Unloading Mechanical Ventilation (VUMV) with High Volume, no PEEP and little Sedation for patients with ARDS and COVID19
- 1. Clinic for Cardiology and Pneumology, University Medical Center Göttingen (UMG), Germany
Abstract
ARDS, a syndrome of various diseases with severe hypoxemia including COVID-19, is treated with low volumes, high PEEP and low pressure. Mortality is high with 30 to 50% and up to 80% during the SARS COV2 pandemia. A different strategy, to relief dyspnea with a high tidal volume, low PEEP to overventilate the patients and put their overloaded muscles at rest results in much lower mortality rates from 2 to 8%. However patients in these series might be different and randomized studies lack. In addition, actual ventilators favour the lung protective strategy, as they are underpowered to effectively support the respiratory muscles.
In addition to a randomized study comparing the unloading strategy to the lung protective, which is on the way, we designed a ventilator to meet this unloading strategy in that it automatically keeps the patient passively ventilated.
Keywords
Mechanical Ventilation, Sedation, High tidal volume, PEEP
Citation
Laier-Groeneveld G (2022) Unloading Mechanical Ventilation (VUMV) with High Volume, no PEEP and little Sedation for patients with ARDS and COVID19. J Chronic Dis Manag 6(1): 1027.
INTRODUCTION
Acute Respiratory Distress Syndrome ARDS comprises a number of different diseases, which have in common a severe hypoxemia, defined as arterial oxygen pressure over inspiratory fraction of oxygen pO2/FiO2 < 300. COVID-19 although new, is also considered as ARDS, so called CARDS.
There are numerous guidelines for the treatment of ARDS and thus COVID19 CARDS, which focus on early intubation and lung protective ventilation with prone positioning. However, many patients then die shortly after intubation and during the following treatment. Since years, and again with COVID19 disease, we offer an alternative strategy to save their lives and to spare the resources needed to treat numerous patients at the same time.
We observe two manifestations of COVID19. One is acute pneumonia with minor or no changes in chest CT scan. This disposes to acute exacerbations of chronic lung diseases and does not perform differently to exacerbations caused by other organisms outside of SARS-COV-2 pandemic. Medical treatment, oxygen and noninvasive ventilation are the standard therapy.
More threatening is COVID19 pneumonia with cellular patchy infiltrates throughout the lungs and progressive and considerable hypoxemia. We avoid to intubate such patients and treat them with high dose oxygen, high flow oxygen and noninvasive ventilatory unloading ventilation (nMUMV) to ventilate them passively and relief them from dyspnea. Only in case of cerebral confusion due to in compensable hypoxemia, we perform wakeful intubation and ventilatory unloading mechanical ventilation VUMV to completely unload the ventilatory pump. Once intubated, we use a high volume and wean them to spontaneous breathing or to noninvasive ventilation at the earliest possible time. This treatment is discussed below.
As Oxygen and CO2 are vital gases, a lack of oxygen and an increase in pCO2 are subjectively well tolerated by humans after adaptation was possible. They climb high mountains with considerably low pO2 down to 30mmHg and saturations down to 60%. In healthy individuals oxygen content is 21ml per 100ml of blood before and 18ml after extraction in the capillary bed leaving huge compensation in place for hypoxemia. In addition, oxygen delivery is more dependent on cardiac minute volume and haemoglobin than on saturation or pO2.
In consequence in COVID19 patients spontaneous breathing can be preserved up to very low pO2 pressures as long as they are not confused and cerebral and renal function remain intact. This avoids the threat of invasive mechanical ventilation to their lives.
We observe patients with severe hypoxemia due to multiple patchy pulmonary infiltrates caused by COVID19, who remain mentally adequate and improved within days from their disease. They use oxygen, high flow oxygen and noninvasive mechanical ventilation over masks but eat and drink and cough in their short periods off the machine. We therefore do not intubate until cerebral organ failure occurs and the vast majority is not intubated at any time.
