Tumoral Calcinosis Involving the Airway
- 1. Department of Otorhinolaryngology and Facial Plastic Surgery, University of Michigan, USA
- 2. Department of Pathology, Wayne State University, USA
Abstract
We present a unique case of tumoral calcinosis (TC) with airway involvement and a novel technique for debridement. TC is a rare disorder, characterized by calcified tumors and dysfunction of large joints. To date there have been no reports of calcification involving the airway. CD is a 43 year old male with a long history of TC who developed dysphagia prompting otolaryngic evaluation. He was found to have frank calcifications and soft tissue hypertrophy of the supraglottis causing aerodigestive tract obstruction. CO2 LASER, along with tracheotomy, was used to ablate the lesions; resulting in complete resolution of dysphagia and re-establishment of a safe and functional airway.
Keywords
• Tumoral Calcinosis
• Calcinosis Cutis
• Airway
• CO2 LASER
• Dysphagia
Citation
Kelley B, Vandjelovic N, Neil D, Dworkin-Valenti JP, Amjad E (2016) Tumoral Calcinosis Involving the Airway. J Ear Nose Throat Disord 1(1): 1011.
ABBREVIATIONS
CT: Computed Tomography; TC: Tumoral Calcinosis; CRP: C-Reactive Protein; MSDL: Micro Suspension Direct Laryngoscopy
INTRODUCTION
TC is a rare disorder of unknown etiology, typically affecting tissues around large joints, without involving the joints themselves. It is considered a type of idiopathic calcinosis cutis; a calcification of soft tissues in the absence of tissue injury or an underlying metabolic disorder [1]. Subcutaneous calcified masses appear in periarticular regions, classically beginning in the first or second decade of life, sometimes causing debility and requiring surgical removal. There seems to be no sex predilection [2]. Patients of African descent are preferentially affected; however, nearly all races and demographics have been described [2]. There are sporadic and familial forms of the disease. In some familial cases serum phosphate will be elevated without compensatory decrease in 1, 25-dihydroxycalciferol, suggesting an error in Calcium-Phosphate-Vitamin D metabolism. These cases are designated as Hyperphosphatemic Familial Tumoral Calcinosis, and have been shown to result from mutations in any of three genetic loci (FGF23, KL, GALNT3). There is also a normophosphatemic familial form resulting from abnormalities in SAMD9, a tumor suppressor gene. The etiology of sporadic cases has yet to be identified [8].
Approximately 250 cases have been reported in the world literature [3]. Of these, the most commonly involved structures include the hip, elbow, shoulder, foot, wrist, and temporomandibular joint [1]. Twelve cases have been reported with upper airway symptoms; however no accounts of airway tumors or airway intervention have been published [2].
Medical management for TC includes a diet low in calcium and phosphorus, various oral agents for phosphorus depletion, and anti-inflammatories [4]. A case study of four family members treated with phosphate binding antacids and diets low in calcium and phosphorus resulted in sustained reduction of tumor size with eight years follow up [5]. A report of eight subjects with differing manifestations showed variable response to therapy with “phosphaturia-inducing therapies”, low phosphate diet and phosphate binders. One of these patients achieved complete resolution of a single mass; two others were also treated with Interleukin-2, which normalized elevated CRP and greatly reduced joint inflammation and pain in both patients [6]. Overall treatment results are mixed, and many patients have no response to medical management [4].
CASE PRESENTATION
This patient is a 43 y/o male with history of TC, status-post resection of tumors and radiation therapy to the chest, shoulder, elbows and neck. Seven years later he presented to the emergency department with symptoms of chronic hoarseness and dysphagia to liquids persisting for two months. He related no family history of TC. Flexible laryngoscopy revealed right lateral pharyngeal wall swelling and associated calcifications. The epiglottis was deviated to the right, and the laryngeal inlet was obstructed from view. Serum calcium was normal at 10mg/dL. The patient had a notable history of mildly elevated serum phosphorus levels (5.1- 7.2 mg/dL [normal range 2.3-5.0]). A modified barium swallow showed penetration and silent aspiration with both thin and thick liquids. Computed tomography (CT) of the neck and thorax demonstrated complete obliteration of the airway secondary to mass effect from a calcified tumor in the right supraglottis, extensive mucosal thickening from nasopharynx to subglottis and extensive calcinosis involving the soft tissues of the chest. The decision was made to intervene surgically due to the severity of these findings.
