Comparative Study of the Burden Associated with the Management of Open Tibia Shaft Fractures using Illizarov Frame Fixator and Linear Rail System in a Resource Poor Country
- 1. Department of Orthopaedics and Trauma Surgery, University College Hospital, Nigeria.
- 2. Department of Surgery, University of Ibadan, Nigeria.
- 3. Department of Surgery, University of Ibadan, Nigeria.
Abstract
Background: Management of open tibia shaft fractures is frequently laden with complications. Hence this places an enormous burden on the patient and the surgeon alike. The study objective is to determine the union and non-union rate, and associated complications encountered in the management of open tibia shaft fractures using the Ilizarov frame fixator and Linear rail system [LRS] in Ibadan, Nigeria.
Research Method: This is a follow up study to our previous prospective study involving thirty (30) patients of both sexes, divided into two (2) groups; Ilizarov frame fixator group and LRS group. All patients had open tibia shaft fractures of Gustillo-Anderson Class [GA II-IIIB]. The union rate, non-union rate, associated complications noted while on the respective devices as well as the mean total cost implication of managing these open tibia fractures using the Ilizarov frame fixator and LRS respectively were all assessed.
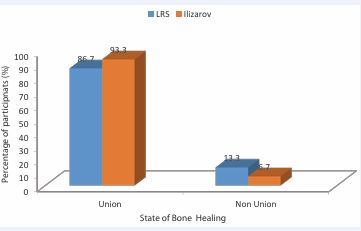
Result: The union rate in the LRS group was 86.7% while the non-union rate was 13.3%. In the Ilizarov group, the union rate was 93.3% while the non-union rate was 6.7%. The mean total cost implication for the management of open tibia shaft fractures using LRS and Ilizarov frame fixators were N455,960.0±46,967.3 and N505,614.3±113,345.9 respectively. There is no significant difference noted in the union rate, non-union rate.
Conclusion: This study has shown that management of open tibial shaft fractures using either Ilizarov frame fixator or Linear rail system [LRS] is very cost effective especially in a resource poor country like Nigeria.
INTRODUCTION
Open tibial fractures usually occur following high velocity trauma; road traffic accidents (RTA), gunshot injuries and from falls from height [1]. Urbanization and social development have further increased the incidence of this high velocity trauma in our environment.
The recklessness of motorists, inconsistences in the enforcement of traffic laws, unqualified drivers as well as the use of unroadworthy vehicles, and the use of motorcycles as a commercial means of transportation,
largely explain why RTA is a major player in the incidence of open tibia shaft fractures [2-5]. Studies have shown that motorcycle associated RTAs constitute a substantial percentage of these injuries [2,3].
This could be partly because of their perceived affordability, rapidity and ease of accessibility as a means of transport and poor regulation of their use along many highways [2,3]. More so, most of the cyclists, commercial or otherwise, are untrained or poorly trained at best, with some not even licensed to ride a motorcycle.
The management of open fractures is usually tasking and demanding even in the best of hands and with the best of facilities. It is usually a great burden to the patient and the surgeon alike.
The patient is faced with a heavy financial burden, due to the cost of management, emotional burden, if complications ensue and productivity burden, since the patient is usually off work for a long time hence a waste of workforce time and a considerable loss of income.
The surgeon may encounter emotional burden when complications occur and the patient keeps coming back for their problems to be resolved, often insisting on holding the surgeon responsible even when such complications are not due to the actions, or otherwise, of the surgeon.
The conventional protocol for the management of open fractures usually involves debridement, temporary stabilization by external fixators, wound management, and definitive fracture care [6].
This conventional protocol predisposes the affected patients to multiple surgeries, prolonged hospital-stay, exorbitant financial burden and still the complications associated with open fracture management are not outrightly prevented. Thus, with the emergence of complications, the financial burden on the patient increases. Such complications associated with open fracture management include pin tract infection, knee stiffness, wound dehiscence, delayed fracture union, infected non-union and chronic osteomyelitis.
Since we reside in a resource poor country, where patients often pay out of pocket to assess health care, a management protocol was formulated using Illizarov frame fixator and the linear rail system as the definitive fixators of choice.
This protocol was able to strike a balance between reducing the number of surgeries, reducing the financial burden, reducing hospital-stay, and achieving fracture union whilst still reducing the possibility of encountering the previously outlined complications.
This is a comparative prospective follow-up study [7], that compares the burden associated with management of open tibial shaft fractures using the Illizarov frame fixator and linear rail system as the primary definitive fixator of choice in a resource poor country.
