Mediterranean Dietary Pattern Adherence and Plasma Lipids Profile
- 1. Department of Cardiovascular, Respiratory, Nephrologic, Anesthesiologic and GeriatricSciences, “Sapienza” University of Rome, Italy
- 2. Department of Cardiovascular, Respiratory, Nephrologic and Geriatric Sciences, Sapienza University of Rome, Geriatric Center Romano, Italy
Abstract
We sought to explore whether the adherence to the Mediterranean dietary pattern is associated with better plasma lipid profile, regardless of obesity, insulin resistance and metabolic syndrome.
Adult outpatients free of clinical cardiovascular diseases, diabetes, previously diagnosed Dyslipidemia and any lipid-lowering medications, were considered. The following features were assessed: HDL and total cholesterol, triglycerides and total to HDL cholesterol ratio. Insulin resistance was assessed through HOMA index. The adherence to Mediterranean dietary (Med Diet) pattern was assessed through a validated 14-item questionnaire.
Twenty-two out of fifty subjects adhered to Med Diet. Subjects with low adherence had higher prevalence of metabolic syndrome and poorer plasma lipids profile and insulin resistance state. The bivariate regression analysis showed an inverse trend between Med Diet score and total to HDL cholesterol ratio (r= -0.417; p= 0.003) and triglycerides (r= -0.355; p= 0.01), and a positive trend with HDLc (r= 0.279; p=0.04). When multivariable regression models were constructed, the higher Med Diet score predicted higher HDLc (β= 0.340; SE (β)= 0.109; p= 0.016) and lower total to HDLc ratio (β= -0.437; SE(β)= 0.011; p= 0.007) and triglycerides (β= -0.893; SE(β)= 0.438; p= 0.043). Interestingly, whole and abdominal obesity, insulin resistance and presence of metabolic syndrome did not affect the associations.
Med Diet may be associated to favorable plasma lipids profile, independently of being overweight / obese and having insulin resistance and metabolic syndrome. Further investigations will assess whether the adoption of Med Diet may prevent metabolic disorders and reduce the rate of progression towards clinical cardiovascular diseases.
Keywords
• Mediterranean diet
• Lipids profile
• Metabolic syndrome
Citation
Viscogliosi G, Ettorre E, Chiriac IM, Andreozzi P, Cacciafesta M (2014) Mediterranean Dietary Pattern Adherence and Plasma Lipids Profile. J Endocrinol Diabetes Obes 2(2): 1022.
INTRODUCTION
Parallel with the alarming increase of obesity and sedentary lifestyles, Western countries are facing a pandemic of metabolic disorders [1,2]. Plasma lipids alterations are a widespread condition in adults, even in the absence of genetic predisposition, representing major cardiovascular (CV) risk factors [2].
In most cases, lipids derangements with onset in adulthood frequently overlap with other CV and metabolic traits [2]. Metabolic syndrome (MetS), a cluster of CV and metabolic risk factors, is frequently characterized by insulin resistance, which may be independently associated with lipid derangements. In its classical definition, diagnostic features of MetS include low high-density lipoprotein cholesterol (HDLc) and high plasma triglycerides. In spite of this, elevation of non-HDL cholesterol is frequent in MetS, resulting in higher total plasma cholesterol concentrations.
Adhering to healthy dietary pattern and performing physical exercise, are known to have a beneficial impact on lipid metabolism [1,3-6]. The Mediterranean diet (Med Diet) is an example of healthy dietary pattern [1,7], with a growing body of evidence reporting its beneficial effects on CV and metabolic risk factors, as well as in preventing CV diseases and diabetes [1-8].
It remains unclear whether poorer dietary habits lead to lipid homeostasis derangements, regardless of overweight/obesity and insulin resistance.
The present study was aimed to explore whether the adherence to Med Diet pattern predicts better lipids profile, independently of the presence of MetS, insulin resistance and obesity.
MATERIALS AND METHODS
Subjects who visited the Ambulatory of our Department, for a specialist evaluation of cardiovascular risk factors, in the period between January and November 2013, were considered for the present investigation. Exclusion criteria included any history of: previously diagnosed dyslipidemia or conditions of familial dyslipidemia, relevant changes in diet within the past year, history of clinical cardiovascular diseases, diabetes mellitus, consumption of more than 200 ml of alcoholic beverages for women, and more than 300 ml for men. We further excluded subjects on treatment with any lipid-lowering agents, including dietary supplements, and those on treatment with anti-diabetes drugs. Antihypertensive medications were allowed, except for α and β-blockers and diuretics.
In the same day of the visit, all elements of the study assessment were obtained for each patient.
A face to face interview investigated medical history and general habits of participants.
Venous blood samples were drawn in the early morning, after an overnight fast of at least 8 hours. Blood was analyzed for fasting blood glucose, triglycerides, HDL and total cholesterol, using standard enzymatic methods. Fasting insulin was assessed with an enzyme-linked immunosorbant assay kit.