Intubation in such situation is critical. If sedatives are given in order to intubate, they instantly deteriorate in saturation and mechanical ventilation must abruptly take over complete ventilation. As patients are already mentally compromised minimal or no sedatives are necessary until the tube is in place. This avoids rapid desaturation when their respiratory efforts abruptly cease following full sedation. Mechanical ventilation should augment patient´s respiration immediately after intubation with a high ventilatory rate, short inspiratory time and a high tidal volume. Sedation should be introduced carefully to smoothen the transfer from spontaneous to mechanical ventilation and to carefully install ventilatory unloading mechanical ventilation (VUMV) to relief their dyspnea. If not patients severely deteriorate in gas exchange, develop profound acidosis and die from acute ventilatory failure as reported in many intubated COVID19 patients.
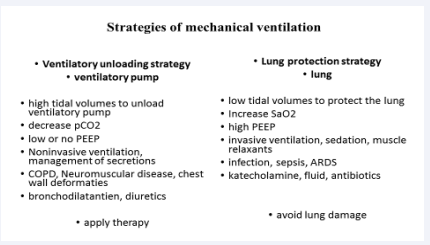
If then mechanical ventilation is inevitable, the ventilatory strategy must be determined. Two mutually exclusive ventilatory strategies are used:
• The lung protective strategy is performed with a low tidal volume, usually 6ml per kg of ideal body weight, with a ventilation pressure below 30mbar, and a high PEEP. The increase in pO2 is the target of this strategy
• The ventilatory unloading strategy of mechanical ventilation (VUMV) uses much higher tidal volumes and sufficiently high inspiratory pressures to drive the arterial pCO2 below 40mmHg together with little or no PEEP. It is set to unload the ventilatory pump and to improve spontaneous breathing capacity by improving ventilatory function. This is the strategy we propose.
The lung protective strategy of mechanical ventilation was introduced in times when large fluid volumes were given in response to a low blood pressure called fluid resuscitation. Fluid increases tissue pressure in the lung and can cause airway closure by dissemination of fluid into the alveoli. Fluid is responsible to PEEP and changing body position to increase pO2 but also to diuretics. It was assumed that ventilation causes trauma to the lung followed by progressive lung failure. The thesis has mainly been investigated in ARDS syndrome with an excessive fluid congested lung [1,2]. During expiration the alveoli were assumed to collapse due to the interstitial fluid load. Each mechanically initiated breath then requires a high reopening pressure, which causes stress to the lung tissue named stretch and strain. A high PEEP is set as it does not allow the airways to close. A low tidal volume together with low inspiration pressure are intended to prevent barotrauma and protect the lung from damage. However, by scientific evidence, volume resuscitation strategy has changed to volume deresuscitation and cellular infiltrates as in COVID19 do not respond to PEEP or changes in body position. We therefore do not use this strategy in COVID19, neither the lung protective strategy or PEEP nor prone positioning of the patient. They require huge sedation sometimes relaxation to be tolerated followed by a high mortality from hypotensive ventilatory failure.
The ventilator unloading strategy, which we prefer in COVID19, treats the overloaded ventilatory muscles and relieves failure of the ventilatory pump and by this respiratory distress. It has been established in neuromuscular disorders where the lungs are not affected and only the muscles are weak and overloaded. Ventilatory unloading results in a normal pCO2 during ventilation, a normal pCO2 during spontaneous breathing, in improved breathing capacity, in an increase in quality of life and in longevity. Most evidence exists in COPD. The load is high, to overcome intrinsic PEEP and to provide an increased tidal volume. The inspiratory pressure reserve is decreased by severe lung hyperinflation and by shortening of the inspiratory muscles [3]. In a multicentre study we could demonstrate a mortality reduction from 33% to 12% in initially hypercapnic COPD per year [4-6] (Figure 1-3).
