Efficacy of Ultrasound Guided Nerve Block versus Intravenous Tramadol Injection for Pain Relief in Patients with Fresh Lower Limb Fractures
- 1. Department of Anesthesia, Puducherry, India
Abstract
With the increasing incidence of trauma and the financial implications thereon, the necessity for early debridement, early fixation of fractures and early discharge needs to be underlined. High velocity road traffic accidents lead to lot of compound fractures, contaminated crush injuries and simple fractures as well.
Keywords
• Fractures
• Orthopedic
• Pain
Citation
Mohamed AS (2024) Efficacy of Ultrasound Guided Nerve Block versus Intravenous Tramadol Injection for Pain Relief in Patients with Fresh Lower Limb Fractures – A Hospital Based Study in Puducherry. J Fract Sprains 3(1): 1010.
INTRODUCTION
Hip and femur fractures remain one of the most common and serious injury in elderly who are at an increased risk of complications if the pain is sub optimally managed [1]. It is shown that the number of expected hip fracture in India will increase from 3, 31, 898 in 2018 to 7, 92, 334 in 2050 [2]. Pain is the most common reason that brings the patients to the Emergency department [3]. Patients with fresh fractures of lower limb are in severe pain upon arrival at the emergency department, following that the patient needs to be transferred from stretcher to stretcher to multiple places for imaging, for orthopedic examination and for necessary fracture reduction procedure or shifting to operation theatre or ward which further aggravates the pain [4].
The consequences of pain are due to activation of neuro- hormonal stress response which cause release of catecholamines from the adrenal medulla and release of norepinephrine from the presynaptic nerve terminals thereby increasing sympathetic activity all of which may lead to adverse cardiovascular events like tachycardia, hypertension and increased myocardial oxygen demand, this may be detrimental especially in elderly and in those with preexisting coronary artery disease. Untreated pain and inadequate analgesia leads to increased risk for depression, sleep disturbances, delirium and increased adverse outcome in the postoperative period including functional decline, permanent cognitive impairment, delayed mobilization and prolonged hospital stay [5]. Inadequate pain relief leads to anxiety to the patient, the family and the doctor so rapid provision of effective analgesia should begin at presentation to the Emergency Department [6]. Pain relief can be done through oral analgesics and regional analgesia techniques [7]. NSAIDs and Opoids has some contraindication and side effects like respiratory depression on fracture treatment, in such conditions, regional analgesia offers an attractive alternate to systemic analgesics.
Ultrasound guided peripheral nerve block can be used as a safe and potent tool for managing acute pain in the emergency department as it does not require air way monitoring and profound analgesia is obtained without the adverse effects associated with systemic analgesics (respiratory depression, hemodynamic effects, or obtundation of consciousness) and it also reduces the need for systemic analgesics in the pre and postoperative period [3]. Ultrasound allows direct visualization of the nerves and their relationship to other structures and hence reduces the volume of drug needed and incidence of vascular injury, improves quality of block, spread of the local anaesthetic can be visualized and success rate is increased. Local anaesthetics with or without additives can be used either as a single shot technique or a continuous infusion through an indwelling catheter, looking at the feasibility and enormous rates of ultrasound guided nerve blocks for pain relief, tertiary care institutions have adopted institutional protocols to extrapolate the same results to provide pain relief to a patient with acute trauma [8,9]. With this rationale, the objective of the study was to determine the efficacy of ultrasound guided nerve block and intravenous tramadol injection for pain relief in patients presenting with fresh lower limb fractures in emergency department through hemodynamic parameters, visual analogue scale and 5 tiered likert scale and to compare the same.
MATERIAL AND METHODS
The present prospective randomized controlled trial study which was conducted for a period of 18 months in emergency department of Indira Gandhi Government General Hospital and Post gradute Institue, Puducherry. Patients with fresh lower limb fractures in age group of 15-75 years and ASA (American society of anesthesiologists) physical status 1 and 2 were included in the study. Patients with ASA physical status 3 and above, coagulation abnormalities, sepsis, neurological deficits, infection at local site and pregnant mother were excluded. A total of 108 participants were included, considering 54 in each study group (Group (NB) – PATIENTS RECEIVING ULTRASOUND GUIDED LOWER LIMB NERVE BLOCKS. Group (T) - PATIENTS RECEIVINGINTRAVENOUS TRAMADOL). Using open epi software version 3.01, the sample size was calculted with 95% confidence interval, 80% power, ratio of 1:1 and 24% as proportion of subjects achieving good graded analgesia [10].
