Assessment of Pro-Inflammatory Serum Cytokines in Patients with Type II Diabetes Mellitus with Non Healing Foot Ulcer in North India
- 1. Department of Medicine, Institute of Medical Science, Banaras Hindu University, Varanasi, India
- 2. Faculty of Health Sciences, Department of Microbiology, Immunology and Genetics, Ben Gurion University of the Negev, Beer Sheva, Israel
- 3. Department of Dental Science, Institute of Medical Science, Banaras Hindu University, Varanasi, India
Abstract
Aim: To evaluate IL-6 and TNF-α concentration in the serum of type 2 diabetes mellitus (T2DM) with and without foot complications.
Materials and methods: We recruited 100 subjects with T2DM having foot ulceration (group C), 100 subjects with T2DM without foot ulceration (group B) and 100 healthy control without any history of diabetes mellitus and foot ulceration (group A). IL-6 and TNF-α serum levels were evaluated by Enzyme-linked Immuno Sorbent Assay (ELISA).
Results: IL-6 and TNF-α levels were significantly higher in the serum of group C as compare to group B and group A (p25).
Conclusion: In conclusion current study revealed that the excessive presence of IL-6 and TNF-α might play a role in diabetic foot ulcer pathogenesis and delayed wound healing.
Keywords
- Interleukin-6
- Tumor necrosis factor-α
- Type2 diabetes mellitus
- Diabetic foot ulcer
Citation
Tripathi K, Yadav SK, Arya AK, Tripathi R (2017) Assessment of Pro-Inflammatory Serum Cytokines in Patients with Type II Diabetes Mellitus with Non Healing Foot Ulcer in North India. J Endocrinol Diabetes Obes 5(3): 1108.
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is one of the fastest growing non communicable diseases (NCDs) globally including developing countries and South East Asia [1]. Among all other diabetes complications, diabetic foot ulcers are more common and 60– 80% will heal, whereas 10-15% of them will remain active, and up to 24% of them will finally lead to lower extremity amputation [2]. Prolonged hyperglycemia increases the prevalence of foot ulcers ranges from 4 to 10% and its lifetime incidence may be as high as 25% [3].
Lower extremity ulceration is characterized by exaggerated and prolonged pro inflammatory reactions with a significant mutilation in confined bacterial invasion control. Tumor necrosis factor (TNF-α) enables homing of inflammatory cells, triggers pro-apoptotic gene and repair epithelium [4]. Presence of several characteristic diabetic foot pathologies such as infection, diabetic foot ulcer and neuropathic osteoarthropathy further leads to the risk of cardiovascular diseases [5]. To raise awareness about this disease International Diabetes Federation declared year 2005 to foot care of people with diabetes neuropathy. Foot ulcer progress in the four sequential steps which are peripheral neuropathy, deformity, peripheral vascular disease and injuries [6].
Leukocyte migration into wounded area is stimulated by collagen, elastin breakdown product, element factor and immune response mediated by immune modulator factor including TNFalpha, interleukin-6 (IL6), platelets derived growth factor (PDGF), transforming growth factor (TGF-beta). All leukocytes require activation before they can perform their vital function in wound environment [7]. Hyperglycemia has been shown to induce pro-inflammatory cytokine progression and chemokine gene in monocyctic cells [8]. A pro-inflammatory cytokine promotes systemic inflammation. Chronic low-grade inflammation and activation of the innate immune system were closely involved in the pathogenesis of Diabetes and its microvascular complication including neuropathy, retinopathy and nephropathy [9]. IL6, TNF-alpha and IL1beta were major mediator of pro inflammatory cytokine in the induction of acute phase response in the diabetic foot [10,11].
MATERIALS AND METHODS
This Immunological based study was conducted in Department of Medicine, Institute of Medical Science, Banaras Hindu University, Varanasi, India. All procedures performed in this study involving human participants were in agreement with the ethical standards of the Institutional Research Committee, Faculty of Medicine, Institute of Medical Science, Banaras Hindu University, Varanasi India. The study was carried out in accordance with the principles of the Declaration of Helsinki and received written consent from all participants to take part in the research. Foot ulcer was defined as a full-thickness skin defect that required ≥ 14 days for healing. A physical examination with prominence on the lower limbs was performed by research operators, who assessed the presence of the following characteristics: hammer/claw toe, Charcot deformity, hallux limitus, prominent metatarsal heads, hallux valgus, bony prominences, and ankle in all participants.