Approximately six weeks later the patient underwent elective awake tracheotomy, esophagoscopy, bronchoscopy and micro suspension direct laryngoscopy (MSDL) with CO2 LASER excision of the calcified right supraglottic mass. Intraoperatively a large exophytic mass was seen in the right supraglottic region with overlying irregular mucosa. Vocal cords were significantly edematous with soft tissue thickening and compromise of the airway (Figure 1).
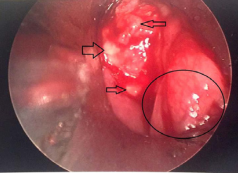
Figure 1 Intraoperative photograph showing frank calcifications (open black arrows) of the right supraglottic region with redundant soft tissue of the lateral pharyngeal wall (circled).
Pathology revealed micro calcifications and giant cell reaction without evidence of malignancy (Figure 2a,2b).
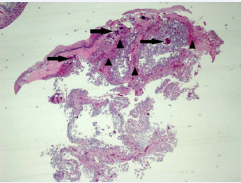
Figure 2a Supraglottic Mass Biopsy 9/24/15. Hematoxylin and eosin (H&E) stain, low power (20x magnification) view of biopsied tissue showing extensive calcification (solid arrow), increased vascularization (arrow heads point to vessel lumen) and tissue debris with overlying squamous mucosa.
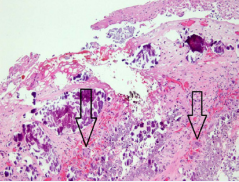
Figure 2b Supraglottic Mass Biopsy 9/24/15. H&E stain, medium power (100x magnification). At this power, multinucleated giant cells are visible (outline arrow). Calcification, increased vascularization, and cellular debris are conspicuous
The patient was discharged on postoperative day five and was decannulated in clinic one month later. Two months postoperatively his dysphagia resolved completely, but the preoperative hoarseness remained unchanged. Flexible nasopharyngolaryngoscopy revealed mildly redundant mucosa of the right arytenoid cartilage and mild fullness of the right lateral pharyngeal wall, neither of which caused airway obstruction. The right true vocal fold was fixed in the paramedian position, but complete mobility of the opposing vocal fold enabled adequate glottal airway dimension both at rest and during respiration. Repeat CT of the neck showed a moderate decrease in supraglottic soft tissue asymmetry, absence of the offending calcified tumor and a patent airway (Figure 3a,3b).
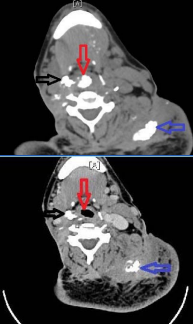
Figure 3 3a-3b (Top-Bottom): 3a: Preoperative Neck CT showing right supraglottic calcified mass (open black arrow) and airway obstruction from central supraglottic mass (open red arrow). 3b: Postoperative Neck CT showing absence of prior obstructing calcified mass and patent airway (open red arrow). There is slight reduction in size of right supraglottic mass (open black arrow). Preexisting calcified mass of left shoulder is seen in both images (open blue arrow).
The pt was asked to return to clinic on an “as needed” basis.
DISCUSSION
TC is considered a benign yet potentially debilitating condition, and its underlying pathophysiology has yet to be completely elucidated. There are sporadic and familial forms of the disease, with the familial forms divided into hyperphosphatemic and normophosphatemic, each with separate genetic etilogies.8 Our patient does have hyperphosphatemia, but no history of affected family members or genetic testing, making it difficult to determine the category into which he falls.