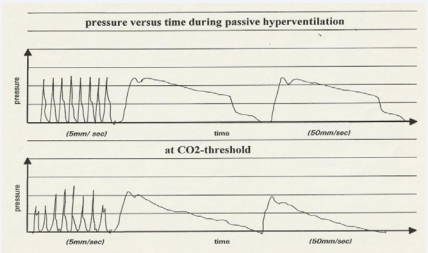
Figure 1: The lung protective and ventilatory unloading strategy of mechanical ventilation are completely opposite. Before to start with mechanical ventilation the strategy has to be determined. We porpose a ventilatory unloading startegy in all patients with COVID19. It shows the pressure time curves of a mechanical ventilated patient in a volume preset mode of ventilation. Below the apnoea threshold (above) with a totally passive ventilation to avoid any need for sedatives. There are no patients efforts. Little above the apnoea threshold (below) irregular ventilatory efforts of the patient interfere with ventilation. Dyspnoea increases and requires sedatives to tolerate as soon as a critical threshold is reached or when asynchrony occurs.
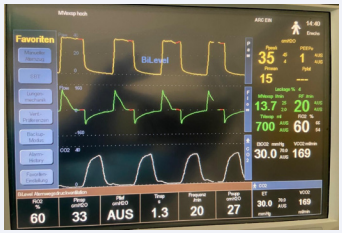
Figure 2: The ventilator mode and setting we used in our COVID19 patients.
Figure 3: The proposed strategy in COVID19.
Patients, suffering from COVID19, are dyspnoeic and severely hypoxic. Mechanical ventilation can unload the respiratory muscles completely, relieve their dyspnoea and decrease the pCO2 to normal. This occurs because the elimination of CO2 is only dependent on alveolar ventilation. The diffusion capacity of CO2 is 20fold higher compared to oxygen and its solubility in fluid is 25fold better. Therefore, in reality the transport of CO2 within the blood from the tissue to the lung and the diffusion of CO2 from the blood into the alveoli is not a limitation as long as blood circulation is active. The arterial pCO2, while breathing spontaneously, only depends on the alveolar ventilation provided by the respiratory muscles. During mechanical ventilation, pCO2 is a consequence of the decision of the therapist, as he sets the ventilator and determines alveolar ventilation. In conclusion, hypercapnia is not a consequence of lung disease but a result of ventilatory pump failure. Any increase in alveolar ventilation will result in a decrease of arterial pCO2. Every patient can be ventilated to a normal pCO2, both by invasive and non-invasive means [3]. Dyspnea is dependent on the action of the respiratory muscles. If the patient does not breathe, he does not experience dyspnea. Dyspnea is highly related to the patient´s effort to breathe (Criee). There is an apnoea threshold, usually more than 4 mmHg below the patient´s pCO2 [5]. He then stops to breath when mechanically hyperventilated as soon as this threshold is reached. We extensively reported the technique of ventilatory unloading, the ventilators used and how the modes are set in Chapter 2 in Esquinas: Mechanical ventilation.
Oxygen by contrast is largely present in ambient air (21%) and can be further augmented by oxygen supplementation to the inspiratory air. Oxygen supply is therefore not limited by the ventilation of the lung. Oxygen has a 25 fold lower diffusing capacity than CO2 through the alveoli blood barrier. Impairment of diffusion will always interfere with oxygen uptake. Haemoglobin packed in red cells is required to make oxygen transport to tissue possible, as solubility in fluid is minimal. In summary, oxygen supply in contrast to CO2 removal is largely dependent on diffusion and ventilation perfusion match in the lung as well as on the transport capacity (minute volume and haemoglobin) of the blood. Hypoxemia therefore can be treated with oxygen and high flow oxygen. But thereafter hypoxemia has to be tolerated until relief. Only complains as dyspnea can be treated by VUMV noninvasively or invasively until disease resolves.
Preference of a ventilatory strategy: As described above, prevention of airway collapse and tissue stress during instant reopening is the pathophysiological rationale for lung protective ventilation. In real life, however, this phenomena rarely occurs. Of course, if tissue pressure is high, which is the case in highly over floated lungs due to left heart failure or other capillary leak syndrome (ARDS), such alveolar collapse can occur. High dose diuretics and short time CPAP as needed or pressure support can often rapidly correct this phenomena in cardiac lung edema.