A total of 300 participants were divided into three groups. Group A contains One hundred healthy volunteers (65 male and 35 female) which are not having any history of T2DM whereas group B contains one hundred T2DM patients (37 male and 63 Female) without diabetic foot. Group C contains one hundred T2DM patients with chronic non healing diabetic foot complications (48 male and 52 female).
Patients involved in this study were gone through detail clinical history and physical examination. This included age, sex, duration of diabetes, symptoms suggestive of diabetes mellitus and family history of diabetes. Physical examination included anthropometric measurements such as, height, weight, body mass index and waist circumference. Subjects were also investigated for baseline study parameters (Table 1).
Table 1: General Demographic detail between different Groups of Diabetes Mellitus.
| Parameters | Group A (mean ± SD) | Group B (mean ± SD) | Group C (mean ± SD) | P-Value |
| AGE(Year) | 45.35±5.77 | 55.85±2.961 | 64.15±64.15 | 0.0001 |
| Duration (Year) | - | 3.85±1.872 | 5.65±3.167 | 0.0001 |
| Weight(Kg) | 52.90±5.637 | 63.55±2.139 | 71.65±4.069 | 0.0001 |
| Height(Meter) | 1.63±.036 | 1.66±.030 | 1.57±.028 | 0.0001 |
| BMI(wt./m^2) | 19.81±1.569 | 22.98±.557 | 29.03±.826 | 0.0001 |
| RBS(mg/dl) | 197.10±4.856 | 263.95±7.126 | 360.50±5.854 | 0.0001 |
| SBP(mmHg) | 118.60±11.564 | 132.95±3.471 | 155.25±11.85 | 0.0001 |
| DBP(mmHg) | 68.50±6.220 | 155.25±11.85 | 90.45±3.953 | 0.0001 |
Patients were diagnosed T2DM as per American Diabetes Association (ADA) criteria (fasting serum glucose level (? 126mg/ dl, i.e., 7.0 mmol/l) on two occasions, or an oral glucose tolerance test (OGTT) yielding ? 200 mg/dl (11.1 mmol/l) after 2 h, or symptoms of uncontrolled diabetes with a random serum glucose level ? 200 mg/dl (11.1 mmol/l) and glycosylated hemoglobin (HbA1c%) ? 6.5% from outpatient department (OPD) of Wound Clinic, Institute of Medical Sciences, Sir Sunderlal hospital, Banaras Hindu University, Varanasi, India . Blood samples were collected from the vein by venipuncture in a tube without having any anticoagulant. Serum were immediately separated by centrifugation and stored in aliquots at -80° C until analysis. Serum glucose level fasting blood glucose (FBG), postprandial blood glucose (PPBG) was estimated by glucose oxidase/glucose peroxidase method by commercial kit as per manufacture instructions (Span diagnostics, India). Concentrations of serum IL-6 and TNF-α level were determined by quantitative sandwich enzyme-linked immune-sorbent assay (ELISA) kit (R&D Systems, USA) as per manufacturer’s protocol.
STATISTICAL ANALYSIS
Results are expressed as mean ± standard deviation (SD) for different groups. The statistical significance was evaluated by One-way Analysis of Variance (ANOVA).
Newman-Keuls post hoc test was used for multiple comparisons. The differences were considered statistically significant when p-value was less than 0.05. Statistical analysis was performed using the SPSS for Windows (version 16.0; SPSS Inc., Chicago, IL).
The statistical data was analysed by statistical unit in our Institute. Mean ± standard deviation (SD) and proportion were reported for the variable due to the skewed distribution of the cytokine variable the median values and ranges were reported. The median test was used for intergroup comparisons. For further multiple groups of comparison analysis odd Variance (ANOVA) testing with honestly significant different and Chi-Quadrat Test (χ2 Test) with Yates correlation was used for comparison of proportion and <0.05 was conserved as significant.
RESULTS
In this study (Table 1) shows the demographic and clinical detail of the study. Group A subjects have 65% male and 35% Female, group B include 37% male and 63% female whereas group C includes 48% male and 52% female. According to locality in group A control subjects were 45% from rural and 55% from urban and in group B 65% Rural and 35% was urban while an equal proportion in Group c that is 50% both from Rural and urban. Regarding the Food habits in control group was 90% NonVeg and 10% Vegeterian where as in Group B were 60% non Vegetarian and 40% Vegetarian and In Group C with Diabetic Foot were 55% non Vegetarian and 45% Vegetarian. With regard to uncontrolled foot ulcer risk factors, 30% of subjects in group C and 5% of subjects in group B was a smoker and 10% consuming alcohol in both group B and group C. Regarding the Educational Graduate and post graduate was equal proportion in all three groups and illiterate proportion were higher in group C 45% as compared to 40% Group B and 20% Group A. On aspect views of occupation female were mostly housewives in all three Groups 65% were businessman and 55% were unskilled people.(Figure 1,2).
