Conversion to Armour Thyroid from Levothyroxine Improved Patient Satisfaction in the Treatment of Hypothyroidism
- 1. Gary M. Pepper, Palm Beach Diabetes and Endocrinology Specialists, University of Miami “Leonard M. Miller” School of Medicine, USA
Abstract
The use of Armour Thyroid (desiccated thyroid) in the treatment of hypothyroidism has generated debate among endocrinologists although there is evidence that a significant percentage of patients prefer this medication to T4-only replacement strategies. In this retrospective analysis we investigate the preference for replacement therapy of patients with persistent subjective symptoms of hypothyroidism on T4-only treatment who subsequently switched to Armour Thyroid (AT).
Methods: 450 consecutive patients being treated for hypothyroidism were screened. Of these, 154 had been switched from either generic or brand T4 replacement to AT for treatment of persistent symptoms of hypothyroidism. Patients undergoing treatment for thyroid cancer or on suppression therapy for nodular thyroid disease were excluded. Patients were instructed to have their blood sampled for thyroid function testing in the morning after taking their medication. After a minimum of 4 weeks on medication patients were asked to compare AT treatment versus T4-only treatment using a 5 point satisfaction rating scale. Results are reported as mean ± SD.
Results: On a 5 point Satisfaction Rating Scale with “5” indicative of the highest level of satisfaction, 117 (78.0%) patients gave a score of greater than “3” in preference for AT. Three patients treated with AT and one treated with LT4 reported adverse events, all minor. TSH was 1.30 ± 1.9 mIU/L and T3 1.81 ± 0.78 pmol/L on L-T4 monotherapy while TSH was 1.27 ± 2.2 mIU/L and T3 2.31 ± 1.33 pmol/L on AT (NS for TSH and p<0.003 for T3 ). T4 to T3 ratio on L-T4 monotherapy was 8.45 ± 3.7 while it was 4.70 ± 2.0 (p<0.001) on AT. There was no significant change in weight after switching to AT.
Conclusion: AT treatment was preferred over LT4 replacement therapy by 78% of patients with hypothyroidism in the sub-group with persistent subjective complaints while on T4-only therapy. No serious adverse events were noted while on AT treatment including 30 subjects aged 65 yrs or older. AT could be a reasonable alternative choice for treating this sub-group of patients with hypothyroidism.
Keywords
• Armour thyroid
• Levothyroxine
• Hypothyroid
• Treatment
Citation
Pepper GM, Casanova-Romero PY (2014) Conversion to Armour Thyroid from Levothyroxine Improved Patient Satisfaction in the Treatment of Hypothyroidism. J Endocrinol Diabetes Obes 2(3): 1055.
ABBREVIATIONS
TSH: Thyroid Stimulating Hormone; L-T4: Levothyroxine; T4: Thyroxine; T3: Triiodothyronine; AT: Armour Thyroid; L-T4: levothyroxine; NT: No Thyroid Disease; SRS: Satisfaction Rating Scale
INTRODUCTION
Armour© Thyroid (Forest Pharmaceuticals, St. Louis, Missouri) also known as desiccated thyroid, is an inexpensive, once daily form of T4 plus T3 hormone replacement. Many practitioners regard Armour© Thyroid (AT) as an inferior product however, to be avoided in clinical practice [1]. This could be in part due to a widely publicized report [2] of inconsistency in the thyroid hormone content of generic forms of desiccated thyroid although, in actuality, AT itself was held as a standard of consistency in that study.
In contrast, treatment of hypothyroidism with levothyroxine (L-T4) monotherapy has been the standard of care in the United States for over 3 decades [3]. This is despite the reported failure of this form of therapy to result in satisfactory resolution of symptoms in a portion of treated individuals [4]. Several groups have studied the effect of combination L-T4 and T3 as replacement therapy in an attempt to achieve better clinical outcomes. Results have been mixed [5-16] and combination therapy remains controversial.
A recent [17] prospective double blind study compared the clinical and biochemical response of a group of 70 hypothyroid patients to AT versus L-T4 monotherapy. Although ratings of quality of life were comparable between the two therapies, in a sub-group of about 50% of the study cohort AT was associated with improved subjective symptoms as measured by two assessment tools. Additionally 49% of the study group preferred AT therapy to L-T4 monotherapy. Interestingly, others report patient preference for treatment of hypothyroidism with combination L-T4 plus liothyronine compared to L-T4 monotherapy [9,11].
To investigate the observed preference of a subgroup of hypothyroid patients for AT over L-T4 monotherapy, we retrospectively reviewed the biochemical indices of patients who failed to achieve clinical euthyroidism on L-T4 monotherapy and who were switched to AT treatment. These individuals were subsequently queried as to their preference for either of these therapies.