This study was carried out to determine and compare the union rate, non-union rate, associated complications encountered and the mean total cost implication in the management of open tibial shaft fractures using the Illizarov frame fixator and linear rail system (LRS).
MATERIALS AND METHODS
This hospital-based prospective study of management of open tibial shaft fractures using the Illizarov frame fixator and LRS as the definitive fixator was conducted in the University College Hospital, Ibadan between July 2021 and June 2023. The study protocol was approved by the Hospital/University Ethics Committee and informed consent was obtained from all patients.
Thirty adult patients with open tibial shaft fractures (Gustillo-Anderson types II, IIIA and IIIB) were included in the study. The inclusion criteria were: open comminuted diaphyseal tibia fractures and open segmental diaphyseal tibia fractures. The exclusion criteria were: pathological fractures of the tibia, open fractures of the tibia with bone loss, open simple fractures of the tibia, bilateral open tibia shaft fractures, spinal cord injured patients, patients with prior neurologic problems like polio before the fracture as well as multiply injured patients.
All patients were resuscitated using the ATLS protocol. Prophylactic antibiotic and tetanus immunization were given; initial wound debridement was done in the emergency room. Prophylactic anticoagulation was commenced in patients at risk of deep vein thrombosis (DVT), as assessed with the standard DVT risk assessment tool used in the hospital.
The patients were divided into two groups by simple randomization techniques and definitive fixation done with either Illizarov frame fixator or LRS. The resultant wounds were also managed at the same surgery either with primary closure by direct suturing, skin grafting or flap cover. Post operatively, all patients had antibiotics, analgesics, and prophylactic anticoagulation. The antibiotic of choice was ceftriaxone/sulbactam and levofloxacin for a period of 7-10 days depending on the extent of soft tissue injury. The choice of antibiotics was based on microbiological prevalence and sensitivity within our environment as is standard for all open fractures presenting to our institution. Analgesics were given until pain subsided. Prophylactic anticoagulation continued till patients could mobilize with bilateral axillary crutches. All patients were taught pin site care. Patients who developed pin tract infection were treated with antibiotics and extensive pin site care until symptoms resolved. Partial weight bearing commenced as pain could be tolerated.
Fracture healing was monitored with periodic radiographs done at important points; immediate post-operative period, sixth, twelfth, eighteenth, and twenty fourth weeks during the follow-up period.
Full weight bearing only commenced when there was evidence of bone union. Bone union was assessed both clinically and radiologically; no pain or movement at fracture site and presence of bridging callus in at least three cortices on the radiographs respectively.
The radiological union time was calculated as the time between surgery and confirmation of radiological union. Thereafter the fixator was then removed and the patient placed in a Sarmiento cast for a period of 4-6 weeks. After removal of the cast, all patients were then assessed using the ASAMI criteria [8], to score the bony and functional outcomes.
Data was collected with a well-structured proforma and thereafter analyzed by an independent statistician using SPSS version 23.0. Descriptive statistics such as frequency, percentages and mean were used to summarize and present the results. Graphs and tables were used where necessary. An independent t-test was used to compare the mean total cost implication in both Illizarov frame fixator and LRS groups. For the comparison of associated complications, a chi-square test was used to compare the difference in both Illizarov frame fixator and LRS groups.
RESULTS
This study had a total of thirty (30) adult participants. Their mean age was 38.7±15.2 years. A total of nineteen (19) males and eleven (11) females participated in the study. Nine (9) males and six (6) females were in the LRS group while ten (10) males and five (5) females were in the Illizarov group (Table 1).
Table 1: Demographic distribution of the participants.
|
Variable |
Items |
LRS N (%) |
Illizarov N (%) |
Total |
t-test /χ2 |
p-value |
|
Age range (years) |
18-34 |
9(60.0) |
4(26.7) |
13(43.3) |
5.234 |
0.155 |
|
35-44 |
2(13.3) |
7(46.7) |
9(30.0) |
|||
|
45-64 |
3(20.0) |
2(13.3) |
5(16.7) |
|||
|
65 and above |
1(6.7) |
2(13.3) |
3(10.0) |
|
|
|
|
Age(years) |
mean?SD [range] |
35.6±16.6 [18-75] |
41.7±13.6 [21-66] |
38.7±15.2 [18-75] |
1.228 |
0.277 |
|
Sex |
Male |
9(60.0) |
10(66.7) |
19(63.3) |
0.144 |
0.705 |
|
Female |
6(40.0) |
5(33.3) |
11(36.7) |
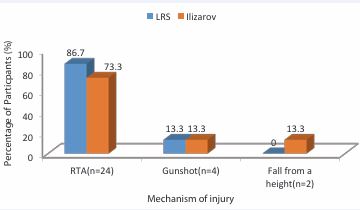
Road traffic accidents (RTA) were noted as the most common mechanism of injury. In the LRS group thirteen (13) of the participants were involved in RTA while two (2) sustained gunshot injuries. In the Illizarov group, eleven (11) of the participants were involved in RTA, two (2) sustained gunshot injuries while two (2) fell from height.