Insulin resistance was assessed by homeostasis model assessment (HOMA) of insulin resistance, with the following formula: HOMA = [(fasting insulin U/ml) x (fasting glucose mmol/L)] / 22.5.
Blood pressure was measured in sitting position, after subjects had rested for 10 minutes, using a mercury sphygmomanometer. The mean of three measures was considered. Hypertension was defined for systolic blood pressure values > 130 mmHg and/or diastolic > 85 mmHg or being on stable treatment.
Weight was assessed with subjects in light clothes, and approximated at the nearest 0.1 kg; height was measured without shoes, and approximated at the nearest 0.1 m. Body mass index was calculated by dividing the weight for the square of height (Kg/m² ). Waist circumference was measured with subjects standing, at the level of the iliac crests, at the end of a normal expiration.
Metabolic syndrome was defined with the third report of the National Cholesterol Education Program (NCEP ATP III, 2001) criteria, by the presence of three or more of the following features: hypertension; HDL cholesterol < 40 mg/dl in men and < 50 mg/dl in women; plasma glucose > 110 mg/dl; abdominal obesity defined as waist circumference > 102 cm in men and > 88 cm in women; plasma triglycerides > 150 mg/dl [2].
The adherence to Med Diet was assessed through a previously validated 14-item questionnaire [1], which was administered by a physician. The total score ranges from 0 to 14, the higher the score the higher the adherence to Med Diet. Each item is scored 0 or 1. 1 point is given for: 1) using olive oil as main culinary fat; 2) daily consumption of at least 4 tablespoons of olive oil; 3) daily consumption of at least 2 servings of vegetables; 4) daily consumption of at least 3 fruits; 5) daily consumption of less than 100 grams of red/processed meat; 6) daily consumption of less than 12 grams of animal fat products such as butter or cream; 7) daily consumption of less than 100 ml of sugar-sweetened beverages; 8) moderate consumption of red wine; 9) weekly consumption of at least 3 servings (1 serving = 150 grams) of pulses; 10) weekly consumption of at least 3 servings (1 serving= 150 grams) of fish; 11) weekly consumption of less than 2 commercial pastries; 12) weekly consumption of at least 3 servings (1 serving= 30 grams) of tree nuts; 13) preferring white over red meats; 14) weekly consumption, at least in 2 occasions, of soffritto, a sauce made with tomato, garlic, onion or leeks, sauted in olive oil. Adherence to Med Diet was defined for total scores > 7/14.
Physical activity performance was self-reported. Housework was regarded as “low-intensity” physical exercise; steady-pace walking was considered as “moderate-intensity” physical exercise; run or gym activities as “high-intensity” physical exercise. Physical activity score was calculated as: (hours of low-intensity exercise/week x 1) + (hours of moderate-intensity exercise/week x 2) + (hours of high-intensity exercise x 3).
RESULTS AND DISCUSSION
Fifty subjects were enrolled. The mean age of the study population was 57.3± 10.1 years, 62% were women. The overall adherence to the Mediterranean dietary pattern was low, with a mean Med Diet score of 7.4±3.1.
Table 1: Characteristics of the sample according to the Med Diet adherence.
| Med Diet adherence | |||
| Low (n=28) | High (n=22) | p | |
| Females (%) | 64.3 | 59.0 | ns |
| Age (years) | 56.0±10.3 | 59.1±10.2 | ns |
| Current smoking (%) | 21.4 | 13.6 | ns |
| Current workers (%) | 53.6 | 45.5 | ns |
| Physical activity (score) | 27.0±4.2 | 36.1±7.6 | <0.001BMI |
| (kg/m²) | 32.0±5.2 | 27.1±3.2 | <0.001 |
| Metabolic syndrome (%) | 68.0 | 13.6 | <0.001 |
| Abnormal WC (%) | 78.6 | 36.4 | 0.006 |
| Low HDLc (%) | 46.4 | 28.0 | ns |
| High Tryglicerides (%) | 53.6 | 23.0 | 0.042 |
| Impaired FBG (%) | 53.6 | 4.5 | <0.001 |
| Hypertension (%) | 75.0 | 45.5 | ns |
| HOMA (n) | 4.18±2.4 | 1.50±0.7 | <0.00 |
| Plasma lipids | |||
| Total cholesterol (mg/dl) | 227.1±38.2 | 203.8±34.0 | 0.029 |
| HDLc (mg/dl) | 50.2±14.4 | 58.6±14.0 | 0.044 |
| Total to HDLc ratio (n) | 5.04±1.8 | 3.70±0.9 | 0.003 |
| Triglycerides (mg/dl) | 155.3±66.0 | 116.6±60.6 | 0.038 |
Abbreviations: Med Diet: Mediterranean Diet; BMI: Body Mass Index; WC: Waist Circumference; FBG: Fasting Blood Glucose.
