A Swollen Red Leg: Sweet
- 1. Dermatology Resident, Universidad Tecnológica Equinoccial, Quito, Ecuador
- 2. Department of Dermatology, Hospital Carlos Andrade Marín, Universidad Central del Ecuador, Quito, Ecuador
- 3. Department of Dermatopathology, Hospital Carlos Andrade Marín, Universidad UTE, Quito, Ecuador
Abstract
Neutrophillic dermatoses comprise a range of conditions where the hallmark is histologic infiltrate of neutrophils. Ranging from skin disorders such as acute generalised exanthematous pustulosis or subcorneal pustulosis (Sneddon Wilkinson) which affect the epidermis, the neutrophilic infiltrate can affect the dermal portion such as in Neutrophillic urticaria, Sweet’s syndrome, or eccrine neutrophilic hidradenitis, or it can affect both epidermis and dermis such as in pyoderma gangrenosum. Many times the diagnosis of a neutrophilic dermatosis poses a challenge as the main differential are infectious diseases and a high degree of suspicion needed. Generally, the diagnosis is reached with clinical and dermatopathology correlation. We present the case of an 87-year-old woman with swollen red leg in whom the diagnosis posed a challenge
Keywords
• Sweet
• Neutrophilic dermatosis
• Neutrophil
• Case report
CITATION
Cueva A, Posso V, Caceres P, Felix C, Jaramillo J, et al. (2024) A Swollen Red Leg: Sweet’s Syndrome. J Dermatolog Clin Res 12(1): 1160.
ABBREVIATIONS
ESR: Erythrosedimentation Rate; G-CSF: Granulocyte Colony Stimulating Factor; GM-CSF: Granulocyte’Macrophage Colony Stimulating Factor
INTRODUCTION
Neutrophilic dermatoses enclose disorders where neutrophils affect either the epidermis, the dermis or both [1]. The clinical features are many times similar to infectious diseases, thus high clinical suspicion is needed and diagnosis sometimes is only reached after histological and clinical consensus [2]. It is important to diagnose these diseases accurately so that prompt treatment ensures an adequate response and follow up.
CASE PRESENTATION
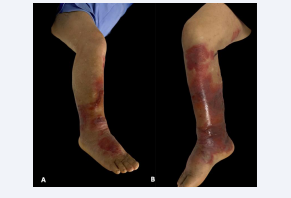
An 87-year-old woman presented to the emergency department at Hospital Carlos Andrade Marin in Quito, Ecuador with a 7-day history of fever and right leg pain for which she had received antipyretics. The leg continued swelling and blisters appeared in the lower portion. Upon physical examination she presented six well-defined erythematous plaques ranging from 2 to 14 cm in diameter affecting the lower right calf, ankle and foot; within the plaques, several bullae containing serohaemorrhagic fluid could be seen. (Figure 1A,B).
Figure 1: Erythematous-violaceous plaques with blisters and bullae within localised in the right lower leg.
A). Lateral view right lower leg.
B). Medial view right lower leg.
On laboratory examination: Leucocytosis of 19.82 x103, neutrophils of 90.9% and D-dimer of 3467 were observed. With the clinical and laboratory findings a diagnosis of cellulitis was made; yet, tissue cultures and biopsy were taken. The patient was placed on antibiotics (ceftriaxone, clindamycin); as no improvement was noted, she was switched to broad-spectrum antibiotics (vancomycin and piperacillin/tazobactam).
A subsequent examination revealed leucocytosis of 27.86 x103, neutrophils of 93.8% and Erythrosedimentation Rate (ESR) of 60 and worsening of the lesions (Figure 2). An ultrasound of the leg reported diffuse oedema, no intralesional gas bubbles and no blood clots within vessels.
Figure 2: Worsening of the lesions affecting the right lower leg.
A diagnosis of neutrophilic dermatosis, Sweet Syndrome variant, was highly suspected. Thus, the patient was started on methylprednisolone 250mg IV, with which the lesions, leukocyte and neutrophil count improved rapidly. The patient fulfilled criteria with the biopsy report of neutrophilic infiltration, and sudden appearance of lesions, coexisting fever, ESR above 20.
DISCUSSION
Neutrophilic dermatoses enclose several conditions in which there is an abundant infiltrate of these cells within the skin. Sweet syndrome was first described in 1964 [3] and it is considered a hypersensitivity reaction with an abnormal secretion of IL-1, Granulocyte and Granulocyte/Macrophage Colony Stimulating Factor (G-CSF and GM-CSF), and interferon γ. It is most common in women ages 30 to 50 and can be related to haematological malignancies, preceding infection, or drugs [4]. Several variants of Sweet syndrome have been described; three aetiology variants can be recognised: classic, malignancy-related, and drug-induced. Clinical variants include bullous, cellulitis-like, necrotising, neutrophilic dermatosis of the hands, pustular generalised, and neuro-sweet. Histology variants include criptococcoid, hystiocitoid and subcutaneous variants. Hystiocitoid variant is more related with malignancies [5].
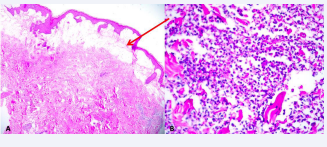
Dermatopathology describes dense neutrophilic infiltrate in the reticular dermis and sometimes perivascular, papillary dermal oedema and sometimes blister formation. Sometimes vasculitis, leukocytoclasia, and red blood cell extravasation possibly due to liberation of noxious contents from neutrophils, as it is seen in our case (Figure 3). Treatment is based on corticosteroid therapy, and when long term management is needed, potassium iodide, colchicine, indometacine, dapsone, cyclosporine, tetracyclines, and others have been described [1,2,5].
Figure 3: A). Arrow: extensive papillary dermal oedema. B). Dense neutrophilic infiltrate with extensive areas of oedema and leukocytoclasia
CONCLUSION
The diagnosis of neutrophilic dermatosis requires a high index of suspicion, as the clinical cases can be confused with infectious aetiologies and thus management can be delayed worsening the clinical course. One must always be mindful that these diseases will always be in the differential diagnosis of cellulitis, erysipelas, bullous and even pustular skin lesions.
Conflicts of Interest
The authors declare no conflicts of interest.