Thus, RTA accounted for 86.7% of the mechanism of injury in the LRS group while in the Illizarov frame group it was about 73.3% (Figure 1).
Figure 1 Bar chart showing the distribution of injury mechanisms.
In the LRS group the union rate was 86.7% while the non-union rate was 13.3 % whereas in the Illizarov frame group, the union rate was 93.3% while the non-union rate was 6.7% (Figure 2).
Figure 2 Bar chart showing Distribution of bone union and non-union in the two fixator groups.
In this study, pin tract infection was noted as the most common complication noticed during the treatment in the external fixators; 80% in the LRS group and 100% in the Illizarov frame group. These pin tract infections mostly involved 2-3 pin tracts, usually grade 1 and 2 (Paley grading). The affected pin tracts were taken care of by regular cleaning with methylated spirit and administration of sensitive antibiotics till the infection subsided.
The second most common complication was knee stiffness; 13.3% in the LRS group and 20% in the Illizarov frame group (Table 2).
Table 2: Distribution of Complications Noticed While on Treatment with Their Various P-Values.
|
Variables of Complications |
LRS N (%) |
Illizarov N (%) |
χ2 |
P-Value |
|
Pin tract infection |
12(80.0) |
15(100.0) |
3.33 |
0.068 |
|
Losing of pins |
0 |
1(6.7) |
1.034 |
0.309 |
|
Non-union |
1(6.7) |
0 |
1.034 |
0.309 |
|
Knee stiffness |
2(13.3) |
3(20.0) |
.240 |
0.624 |
|
Ankle stiffness |
0 |
2(13.4) |
2.143 |
0.143 |
|
Chronic osteomyelitis |
1(6.7) |
1(6.7) |
0.000 |
1.000 |
|
Equinus deformity of the foot |
0 |
1(6.7) |
1.034 |
0.309 |
None of the participants had pin breakage. One (6.7%) participant in the LRS group had non-union following desiccation of the exposed tibia, following flap necrosis.One (6.7%) participant in each of the fixator groups developed chronic osteomyelitis and thereafter resulted in infected non-union.
The differences in the distribution of the complications noticed during the treatment in the two fixator groups were not statistically significant.
The mean cost price for the purchase of the external fixators was shown to be N175,933.3±12,775.0 for the LRS fixator while N216,000.00±42,895.0 for the Illizarov fixator. This difference in the mean cost price of the external fixators was noted to be statistically significant [X2 (15) – 3.467, P=0.002).
However, the mean total cost implication for the management of the participants with open tibia shaft fractures using LRS and Illizarov frame fixators were N455,960.0±46,967.3 and N505,614.3±113,345.9 respectively. This difference in the mean total cost implication between the two fixator groups was noted not to be statistically significant [X2 (15) – 1.567, P=0.128) (Table 3).
Table 3: Comparison of the Mean Total Cost Implication for Management of Open Tibia Shaft Fractures using LRS and Illizarov Frame Fixators.
|
Variables of management |
LRS Mean ± SD (Naira) |
Illizarov Mean ± SD (Naira) |
t-test |
P-Value |
|
Cost of fixator |
175,933.3±12,775.0 |
216,000.0±42,895.0 |
3.467 |
0.002 |
|
Surgery fee |
169,826.7±27,267.2 |
164,320.0±8,519.1 |
0.747 |
0.462 |
|
Total cost of X-ray |
30,000.0±0 |
29,933.3±7,272.0 |
0.035 |
0.972 |
|
Cost of Scotch cast material |
5,900.0±0 |
5,506.7±1,523.3 |
1.000 |
0.326 |
|
Cost of cast application |
4,200.0±0 |
3,920.0±1084.4 |
1.000 |
0.326 |
|
Total cost of feeding |
28,673.3±16,400.6 |
44,200.0±68,280.9 |
0.856 |
0.399 |
|
Total amount spent on admission fees |
33,426.7±20288.0 |
34,266.7±15198.1 |
0.128 |
0.899 |
|
Follow-up consultation fee |
8,000.0±0 |
7,466.7±2065.6 |
1.000 |
0.326 |
|
Total cost |
455,960.0±46,967.3 |
505,613.3±113,345.9 |
1.567 |
0.128 |
RESULTS
This study had a total of thirty (30) adult participants. Their mean age was 38.7±15.2 years. A total of nineteen (19) males and eleven (11) females participated in the study. Nine (9) males and six (6) females were in the LRS group while ten (10) males and five (5) females were in the Illizarov group (Table 1).