A considerable proportion of patients with ventilatory failure suffer from COPD. COPD is characterized by airway obstruction. The airways usually close before full expiration has occurred, providing an increased end expiratory alveolar volume called volumen pulmonum auctum or increased end expiratory pressure, intrinsic PEEP. With either mechanism of intrinsic PEEP, airway closure before the end of expiration or the necessity to inspire before expiratory flow has ceased due to dyspnea the alveoli are kept open if not extended. The presence of emphysema with irreversible enlargement and destruction of the alveolar air space will also make a collapse of the alveoli impossible. All COPD therefore have to be excluded from lung protective ventilation due to a different pathophysiology without a risk of alveolar collapse. They instead suffer from extensive dyspnea due to a high load on the inspiratory muscles to overcome intrinsic PEEP. They struggle to provide the increased tidal volume, with their inspiratory muscles extensively shortened by emphysematous over inflation. Such ventilatory over load can, however, be fully addressed by the unloading strategy of mechanical ventilation. If the ventilator load is taken over by the respirator, the patient’s complaints will instantly disappear. This is a major reason for the success of non-invasive ventilation and its considerable benefit on mortality through this disease. Symptoms and ventilatory failure can be improved and hazardous effects of intubation, sedation and inactivity can be avoided. Not only COPD but all patients requiring mechanical ventilation experience an increased respiratory drive and an increased inspiratory load, making them candidates for the ventilator unloading strategy. No randomized comparison of the two strategies has been performed so far. We could show in 20 patients that a transfer from lung protection to ventilatory unload does not produce any negative effects but requires less sedatives, allows more spontaneous breathing, results in better cardiac stability and increased diuresis [7,8]. In a single case study a transfer from non-invasive ventilatory unload to invasive lung protection resulted in severe hypercapnia, severe acidosis, high sedative requirement, a fall in blood pressure with the consequence of catecholamine administration, fluid resuscitation and progressive renal failure [9]. This year we reported on a huge number of patients with different respiratory disorders. Guidelines still propose lung protective ventilation in several disorders. By contrast, we always use the unloading ventilatory strategy with any patient [10], and reserve the lung protective strategy for those who are severely overloaded with fluids and only until the diuresis is initiated.
The unloading ventilatory modes: Mechanical ventilation can increase the inspiratory tidal volume until the patient is totally ventilated by the machine. Once the apnoea threshold of CO2 is reached, spontaneous breathing efforts cease both with invasive ventilation and with non-invasive ventilation via masks. The apnoea threshold of the respiratory centre usually is reached at 4 mmHg below the spontaneous PCO2 in the normocapnic and up to 7mmHg below spontaneous pCO2 in the hypercapnic patient [10]. If the threshold is reached, respiratory drive decreases, ventilatory effort ceases and passive controlled mechanical ventilation is in place. This is why passive unloading mechanical ventilation is possible even without any sedatives. Patients with severe respiratory distress as during a life threatening asthma attack will also be ventilated comfortably beyond the apnoea threshold [11].
We treated 4 patients with the unloading strategy after they were treated with lung protective ventilation and prone positioning for 2 to 14 days. They were transferred from Alsace, France to our unit. PEEP was decreased to 4mbar which resulted in a significant increase in tidal volume. With a ventilator frequency near 18 per minute and an inspiratory time of 1.4 s and the elevation of ventilation pressure up to 35mbar and more a pCO2 below 35mmHg was obtained. FiO2 was tailored down to an Sa02 of 93%. Then sedatives were completely withdrawn as the patent was passively ventilated. Catecholamines could be reduced and withdrawn in 3 within the following hours. After a 30 min T piece trial patient one was extubated 20 hair after arrival. Patient 2 sustained the breathing trail but did not yet awake from long their sedation. Patient 3 and 4 are passively ventilated and perform twice daily breathing trials in preparation for Extubation. Up to now no one died (Table 1).