METHODS
450 consecutive patients being treated for hypothyroidism within a single endocrinology practice were screened between February 2013 and April 2013. Of these, 154 (34.2%) had been converted to AT after apparent failure of L-T4 therapy to eliminate persistent symptoms of hypothyroidism including fatigue, cold intolerance, constipation, myalgia, and unexplained weight gain. Patients were instructed to take all thyroid replacement medication while fasting, one hour prior to breakfast. During both L-T4 monotherapy and AT treatment patients were reevaluated at regular office visits generally at 1 to 3 month intervals with repeat thyroid function testing, physical exams and clinical interviews in an effort to titrate the medication dosage to achieve relief of clinical symptoms without inducing biochemical hyperthyroidism or hypothyroidism.
TSH, total T4, total T3 levels on L-T4 monotherapy and during treatment were measured. Patients receiving post thyroid cancer replacement therapy (2 patients) or suppressive treatment for thyroid nodular disease (2 patients) were excluded from this analysis. In all others hypothyroidism developed as a result of Hashimoto’s Thyroiditis, other endogenous causes, non-cancer related thyroidectomy, or post-iodine ablation for hyperthyroidism.
Patients were asked to compare AT treatment versus prior L-T4-only treatment using a 5 point [11] Satisfaction Rating Scale (SRS). SRS is as follows: 1=AT definitely worse than LT4, 2=AT probably worse than LT4, 3= AT no different than L-T4, 4=AT probably superior to L-T4, 5= AT definitely superior to L-T4. Prior to patient interview a minimum of 4 weeks of L-T4 and AT therapy was completed, unless an adverse event occurred. In an effort to reduce interviewer induced bias questioning of subjects and recording of their response was done by a medical assistant prior to the physician’s visit.
Separately, 51 ambulatory adults without active thyroid disease (NT) undergoing routine health evaluation provided samples for total T4, T3 resin uptake, TSH and total T3 measurement. Written consent for use of clinical data was obtained from all participants. HIPAA compliant protocols for protection of the privacy of health information were employed throughout this project.
Statistical comparisons of data between treatment groups were made using a t-test for paired variables; Non parametric data were analyzed using Kruskal-Wallis one way ANOVA on ranks. Results are expressed as mean ± SD, or mean ± SEM for graphical purposes and median for time; p<0.05 is used as the threshold for statistical significance. Statistical analysis was performed using NCSS 2007 statistical program [18].
RESULTS
Characteristics of the study population are presented in (Table 1).
Table 1: Characteristics of the Study Population.
| Variables | Mean |
| Age (years) | 53.5±12.5 |
| Baseline TSH on L-T4, (µU/mL) | 1.30±1.7 |
| Baseline Serum T4 on L-T4, (µg/dL) | 8.3±2.5 |
| Baseline Serum T3 on L-T4, (pg/dL) | 1.2±0.5 |
| Baseline Weight on L-T4, (pounds) | 165.2±34.0 |
| Armour© Thyroid (AT) Dosage (mg) | 92.3±28.6 |
| Serum TSH on AT (µU/mL) | 1.35±2.4 |
| Serum T4 on AT (µg/dL) | 5.9±1.9 |
| Serum T3 on AT (pg/dL) | 1.5±0.9 |
| Weight on AT (pounds) | 163.7±33.9 |
| Serum TSH change (µU/mL) | -0.07±2.9 |
| Weight change (pounds) | 1.25±11.0 |
Abbreviations: TSH= Thyroid Stimulating Hormone, L-T4= Levothyroxine, T4= Thyroxine T3= Triiodothyronine
Of 450 patients being treated for hypothyroidism with L-T4, 154 (34.2%) had persistent complaints typical of hypothyroidism despite thyroid hormone levels in the normal or above normal range. The average age of this study group was 53 ± 12.5 years (range 24 to 86 years), 30 of these being 65 yrs of age or older and 139 were female (92.6%). Duration of prior L-T4 treatment was 6 years and 7 months (median 3 years) and for AT treatment at the time of study was 2 years and 9 months (median 2 years). Three adverse events on AT occurred; itchiness of the eyelids in one, scalp hair loss in one and palpitations in the third. Tingling and numbness of the lips while on Synthroid constituted an adverse event during LT4 therapy. AT dose at the time of study was 92.3 ± 28.6 mg.
117 (78%) patients gave a score of greater than “3” (Satisfaction Group A or Responders) vs. 33 patients with a score equal or less than “3” (Satisfaction Group B or Non-Responders) (Figure 1).