Table 1: Demographic distribution of the participants.
|
Variable |
Items |
LRS N (%) |
Illizarov N (%) |
Total |
t-test /χ2 |
p-value |
|
Age range (years) |
18-34 |
9(60.0) |
4(26.7) |
13(43.3) |
5.234 |
0.155 |
|
35-44 |
2(13.3) |
7(46.7) |
9(30.0) |
|||
|
45-64 |
3(20.0) |
2(13.3) |
5(16.7) |
|||
|
65 and above |
1(6.7) |
2(13.3) |
3(10.0) |
|
|
|
|
Age(years) |
mean?SD [range] |
35.6±16.6 [18-75] |
41.7±13.6 [21-66] |
38.7±15.2 [18-75] |
1.228 |
0.277 |
|
Sex |
Male |
9(60.0) |
10(66.7) |
19(63.3) |
0.144 |
0.705 |
|
Female |
6(40.0) |
5(33.3) |
11(36.7) |
Road traffic accidents (RTA) were noted as the most common mechanism of injury. In the LRS group thirteen (13) of the participants were involved in RTA while two (2) sustained gunshot injuries. In the Illizarov group, eleven (11) of the participants were involved in RTA, two (2) sustained gunshot injuries while two (2) fell from height.
Thus, RTA accounted for 86.7% of the mechanism of injury in the LRS group while in the Illizarov frame group it was about 73.3% (Figure 1).
Figure 1 Bar chart showing the distribution of injury mechanisms.
In the LRS group the union rate was 86.7% while the non-union rate was 13.3 % whereas in the Illizarov frame group, the union rate was 93.3% while the non-union rate was 6.7% (Figure 2).
Figure 2 Bar chart showing Distribution of bone union and non-union in the two fixator groups.
In this study, pin tract infection was noted as the most common complication noticed during the treatment in the external fixators; 80% in the LRS group and 100% in the Illizarov frame group. These pin tract infections mostly involved 2-3 pin tracts, usually grade 1 and 2 (Paley grading). The affected pin tracts were taken care of by regular cleaning with methylated spirit and administration of sensitive antibiotics till the infection subsided.
The second most common complication was knee stiffness; 13.3% in the LRS group and 20% in the Illizarov frame group (Table 2).
Table 2: Distribution of Complications Noticed While on Treatment with Their Various P-Values.
|
Variables of Complications |
LRS N (%) |
Illizarov N (%) |
χ2 |
P-Value |
|
Pin tract infection |
12(80.0) |
15(100.0) |
3.33 |
0.068 |
|
Losing of pins |
0 |
1(6.7) |
1.034 |
0.309 |
|
Non-union |
1(6.7) |
0 |
1.034 |
0.309 |
|
Knee stiffness |
2(13.3) |
3(20.0) |
.240 |
0.624 |
|
Ankle stiffness |
0 |
2(13.4) |
2.143 |
0.143 |
|
Chronic osteomyelitis |
1(6.7) |
1(6.7) |
0.000 |
1.000 |
|
Equinus deformity of the foot |
0 |
1(6.7) |
1.034 |
0.309 |
None of the participants had pin breakage. One (6.7%) participant in the LRS group had non-union following desiccation of the exposed tibia, following flap necrosis.One (6.7%) participant in each of the fixator groups developed chronic osteomyelitis and thereafter resulted in infected non-union.
The differences in the distribution of the complications noticed during the treatment in the two fixator groups were not statistically significant.
The mean cost price for the purchase of the external fixators was shown to be N175,933.3±12,775.0 for the LRS fixator while N216,000.00±42,895.0 for the Illizarov fixator. This difference in the mean cost price of the external fixators was noted to be statistically significant [X2 (15) – 3.467, P=0.002).