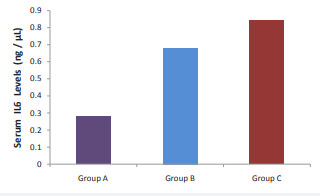
Figure 1 Showing Concentration of Cytokine IL-6 Level in Three groups of diabetic subjects.
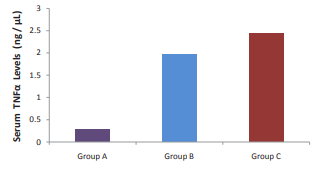
Figure 2 Showing Concentration of Cytokine TNF-α Level in Three groups of diabetic subjects.
Analysis of cytokine IL6 and TNF-α was performed on Serum sample using Enzyme linked Immunosorbent Assay commercial ELISA. Especially the expression of pro-inflammatory cytokines such as IL 6 and TNF-α show peaked early in group C diabetic foot ulcer in contrast to other group B and control group A. Analysis from different comparison of control versus and other two group and vice versa we find significant result (p<0.005) that suggest group c diabetic foot patients have higher level of Growth factor and cytokine (Table 2).
Table 2: Concentration of Cytokine IL-6 and TNF-α between different Groups of Diabetes Mellitus
| Group A (mean ± SD) | Group B (mean ± SD) | Group C (mean ± SD) | P-Value | |
| IL6 | 0.2985±.08107 | 0.6565±.11854 | 0.8122±.08946 | 0.001 |
| TNF-α | 0.2940±.03513 | 1.9757±.30155 | 2.2857±.47645 | 0.001 |
| Cytokine | (mean ± SD) | P-Value | ||
| IL6 Group A | Group B | 0.05796± 0.03089 | 0.066 | |
| Group C | 0.21367± 0.03089 | 0.0001 | ||
| IL6 Group B | Group A | 0.05796± 0.03089 | 0.066 | |
| Group C | 0.15570± 0.03089 | 0.0001 | ||
| IL6 Group C | Group A | 0.21367± 0.03089 | 0.0001 | |
| Group B | 0.15570± 0.03089 | 0.0001 | ||
| TNF-α Group A | Group B | 1.68163± 0.10314 | 0.0001 | |
| Group C | 1.99163± 0.10314 | 0.0001 | ||
| TNF-α Group B | Group A | 1.68163± 0.10314 | 0.0001 | |
| Group C | 0.31000± 0.10314 | 0.004 | ||
| TNF-α Group C | Group A | 1.99163± 0.10314 | 0.0001 | |
| Group B | 0.31000± 0.10314 | 0.004 | ||
| Abbreviations: BMI- Body Mass Index; RBS- Random Blood Sugar; SBP- Systolic Blood Pressure; DBP- Diastolic Blood Pressure | ||||
DISCUSSION
The present study have showed that IL-6 and TNF-α were significantly increased in blood Serum in type 2 diabetic foot patients with peripheral diabetic neuropathy. The results of our study suggest that inflammatory cytokines may be pathogenically important in T2DM foot patients. In T2DM patients proinflamatory cytokines playing important role in the autoimmune pathogenesis of β-cell destruction [12]. T2DM results from an immunoregulatory (repressor) mechanism in which Th1 cells and their cytokine products, IL-6, and TNF-α (Type 1 cytokines), dominate over immunoregulatory (suppressor) Th2 cells and their cytokine products, IL-4 and IL-10 [13]. Therefore, the current therapies aimed at T2DM prevention should be directed at increasing Th2 cell function and Type 2 cytokine production, and/or decreasing Th1 cell function and Type 1 cytokine production [14].
IL-6 is produced by a variety of cells such as macrophage, Th2cell, B cell, endothelial cell involved in pro inflammation. IL-6 is an important mediator of intra-skin inflammation, can amplify leukocyte recruitment. Various investigators have detected IL-6 in wound fluid from patients with diabetic foot [15]. Inflammatory processes were then likely to be involved in the pathogenesis of proliferative retinopathy in diabetes. Moreover, in a recent study, anti inflammatory cytokines such as IL-2, IL-4, IL-10, secreted from macrophage type 2 and interferon (IFN-γ) were detected in vitreous fluid in diabetic retinopathy [16]. Serum concentrations of TNF-α were reported to be eminent in diabetic patients. The source of TNF-α in human Serum is not clear. Macrophages from diabetic patients have been found to release more TNF-α than control macrophages [17]. Identification of the sources of Serum TNF-α requires further study; origin from multiple tissues including adipose tissue and macrophages appears likely. This study results then suggest the possibility that inflammatory cytokines may participate in the proliferative diabetic neuropathy of diabetes although origins and intraocular effects of these mediators require further investigation [12].
