Water-Clear Cell Adenoma of Parathyroid Gland: A Case Report and Concerns on Differential Diagnosis
- 1. Department of Pathology, “Evangelismos”General Hospital, Athens,Greece
- 2. Department of Pathology,“SaintSavvas”Anticancer Oncologic Hospital, Athens, Greece
- 3. Department of Pathology, “Metaxa” Cancer Hospital, Piraeus, Greece
Abstract
Primary Water-Clear Cell Adenoma (WCCA) of the parathyroid glands are extremely rare neoplasm, consisting of cells with clear, foamy cytoplasm filled with glycogen, lacking an infiltrative growth pattern and metastases. We report the case of a 58-year-old woman with primary hyperparathyroidism, without a known history of MEN-1 or NF-1, with a tumour posterior to the right thyroid lobe. No evidence of metastasis was reported. The clinical diagnosis was parathyroid adenoma. Following the surgical procedure, we received an encapsulated tumor measuring 4,5 cm in diameter and weighting 12 gr, consisting of water-clear cell cells, without mitoses, atypical features or capsular invasion, at the rim of which normal residual parathyroid tissue was included. The differential diagnosis included a variety of primary and secondary clear-cell tumors of head and neck region, however the morphological and immunohistochemical (strong positivity only for PTH, p27 and bcl-2) assessment drove to the diagnosis of WCCA of the parathyroid gland. After the operation, the levels of PTH in patient’s serum dropped to normal and the post-operative course remained free of symptoms or abnormal laboratory findings. In conclusion, all the clinical and laboratory findings strongly suggested the diagnosis of WCCA of the parathyroid gland, however because of the rarity of this type of tumours, we had to examine this partiular tumour in detail, in order to exclude all the other clear-cell tumours that can appear in this region.
Keywords
- Water-Clear Cell Adenoma
- Parathyroid glands
- Parathormone
Citation
Ioannis P, Stavros P, Nektarios K, Chrysa S, Kalliopi P, et al. (2018) Water-Clear Cell Adenoma of Parathyroid Gland: A Case Report and Concerns on Differential Diagnosis. J Endocrinol Diabetes Obes 6(1): 1117.
ABBREVIATIONS
MEN-1: Multiple endocrine neoplasia type 1; NF-1: Neurofibromatosis type I; PTH: Parathormone; U/S: Ultrasound; WCCA: Water-Clear Cell Adenoma
INTRODUCTION
Primary hyperparathyroidism is most commonly attributed to parathyroid tumors such as parathyroid hyperplasia. parathyroid adenoma or more rarely to parathyroid carcinoma [1]. Parathyroid adenomas, are benign, most often single tumors, consisting of either chief cells or oxyphil cells or both types of cells, sometimes admixed focally with a few cells with clear-cell morphology. Parathyroid carcinomas may show a morphology similar to adenoma, with additional invasive and metastatic features. However, parathyroid tumours consisting exclusively of clear cells is a quite rare entity. To our knowledge, so far there have been twenty-one cases reported worldwide [1-19,22]. Herein, we present a case of a large water-clear cell adenoma (WCCA) with special considerations on its particular immunophenotype and differential diagnosis.
CASE PRESENTATION
A 58 year old female patient presented to the 3rd Surgical Department of our Hospital for evaluation of hyperthyroidism, with no recorded history of either Multiple neuroendocrine neoplasia-1 (MEN-1) or type 1 Neurofibromatosis (NF-1).
The biochemical and serological analysis showed a total serum calcium level of 10.4mg/dL (reference range 8.5-10.5mg/ dL), serum phosphorus level of 1.4mg/dL (reference range 2.5- 5mg/dL) and PTH level of 902 pg/mL (reference range 10-67pg/ dL), indicating hyperparathyroidism.
On preoperative ultrasound (U/S), an avascular formation with an echogenicity similar to that of fat was detected at the right paratracheal region, right behind the right thyroid lobe. Its lower edge was difficult to be localized, probably being situated in the mediastinum. No other change or lesion was observed. The patient was admitted for surgical operation with the diagnosis of parathyroid adenoma. During the procedure, we received a part of the above mentioned formation for intraoperative pathological consultation (frozen section biopsy) 1,1 cm in diameter, which revealed a lesion consisting of clear cells, at the periphery of which scant normal parathyroid tissue.