However, the mean total cost implication for the management of the participants with open tibia shaft fractures using LRS and Illizarov frame fixators were N455,960.0±46,967.3 and N505,614.3±113,345.9 respectively. This difference in the mean total cost implication between the two fixator groups was noted not to be statistically significant [X2 (15) – 1.567, P=0.128) (Table 3).
Table 3: Comparison of the Mean Total Cost Implication for Management of Open Tibia Shaft Fractures using LRS and Illizarov Frame Fixators.
|
Variables of management |
LRS Mean ± SD (Naira) |
Illizarov Mean ± SD (Naira) |
t-test |
P-Value |
|
Cost of fixator |
175,933.3±12,775.0 |
216,000.0±42,895.0 |
3.467 |
0.002 |
|
Surgery fee |
169,826.7±27,267.2 |
164,320.0±8,519.1 |
0.747 |
0.462 |
|
Total cost of X-ray |
30,000.0±0 |
29,933.3±7,272.0 |
0.035 |
0.972 |
|
Cost of Scotch cast material |
5,900.0±0 |
5,506.7±1,523.3 |
1.000 |
0.326 |
|
Cost of cast application |
4,200.0±0 |
3,920.0±1084.4 |
1.000 |
0.326 |
|
Total cost of feeding |
28,673.3±16,400.6 |
44,200.0±68,280.9 |
0.856 |
0.399 |
|
Total amount spent on admission fees |
33,426.7±20288.0 |
34,266.7±15198.1 |
0.128 |
0.899 |
|
Follow-up consultation fee |
8,000.0±0 |
7,466.7±2065.6 |
1.000 |
0.326 |
|
Total cost |
455,960.0±46,967.3 |
505,613.3±113,345.9 |
1.567 |
0.128 |
DISCUSSION
The aim of the study was to determine and compare the union and non-union rates, the associated complications and the mean total cost implication in the management of open tibia shaft fractures using Illizarov frame fixator and linear rail system (LRS).
In this study, union rate was noticed not to have any statistically significant difference between the Illizarov frame and LRS groups. This was also noticed to be comparable to the findings of Pal et al [6].
Numerous studies where LRS was the fixator being evaluated such as Kale et al., Singh et al., Ajmera et al., and Soni et al. [9-12], reported union rates which were comparable to those of the LRS group in our study.
Similarly, studies where Illizarov frame was the fixator under review such as Vyas et al., Inan et al., Sidhathan et al., Wani et al. and Tarek Aly [13-17], reported comparable union rates to that of the Illizarov frame fixator group in our study.
In our study, pin tract infection was noted to be the most common complication and there was no statistically significant difference between the Illizarov frame and LRS groups. Most other studies [6-19], also reported pin tract infection as the commonest complication while on the fixators.
Our quest to compare the mean total cost implication of the management of open tibia shaft fractures using the fixators under review, was born out of the notion in our locality by some orthopaedic surgeons [20], that the Illizarov frames were more expensive, cumbersome and also not readily available even when there is need to use them.
In view of the current standard of living within the country and also because patients pay out of pocket to access health care services, it became pertinent to compare the mean total cost implication for any significant difference when used to manage these patients with open tibia shaft fractures.
In this study, we found a statistically significant difference between the mean cost price for purchasing these external fixators. We realized that the retail vendors increased the prices of the Illizarov frames far more than the price at which the wholesale vendors were selling thus creating a false impression of the Illizarov frames being more expensive.
However, the mean total cost implication for the management of those patients with open tibia shaft fractures reported a difference which was not statistically significant. The results from this study have shown that the Illizarov frame fixator and the LRS fixator are the ideal devices needed in a resource poor country since their outcomes are similar, complication rates low and both still have comparable cost implication when either of the fixators are used.
CONCLUSIONS AND RECOMMENDATIONS
This study has shown that the burden associated with the management of open tibia shaft fractures in a resource poor country can be relatively minimized by using either the Illizarov frame fixator or the LRS. Thus, it is important for orthopaedic surgeons to learn proficiency in the use of both devices in order to maximize the outcomes of patient care.
The government is hereby called upon to help minimize this rising incidence of road traffic accident (RTAs) since we are residing in a country with dwindling economy and patients need to pay out of pocket to access good health care.
REFERENCES
- Nicoll EA. Closed and open management of tibial fractures. Clin Orthop Relat Res. 1974; 105: 144-153.