Table 1: Ventilation parameters and measurements upon arrival and after having changed the ventilatory strategy.
| Upon arrival | After having changed the settings | |||
| mean | SD | mean | SD | |
| FiO2 | 0.44 | 0.13 | 0.35 | 0.1 |
| PEEP (mbar) | 11 | 2 | 2 | 2 |
| Tidal volume (ml) | 426 | 39 | 840 | 31 |
| Inspiratory pressure (mbar) | 16 | 1.5 | 31 | 2 |
| pH | 7.42 | 0.04 | 7.48 | 0.04 |
| PaCO2 (mmHg) | 45 | 9 | 34 | 2 |
| SaO2 (%) | 96 | 3 | 93 | 1 |
| PaO2 /FiO2 | 195 | 35 | 205 | 28 |
Once intubated we use VUMV with no or little sedatives and perform T piece trial twice daily in order to extubate as early as possible either to spontaneous breathing or to intermittent noninvasive ventilation.
In summary we observe 2 manifestations of COVID19: Tracheobronchitis with the risk of COPD exacerbation and COVID19 pneumonia with progressive hypoxemia.
We manage them both symptomatically and with medical treatment of the diseases prevalent, especially COPD and fluid overload.
We avoid intubation until mental confusion makes intubation inevitable despite very severe hypoxemia. We use oxygen, high flow oxygen and early noninvasive VUMV until complaints improve.
A RANDOMIZED STUDY
A randomized study between these two strategies lung protection and ventilatory unload is urgently needed, to define the best strategy in different situations in order to decrease this unacceptable high mortality and to prevent such functional deterioration inevitably occurring with long term sedation.
A MECHANICAL VENTILATOR FOR THE VENTILATORY UNLOADING STRATEGY
Most existing ventilators support lung protection as pressures are limited and flow and pressure develop slowly, not to stress the lung. Thus, ventilatory support is difficult with these devices.
We develop new ventilators which in addition to the existing modes, are capable to overventilate the patient and automatically keep him overventilated below the apnea threshold. He then is comfortable and free of dyspnea with normal gases and normal acid base balance. Little or no sedatives are needed if he consistently remains passively ventilated. Therefore rapid detection of spontaneous breathing attempts and immediate response generated by a highly flow powered ventilator is needed. The concept has been developed and studied for years. COVID19 pandemic however has provided interest in such development. If there was no or only limited intensive care mortality in COVID-19, the whole strategy of SARS-COV-2 prevention would change.
PROPOSED TREATMENT STRATEGY IN COVID-19 VIRUS PNEUMONIA
If hypoxaemic (gas exchange failure)
Increase oxygen supply by nasal canula, by high flow heated oxygen and do not intubate unless mental dysfunction occurs
If dyspnoeic with high breathing frequency (ventilatory failure)
Use noninvasive ventilatory support for several hours with high tidal volume, low PEEP, low pCO2 to relieve dyspnoea, decrease breathing frequency and unload the ventilatory muscles. Avoid intubation and increase noninvasive support in time and intensity as needed.
ONLY INTUBATE, IF SUFFICIENT SUPPORT IS NO MORE TOLERATED AND PCO2 INCREASES
Continue invasive ventilation with high tidal volumes, little PEEP and low pCO2 to avoid or minimize sedation.
Transfer to tracheotomy to provide passive non sedated ventilation with periods of spontaneous breathing to await recovery. Keep cooperativity and activity perceived.
REFERENCES
8. Laier-Groeneveld G, Krause K, Abazed Y. Which ventilatory strategy: ventilatory unload or lung protection A case report. Pneumologie (German). 2017.
12.Othman F, Laier-Groeneveld G,Brinkmnn K, Toukmaktsi S. Atmungsentlastung ode Lungenprotektion - welches Beatmungsziel. Pneumologie (German) 2020, S1: S34.
13.Laier-Groeneveld G, Othman F, Toukmaktsi S, Wiemann J. Das Multiorganversagen könnte therapiebedingt sein. Pneumologie (German). 2020; S1: S35.
14.Koerber W, Laier-Groeneveld G, Criée CP. Problems with intermittent noninvasive ventilation. Atemwegs- Lungenkrkh.(German). 1997; 23.