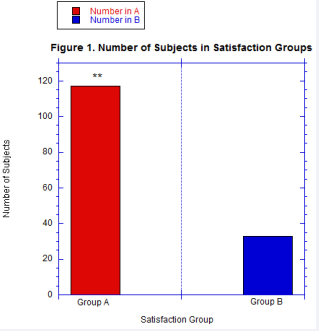
Figure 1 There were 117 patients who gave a Satisfaction Score of greater than “3”, classified as Group A/ Responders versus 33 giving a Satisfaction Score of “3” or less, in Group B/Non-responders. The mean rank Satisfaction Score for Group A was 4.79 ± 0.40 compared to 2.70 ± 0.63, for Group B, p<0.001 (**).
On a 5 point scale, with “5” corresponding to AT “definitely superior” to prior L-T4 therapy and “1” corresponding to AT “definitely worse” the average mean rank score for Satisfaction Group A was 4.79 ± 0.40, significantly greater than Satisfaction Group B 2.70 ± 0.63 , P<0.001. T4 to T3 ratio on L-T4 monotherapy was 8.45 ± 3.7 while it was 4.70 ± 2.0 (p<0.001) on AT, TSH was 1.30 ± 1.7 mIU/L and T3 1.18 ± 0.51 pmol/L on L-T4 monotherapy while TSH was 1.34 ± 2.4 mIU/L and T3 1.50 ± 0.86 pmol/L on AT (NS for TSH and p<0.003 for T3 ). In both LT4 and AT treatment groups TSH levels were not statistically different compared to those without thyroid disease (NT) while T4/T3 ratio was significantly lower for AT treatment only (Figure 2).

Figure 2 Comparison of T4/T3 ratio and TSH between the three groups is shown. The T4/T3 ratio for AT is significantly lower than for both LT4 and NT groups, <0.0001 (**), while there is no significant difference between LT4 and NT group values. There are no significant differences in TSH levels between groups.
There was no significant change in weight after switching to AT, 75.9 ± 15.46 kilograms on L-T4 and 74.40 ± 15.4 kilograms on AT.
There was no significant correlation between the satisfaction rating and TSH or between satisfaction rating and change in weight after switching to AT nor was there significant difference between TSH levels between any of the 5 groups by satisfaction score. TSH levels on L-T4 monotherapy and AT were not significantly different from NT (1.57 ± 0.73 mIU/L) (Table 2).
Table 2: Thyroid Functions of the Population without Thyroid Disease (NT).
| Variables | Mean | STD |
| Age (Years) | 61.6 | 14.9 |
| Serum TSH (µU/mL) | 1.57 | 0.73 |
| Serum T4 (µg/dL) | 7.7 | 1.39 |
| Serum T3 (pg/dL) | 0.91 | 0.17 |
| T4/T3 ratio | 8.64 | 1.71 |
Abbreviations: TSH= Thyroid Stimulating Hormone, L-T4= Levothyroxine, T4= Thyroxine, T3= Triiodothyronine
There were patients in both treatment groups with TSH levels outside the normal range however; TSH below <0.4, 58 patients on L-T4 monotherapy (Figure 3)
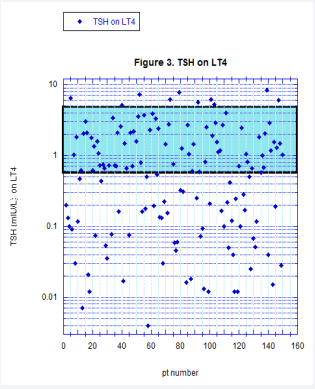
Figure 3 Distribution of TSH values for LT4 treated patients is shown. The shaded portion represents the normal range. A log scale is used to display TSH levels to provide better visual separation of small values.
and 61 patients on AT (Figure 4)
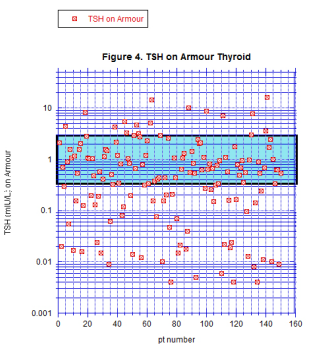
Figure 4 Distribution of TSH levels for AT treated patients is shown. The shaded portion indicates the normal range. A log scale is used to display TSH levels to provide better visual separation of small values.
and TSH above 4.0 mIU/L, 10 patients on L-T4 monotherapy and 12 patients on AT.
DISCUSSION
This retrospective observational study represents the findings of a single out-patient endocrine practice and subjects were not excluded if they had other intercurrent illnesses common in this population such as diabetes, hypertension, and neoplastic disease. These limitations add significantly to the complexity of interpreting our results. The findings however, mirror and expand on those of a prospective, double blind, cross over design study [17] in an unselected group of hypothyroid subjects. In our analysis 78.0 % rated subsequent AT treatment as superior while in the prospective study of unselected hypothyroid patients [17] a 48.6% preference for AT compared to L-T4 monotherapy was reported. Interestingly, in a study [11] comparing LT4 to combination LT4 plus LT3, 52.2% preferred combination therapy. The higher percentage of patients preferring AT in the present study is the expected result of a selection bias for patients already dissatisfied with LT4 treatment.