Lower extremity ulceration is a serious and chronic diabetic complication rendering a significant social burden in terms of amputation and quality-of-life reduction. Diabetic patients experience a substantial wound-healing deficit [18]. Therapeutic approaches aimed to down regulate hyper inflammation and/ or attenuate glucolipotoxicity may assist in diabetic wound healing by dismantling downstream effectors. These medical interventions were demanded to reduce amputations in an expanding diabetic population [19].
Insulin resistance has been defined as a state of inflammation involving both innate and adaptive immunity [20]. Inflammation activated by the metabolic, biochemical and haemodynamic derangements may play a key role in the development and progression of diabetic nephropathy. Cytokines such as IL1, IL-6 and TNF-α stimulate the expression of cell adhesion molecules and profibrotic growth factors, increase endothelial permeability, promote mesangial proliferation [21]. Cytokines of the IL-6 family have been shown to play a role in all stages of the development and progression of atherosclerosis, from early inflammatory lesions to destabilisation of the plaque [22]. The IL-6 signalling is activated through two different ways and it has been a matter of discussion whether this results in both a pro- and anti-inflammatory effect of IL-6. In the classical IL-6 signalling pathway IL-6 binds to IL-6R, which is a membranebound receptor on the cell surface. The receptor-ligand complex then associates with the common signal transducing receptor gp130, initiating activation of intracellular signalling path- ways. The membrane-bound IL-6R is present in cells like hepatocytes, monocytes, inactive B and T-lymphocytes [23].
The Serum IL-6 level in diabetic subjects was significantly higher than in normal healthy controls. The specific optical density of the Serum IL-6/IL-6R complex in diabetic patients was also significantly higher than in normal healthy controls, although there was no significant difference in the Serum IL-6R level between diabetic patients and controls. The Serum IL-6 concentration was correlated significantly with the HbA(1C) level by multiple regression analysis [24]. The expressions of immune markers, such as IL-1β, IL-6 and TNF-α, often were linked to the progression of type 2 DM. This, in combination with TNF-α and IL-6, may synergistically exacerbate the extent of β-cell apoptosis and disease progression [25].
The limitation of study is that falling the natural activity of pro-inflammatory cytokine can reduce the brunt of attack from chronic diseases. The suppression of IL6 and TNF-a will be reduces host disease. Due to sedentary life style, diabetic patients are also at macrovascular artery disease, which could get complicated by release of pro-inflammatory cytokine progression leading to ischemic, infection and endothelial dysfunction resulting in non healing foot ulcer.
CONCLUSION
Diabetic foot is very severe complication of diabetes increasing rapidly as frightening rate. Condensed immunity due to depletion of lymphocytes is one of the major causes of the delayed wound healing. Our experiment shows higher expression of pro-inflammatory cytokine and reduced expression of Antiinflammatory cytokine in blood Serum of uncontrolled diabetic patients having diabetic foot supports the hypothesis that hyperglycemia induced apoptosis in various cell types. These results suggest that hyperglycemia and increased levels of Serum IL-6 can increase the Serum fibrinogen concentration, one of the known risk factors for atherosclerosis in patients with Type 2 Diabetes Mellitus. Impaired diabetic wound healing and diabetic ulcer impair the quality of life of millions of people and burden the healthcare systems globally. Etiological factors involve a high level of TNF-a, which inhibits angiogenesis and cell proliferation and migration in diabetic wounds and increases apoptosis levels. TNF-α inhibition attenuates the impact of diabetes-enhanced TNF-a, which offers the potentially new therapeutic avenue for treatment of abnormally diabetic wounds healing.
ACKNOWLEDGEMENTS
We are grateful to all diabetic subjects and healthy volunteers for their wonderful cooperation during the study. Author Santosh K. Yadav is thankful to University Grant Commission for providing research fellowship Scheme No.5012 which was helpful to complete this study.









































































































