- Wanjema S, Oluoch R, Ayumba BR, Lelei L. Tibial Diaphyseal Fractures: Aetiology, morphology and treatment in adult patients at Moi Teaching and Referral Hospital, Eldoret, Kenya. East Afr Orthop J. 2020; 14: 8-13.
- Ibeanusi SEB, Ekere AU. Epidemiology of open tibial fractures in a teaching hospital. P H Med J. 2007; 1: 156-160.
- Madubueze CC, Chukwu CO, Omoke NI, Oyakhilome OP, Ozo C. Road traffic injuries as seen in a Nigerian teaching hospital. Int Orthop. 2011; 35: 743-746.
- Elachi IC, Okunola BB, Yongu WT, Onyemaechi NO, Odatuwa- Omagbemi OD, Ahachi CN, et al. Motorcycle-related injuries at a university teaching hospital in north central Nigeria. Niger Med J. 2014; 55: 452-455.
- Pal CP, Kumar H, Kumar D, Dinkar KS, Mittal V, Singh NK. Comparative study of the results of compound tibial shaft fractures treated by Ilizarov ring fixators and limb reconstruction system fixators. Chin J Traumatol. 2015; 18: 347-351.
- Onyemelukwe MF, Okunola MO, Owoola AM, Oladiran AB, Adeoye-Sunday II, Anejukwo AA, et al. Comparative outcome study of the management of open tibia shaft fractures using Ilizarov frame fixatorand linear rail system at University College Hospital, Ibadan, Nigeria. Int Orthop. 2025; 49: 1973-1980.
- Jangle R. Treatment of Compound Tibial Diaphyseal Fractures by Ilizarov Method: A Retrospective Study. Int J Sci Res IJSR. 2020; 9: 883-886.
- Kale AB, Patole VV, Argekar HG, Sharan s, Goregaonkar AB. Limb reconstruction system as a primary and definitive mode of fixation in open fractures of long bones. Int J Res Orthop. 2017; 3: 167-171.
- Singh P, Singh SK, Gill SPS. Management of Compound fractures of tibia by Limb Reconstruction System (LRS). J Bone Jt Dis. 2020; 35: 29-34.
- Ajmera A, Verma A, Agrawal M, Jain S, Mukherjee A. Outcome of limb reconstruction system in open tibial diaphyseal fractures. Indian J Orthop. 2015; 49: 429-435.
- Soni JK, Kulkarni S, Khodnapur G, Bagewadi R, Nandi SS. Management of Open Tibial Diaphyseal Fractures by Limb Reconstruction System As Primary and Definitive Treatment: A Prospective Cohort Study. Cureus. 2023; 15: e39774.
- Vyas DT, Shah DH, Shah DA, Gajjar DS, Chaudhari DV, Siddhapuria DP. Retrospective study of open tibial diaphyseal fractures type IIIA and IIIB by Ilizarov method. Int J Orthop Sci. 2017; 3: 507-512.
- Inan M, Halici M, Ayan I, Tuncel M, Karaoglu S. Treatment of type IIIA open fractures of tibial shaft with Ilizarov external fixator versus unreamed tibial nailing. Arch Orthop Trauma Surg. 2007; 127: 617- 623.
- Sidharthan S, Sujith A, Rathod AK, Pathak RH. Management Of High Energy Tibial Fractures Using Ilizarov Apparatus. Internet J Orthop Surg. 2005; 3.
- Wani N, Baba A, Kangoo K, Mir M. Role of early Ilizarov ring fixator in the definitive management of type II, IIIA and IIIB open tibial shaft fractures. Int Orthop. 2011; 35: 915-23.
- Tarek A. Role of Ilizarov Ring Fixator in Management of High Diaphyseal Fractures. EC Orthopaedics. 2020; 11: 13-26.
- Kayode MO, Adewole OA, Shoga MO, Giwa SO. EXPERIENCE WITH MANAGING COMPLICATED FRACTURES USING ILIZAROV PRINCIPLE IN LAGOS, NIGERIA. J West Afr Coll Surg. 2017; 7: 24-43.
- Paley D. Problems, obstacles, and complications of limb lengtheningby the Ilizarov technique. Clin Orthop Relat Res. 1990; 250: 81-104.
- Dakbana T, Nyaku F, Bunu B. Management of traumatic segmental bone loss using linear rail system, our experience at the University of Maiduguri Teaching Hospital, Maiduguri, Nigeria. Sahel Med J. 2016; 19: 171-174.