The surgical specimen for routine histological analysis weighted 12 gr, measuring 4.5 cm in its greatest diameter. Upon macroscopic inspection, it was partially surrounded by a thin fibrous capsule. Its cut surface was yellow to tan, with a partially firm or elastic texture.
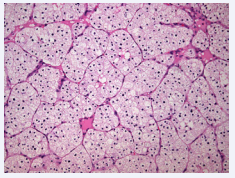
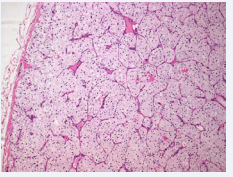
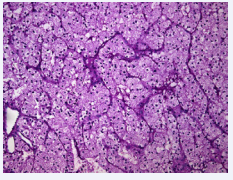
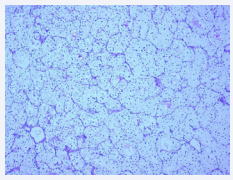
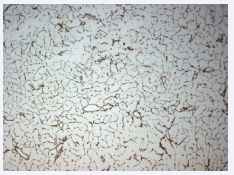
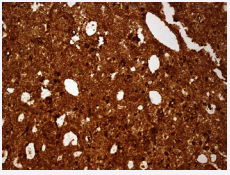
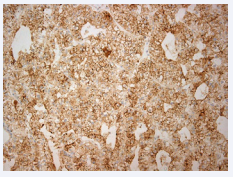
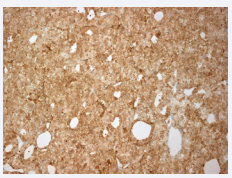
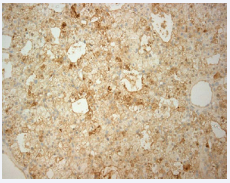
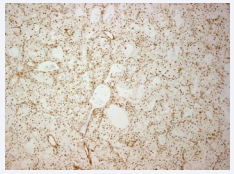
On microscopic examination, the tissue composed almost exclusively of water-clear cells growing in a solid pattern (Figure 1 and 2) or in nests, delineated by a thin vascular network (Figure 5). The morphology of the cells resembled the one described in other clear cell adenomas: foamy clear cytoplasm with PAS and PAS-diastase positive granules (Figures 3, 4), hyperchromatic, small, centrally located nuclei, no cellular or nuclear atypia (Figures 1,2).
Figure 1: Histology shows an encapsulated lesion composed of clear cells, which in turn are arranged into nests or solid sheets. No capsular invasion is noted (H/E x100).
Figure 2: On high power, cells appear to have a foamy cytoplasm, centrally located basophilic nuclei and no mitotic activity (H/E x200).
Furthermore, no necrosis, hemorrhage, mitosis (Figures 1,2 and 7), capsular invasion (Figure 2) or lymphovascular invasion were detected, ruling out the possibility for a water-cell parathyroid carcinoma. A peripheral rim of compressed parathyroid tissue was recognized, with no further histopathological changes.
Figure 3: Cell cytoplasm appears to contain PAS (left) and PASdiastase positive (right) granules (x200, x100.
Figure 4: Cell cytoplasm appears to contain PAS (left) and PASdiastase positive (right) granules (x200, x100.
Figure 5: CD34 staining reveals a thin vascular network delineating the nests of neoplastic cells (x100).
Figure 6: PAX-2 shows diffuse distribution with no actual nuclear staining (x200).
Figure 7: Diffuse, strongly positive cytoplasmic staining with PTH (x200).
Figure 8: No mitotic activity on PHH-3 (x100).
Figure 9: Bcl-2 weakly to strongly positive for the majority of neoplastic cells (x200).
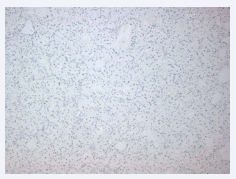
Figure 10: No nuclear staining for PGP 9.5 (x100).
Figure 11: Positive nuclear staining for p27 for the majority of tumour cells (x100).
Figure 12: No staining for Melan-A (x100).