Recent studies suggest that due to polymorphism of the D2 deiodinase gene a percentage of the general population with hypothyroidism may require higher levels of intracellular T3 then can be provided by L-T4 replacement therapy [12]. These individuals would continue to experience symptomatic hypothyroidism despite peripheral T4, T3 and TSH levels in the normal range. In the report by Paniker et al, 16% of the general population exhibited the susceptible genotype. In the present analysis, the subgroup of 150 out of 450 patients being treated for hypothyroidism could include a concentration of the population with this genotype helping to explain the preference for a T3 containing treatment. Future studies providing information on genetic markers for D2 deiodinase polymorphism in the sub-group of hypothyroid patients with persistent symptoms who responded favorably to AT would be invaluable for clarifying the basis for this preference.
TSH levels were comparable on L-T4 monotherapy and AT therapies. In both treatment regimens TSH levels were not significantly different than the reference group without known thyroid disease. Importantly, a portion of each treatment group had values above or below the normal range. This is the result of on-going treatment adjustments required during the process of finding a medication dosage providing maximal relief of symptoms of hypothyroidism. While avoidance of medication toxicity or under treatment is the ultimate goal, during active management it is not always possible to avoid excursions outside these parameters. As opposed to studies employing a fixed medication dosage the results presented here do not necessarily reflect the final equilibrium point in management. In fact, the persistence of symptoms despite low TSH while titrating LT4 dosage frequently served as a trigger for a trial of AT in this practice. Of 58 patients on L-T4 who had TSH levels below the lower limit of normal, only 11 had persistence of this biochemical abnormality after switching to AT while the rest achieved normalization of this key parameter at the time of sampling.
Previous studies of T4 plus T3 therapy suggest that increased peripheral thyroid hormone concentrations reflected by suppressed TSH levels [11] could be a factor in the favorable response to this therapy. In the present analysis however, there was no correlation of satisfaction ratings with TSH levels, in agreement with others [11,17].
There was no change in weight after switching from L-T4 monotherapy to AT. These results suggest that clinical improvements seen with AT were not due to weight loss as has been suggested in other studies of combination therapy [11,17,19]
Previous studies have shown a significant placebo affect persisting for up to 12 months, associated with use of combination L-T4 and T3 treatment [10]. Although some patients reported great improvement in well being occurring within a few days to weeks of being switched to AT from L-T4, characteristic of a placebo effect, there was no correlation of duration of treatment with satisfaction rating in the AT group. Perception of the superiority of AT persisted so that patients still reported their preference for AT even after years of use. These finding are against the existence of a simple placebo effect as the basis of the results here.
Finally, warnings regarding use of AT in older adults have been issued [1,21] although there is no published data to substantiate these concerns. In our study 30 individuals over age 65 years were successfully treated with AT without untoward events with a mean treatment duration of 2.87 ± 2.19 yrs in this older population, minimum 0.5 to a maximum of 10 yrs on AT.
CONCLUSION
AT treatment produced high satisfaction scores in a group of hypothyroid patients with persistent symptoms on L-T4 therapy. Our findings suggest that AT preference is not due to placebo effect, induction of hyperthyroidism or weight loss. No significant untoward effects of this therapy were noted inclusive of 30 subjects 65 yrs of age and older. As suggested by Hershman [20], AT seems no more dangerous than adding T3 to L-T4 therapy and can be offered to patients who “don’t feel normal” on L-T4 monotherapy. Larger prospective studies would help clarify what role AT plays in replacement therapy of patients dissatisfied with L-T4 monotherapy for hypothyroidism. Our results are encouraging to clinicians that this drug does provide a viable treatment alternative.
DISCLOSURE
Dr. Casanova-Romero is on the speakers’ bureau of Sanofi. Dr. Pepper has no multiplicity of interest to disclose. This research was conducted without funding from any public, commercial, or not-for-profit agencies. This research was presented in part at the 83rd Annual Meeting of the American Thyroid Association; Abstract #25, October 17, 2013.









































































































































