% of the Australian population is overweight or obese. Coincidently, there has been a rise in diabetes mellitus from approximately 1 to 4% between 1995 and 2018. Central abdominal obesity increases the risk of Barrett’s oesophagus, oesophageal adenocarcinoma, elevates intra-abdominal pressure promoting reflux and development of hiatus hernia [52-54].
While this data illustrates the societal and financial burden imparted by GORD, it also underlines manifold deficiencies in data collection in Australia. Data is collected via self-reporting, which is unreliable, inaccurate and has poor reproducibility [55]. Historical data is limited as GORD was consolidated under the umbrella of digestive diseases until 2014. Calculating the true burden of disease is further complicated by records held across multiple disparate databases.
CONCLUSION
Chronic diseases are the greatest challenge confronting the Australian health care system. GORD is a chronic disease with an increasing prevalence. A new diagnostic/ therapeutic algorithm must be implemented, especially in the setting of atypical GORD. This is reinforced by increasing adverse reports on the side effects of PPIs. Nuclear scintigraphy provides an innovative approach, which optimises diagnosis in the setting of typical and atypical GORD. This offers an early and cost-effective diagnostic window that allows disease prevention and risk factor management.
REFERENCES
11. MedicineWise. Top 10 drugs 2018–19. Aust Prescriber. 2019; 42: 204.
29. Richter JE. How to manage refractory GERD. Nat Clin Pract Gastroenterol Hepatol. 2007; 4: 658-664.
37. Morice AH. Airway reflux as a cause of respiratory disease. Breathe. 2013; 9: 256.
49. Yadlapati R, Kahrilas PJ. When is proton pump inhibitor use appropriate? BMC Med. 2017; 15: 36.
![Data derived from Pharmaceutical Benefits Schedule (PBS) 2012-2019 [9,10].](https://www.jscimedcentral.com/public/assets/images/uploads/image-1705662724-1.png)
![Data derived from the Medicare Benefits Schedule (MBS) 2012-2019 [13,14].](https://www.jscimedcentral.com/public/assets/images/uploads/image-1705662841-1.png)
![Data extracted from Medicare Benefits Schedule 2012-2019 [13,14].](https://www.jscimedcentral.com/public/assets/images/uploads/image-1705662899-1.png)








































































































