As shown by Table 1, subjects with low adherence (n=28), as expected, were characterized by poorer metabolic status and they were more likely to have sedentary lifestyle. In particular, measures of whole and abdominal obesity were significantly higher, as well as the prevalence of MetS, impaired FBG and insulin resistance. With particular regard to plasma lipids, low-adherence subjects were more likely to have higher concentrations of total cholesterol, triglycerides and total to HDL cholesterol ratio. Mean HDLc was slightly higher in high-adherence subjects.
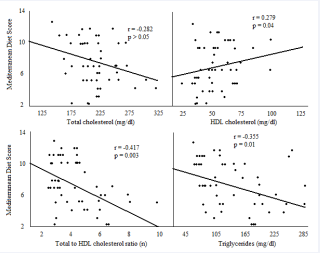
Figure 1: Bivariate regression analysis. Correlations between Mediterranean diet adherence with plasma lipids concentrations.
Figure 1 shows the results of the bivariate regression analysis between Med Diet scores and plasma lipid profile. Higher Med Diet scores showed an inverse trend with total cholesterol, triglycerides and total to HDLc ratio, as well as a positive association with HDLc concentrations. All associations were statistically significant, except for total cholesterol.
Table 2: Multivariable regression analysis Predictors of plasma lipids.
| Total cholesterol | HDL cholesterol | |||
| β (SEβ) | p | β (SEβ) | p | |
| Med Diet score | -1.076 (0.804) | ns | 0.340 (0.109) | 0.016 |
| BMI | 0.126 (0.096) | ns | -0.858 (0.225) | ns |
| WC | 0.138 (0.199) | ns | 0.290 (0.246) | ns |
| HOMA | 0.088 (0.027) | ns | -1.196 (0.540) | 0.013 |
| Total to HDL ratio | Triglycerides | |||
| β (SEβ) | p | β (SEβ) | p | |
| Med Diet score | -0.437 (0.011) | 0.007 | -0.893 (0.438) | 0.043 |
| BMI | 0.163 (0.009) | ns | 0.385 (0.003) | 0.006 |
| WC | 0.301 (0.098) | ns | 0.473 (0.012) | 0.006 |
| HOMA | 1.216 (0.560) | 0.015 | 0.222 (0.482) | ns |
Abbreviations: Med Diet: Mediterranean diet; BMI: body mass index; WC: waist circumference; HOMA: homeostasis model assessment.
When multivariable regression models were constructed as shown by Table 2, Med Diet scores were found to predict higher HDLc, as well as an inverse association with total cholesterol, total to HDLc ratio and triglycerides. Interestingly, none of the specific Med Diet items were associated with plasma lipids. Higher BMI and WC values were associated with triglycerides; insulin resistance predicted lower HDLc concentrations and higher total to HDLc ratio. Such association was independent of FBG, which was entered in the multivariable regression model and was not found to be associated with any plasma lipid parameter. All in all, we have found that higher adherence to Med Diet pattern was cross-sectionally associated with more favorable plasma lipids profile, in a population of patients free of diabetes, previously diagnosed hyperlipidemia and familial history of altered lipids homeostasis. Moreover the association was independent of body weight, abdominal obesity, insulin resistance and presence of MetS, suggesting that the Med Diet pattern may be directly impact on lipid pathways, independently of weight gain and associated metabolic-disorders. It is noteworthy that none of the specific Med Diet items was associated with any of the plasma lipid features. This interesting finding, in line with previous reports [1], suggests that the overall dietary pattern, more than specific food categories, may beneficially impact on cholesterol and triglycerides homeostasis. The concept of Med Diet arose from observations of dietary habits of people living in the Mediterranean basin [1,4-8]. Such dietary pattern is mainly based on the consumption of non-refined products, especially vegetables, fruits, unrefined grain products, moderate consumption of wine. On the other side, red meat and processed meat products, as well as fast food, are far from the typical Med Diet. Given that several pieces of evidence have provided support for the beneficial impact of Med Diet on cardiovascular and metabolic disorders, clinicians should keep in mind that the adoption of a healthy diet should always be fostered.
CONCLUSION
Future investigations are needed to assess whether the adoption of Med Diet pattern can impact on the incidence of cardiovascular diseases, by slowing or delaying their onset, at a population level. Moreover, we need to know whether specific components of Med Diet may exert nutrigenomic effects by modulating metabolic pathways at a genetic and/or epigenetic level, which may explain inter-individual differences in the dietary modulation of metabolic homeostasis. A better understanding of such gene/diet interaction would be especially useful in the patients with genetic lipid derangements, and particularly for those in whom dyslipidemia manifests solely with the reduction in HDL cholesterol, for whom effective therapeutic strategies have not been provided yet.