The immunohistochemical analysis showed positive, diffuse staining for PTH (Figure 7) and RCC, positive staining for p27 (Figure 11) and bcl-2 (Figure 9) for the majority of waterclear cells and negative staining for PGP9.5, Thyroglobulin, PAX-2 (Figure 6), Galectin-3, TTF-1, CD56, Chromogranin, Synaptophysin, Calcitonin, PAX-8, CA-IX, GCDFP-15, Calponin, p63, S-100, Melan-A (Figure 12) and HBM-45 and a very low cell proliferation rate Ki-67 (less than 1%).
The morphological features combined with the diffuse, strong positivity for PTH, p27, bcl-2 and the negativity for PGP 9.5 led to the diagnosis of WCCA of the parathyroid gland.
The patient’s postoperative clinical course was uneventful. There was no evidence of increased calcium or PTH levels in blood post-operatively. On follow-up appointments, all laboratory measurements, including calcium and PTH, remained within the normal range.
DISCUSSION
Parathyroid glands in adults consist mainly of chief and oxyphilic cells [5]. The presence of water-clear cells is not included in the normal histological picture of the parathyroid glands and their origin remain until today controversial. There were studies suggesting that water-clear cells are originating from chief cells, others that all three types of parathyroid parenchymal cells (chief cells, oxyphilic cells and water clear cells) are coming from a single type of cells, suggesting hyper functioning of the parathyroid glands [6,14].
Parathyroid adenomas are single masses, usually weighting from 1.0 to 5.0, reaching a maximum diameter of about 6,5 cm. They are mainly composed of chief or oxyphilic or of both the cell types, lacking features suggesting invasive growth pattern or metastases [3]. Parathyroid adenomas consisting exclusively of water-clear cells are rare and they were firstly reported in 1994 by Kovacs et al. [4]. Interestingly, an earlier reported case of clear-cell hyperplasia mimicking parathyroid adenoma was later considered as a probable case of WCCA. To this day, a total of twenty cases of water-clear ell parathyroid adenomas have been reported in literature.
Given the rarity of these lesions, the size of our specimen, its deep localization as well as the nested pattern of growth, in our case, a wide differential diagnosis had to be considered regarding clear cell lesions of the neck area [20,21]. Clear-cell type change thyroid carcinoma (e.g. papillary carcinoma) was ruled out because of Thyroglobulin and TTF-1 negativity and Calcitonin, CD56, Chromogranin and Synaptophysin negativity eliminated the possibility of Paraganglioma and Paragangliomalike medullary thyroid carcinoma [20]. Clear-cell tumours of the salivary glands (clear cell acinic cell carcinoma, clear cell myoepithelial carcinoma, epithelial myoepithelial carcinoma, hyalinizing clear cell carcinoma) were ruled out because of p63 and Calponin negativity [20]. Metastatic clear cell Renal Cell Carcinoma was excluded because of CA-IX, PAX-2 and PAX-8 negativity [20]. Also negativity for Mammoglobin and GCDFP-15 excluded metastatic breast carcinoma [21] and negativity for S-100, Melan-A and HBM-45 excluded metastatic balloon cell melanoma or soft part clear cell sarcoma [20]. In addition to differential diagnosis considerations, indicators of endocrine activity have been of interest among researchers regarding WCCA. Kanda et al. [10], initially postulated that WCCA have a low endocrine activity, based on correlation between adenoma size and clinical/biochemical presentations. Pirela et al. [22], found a positive correlation between PTH levels at presentation and adenoma size upon pathological macroscopic examination. Our case seems to be in accordance with these findings.
In conclusion, we describe a case of water-clear cell tumor of the parathyroid gland, consisting exclusively of water-clear cells, surrounded by a thin capsule with normal residual parathyroid tissue at the periphery of the lesion, without invasive growth pattern or metastasis. The immunohistochemical assessment of the tumor cells revealed positivity for PTH, p27 and bcl-2, with all the other stains being negative, ruling out other primary or secondary clear-cell tumors of head and neck region. The patient’s PTH dropped to normal levels after the resection of the tumor. All these clinical and histological features supported strongly the diagnosis of water-clear cell adenoma of the parathyroid gland.
ACKNOWLEDGEMENTS
The authors would like to thank Mr. Koufou Nikolaos for the English language review of the text.