Only a few hundred total cases have been reported in the literature, with only a small fraction involving the head and neck. There have been cases of dysphonia associated with TC although the presence of calcinosis was not proven by pathology, and no interventions were attempted [2,3]. The current patient’s airway had gross calcifications seen on CT and intraoperatively. Microcalcifications were also found on pathologic examination. To our knowledge the current case represents the first account of airway calcifications resulting from TC.
Gal et al., described six patients of Jewish-Yemenite descent with oral cavity signs and hoarseness that preceded joint manifestations of the disease; hoarseness was the earliest finding in three of these individuals. Intraoperative indirect laryngoscopy revealed thickened true vocal folds without gross calcifications or immobility [2]. Metzker et al., described 10 patients with TC [3]. Five of Jewish-Yemenite descent presented with mucosal involvement and hoarseness; laryngoscopy revealed thickened vocal cords without gross calcifications, though no biopsies were performed [3]. None of the 5 patients of non-Jewish origin had hoarseness or mucosal involvement.
Calhoun et al., described an African American male with neck manifestations of TC [4]. Six of his fourteen siblings were also affected in large joints but not the head or neck region. In this male patient a 12X16cm neck mass explained his limited range of motion. A neck CT revealed calcific deposits from the mastoid tip to the clavicle. Intraoperative exam showed cystic structures containing amorphous chalky paste, and a pseudo-capsule. There was improvement in range of motion after the de-bulking procedure. The authors did not report whether the patient suffered from hoarseness or laryngeal pathology.
The current patient’s persistent dysphagia and airway compromise required surgical excision of the offending mass using CO2 LASER via MSDL, on the continuous setting with 4 watts of power. Cup forceps were used to debulk all redundant soft tissue. To our knowledge this is the first published example of CO2 LASER utilization for a TC lesion.
The patient required concurrent awake tracheotomy due to near complete airway obstruction from the disease process, and to ensure a safe airway postoperatively. After excision the patient was decannulated without complication. Follow up flexible laryngoscopy revealed improvement of the airway and right vocal cord fixation in the paramedian position. Because of bulky disease preoperatively the status of vocal fold disease could not be determined. We suspect his presenting hoarseness was likely a manifestation of existing vocal cord paralysis. His acute airway symptoms resolved with excision of the calcific lesions; vocal cord paralysis persisted. Notwithstanding associated dysphonia, the patient’s swallowing difficulty improved postoperatively, enabling a normal diet. At two months follow-up, voice was functional but remained hoarse.
Evidence based recommendations for treatment of airway TC are lacking. If airway involvement is severe, the role of pharmacologic intervention may be limited. Although surgical excision may produce improved airway dimensions, these types of lesions have a high likelihood of recurrence, necessitating additional surgical management. Our patient has only 2 months of postoperative follow up, and although he is doing well at this time, may require further airway intervention in the future.
CONCLUSION
TC is a benign, indolent condition of unknown etiology that typically affects tissue around large joints. To our knowledge our patient may be the first case of airway obstruction owing to gross calcifications. Our treatment approached involved use of CO2 LASER debridement and tracheotomy, with subsequent successful decannulation one month postoperatively. Consensus of optimal therapy for this condition has not been established. However, when the airway is significantly affected, surgical debridement may be the most advantageous approach to management and symptom resolution, as in our case. This novel application of CO2 LASER was safe and effective, and deserves further study in the treatment of these patients.
ACKNOWLEDGEMENTS
Benjamin Kelley DO: Lead Author, Corresponding Author
Nathan Vandjelovic DO: 2nd Author, Surgical 1st Assist
Daniel Neil MD: Chief Resident Pathology, Photomicrographs with annotations
James P. Dworkin-Valenti: Research Advisor, Manuscript Editing
Esmael Amjad MD: ENT Faculty, Primary Surgeon









































































































