Equipments/Supplies
This procedure requires: Anesthesia workstation, Laryngoscope with different size blades, Endotracheal tubes, Sonoscape S12 Ultrasound machine with linear and curvilinear probes, Ultrasound gel, Antiseptic solution, Sterile tray with sterile towel, gauze packs, sponge holding forceps, clinge drape, disposable 10ml, 5ml syringes, sterile gloves, 23 G and 26 G spinal needle. Monitors: heart rate, noninvasive blood pressure, pulse oximeter, electrocardiogram. Drugs: 0.25% bupivacaine, Inj. tramadol 2ml ampoule (50mg/ml), emergency drugs needed for resuscitation like adrenaline, atropine and normal saline.
Procedure
After obtaining Institutional Ethical and Scientific Committee clearance, each patient were explained about the study and informed consent taken was obtained. Further, randomized into two groups by sealed envelope method.
Group A
As soon as patient arrived at the emergency department, after initial assessment by the orthopedician. Only fully resuscitated and hemodynamically stable patients were taken up for the procedure in the operation theatre. Baseline vitals such as pulse rate, noninvasive blood pressure, saturation in room air, respiratory rate, electrocardiogram were recorded and hemoglobin, bleeding time, clotting time were obtained. Intravenous access secured with 18G IV cannula and fluids were started. All patients were premedicated with injection ondansetron 4mg and injection ranitidine 50mg through i.v route. After assessment of all the above parameters the patient received appropriate block with appropriate volume of local anaesthetic with the guidance of ultrasound as described below:
Fascia Iliaca Block: Patient were placed in supine position. The Ultrasound Machine with the linear array probe covered with sterile dressing after applying ultrasound gel was mobilized to the operating table. The probe was placed in a horizontal direction over the anterior part of thigh just below the inguinal ligament. Probe was tilted to identify the hyperechoic fascia iliaca lying superficial to the iliopsoas muscle. Ultrasound monitor setting, gain, focus, depth, and frequency were adjusted according to the image scanned. Femoral artery was identified first. The iliacus muscle covered by fascia iliaca was identified lateral to the artery. Local anesthetic 2ml of 2%lignocaine was used to make a skin wheal with 24G hypodermic needle. A 23G spinal needle was then inserted in plane to the ultrasound beam. The needle was then advanced until the tip of the needle pierced the fascia iliaca (appreciating the give way feel as the fascia is pierced) and after negative aspiration, 1-2 ml of local anesthetic was injected to confirm the proper injection plane between the fascia and iliopsoas. Then 25-35 ml of 0.25% bupivacaine was injected and its spread toward the femoral nerve medially and underneath the sartorius muscle laterally was visualized on the ultrasound.
Sciatic Nerve Block: It was achieved with the classic posterior approach of Labat (subgluteal approach). Patient was placed in lateral decubitus position with the limb to be blocked flexed at hip and knee. The two bony landmarks, greater trochanter and ischial tuberosity were palpated and marked with a skin marker. The skin was disinfected and transducer was positioned to identify the sciatic nerve which appears as an oval hyperechoic structure. The ultrasound setting used was adjusted to a depth of 8-10 cm. The gain and focus were adjusted according to the image scanned. Transducer manipulated by slightly tilting proximally or distally to visualize the nerve out of the background of the two muscles (namely the gluteus maximus and quadriceps femoris). Local anesthetic 2ml of 2%lignocaine were used to make a skin wheal with 24G hypodermic needle. A 23G spinal needle was then inserted in plane, from the lateral aspect of the transducer, and advanced towards the sciatic nerve. Needle tip was positioned. After careful aspiration, 2 mL of 5% dextrose was used to hydrolocate the nerve. Then 20-30 mL of 0.25% bupivacaine were injected in smaller aliquots to ensure that the sciatic nerve was surrounded with the local anesthetics.
Femoral Nerve Block: Patient was placed in the supine position. The skin over the femoral crease was disinfected and the transducer was positioned transversely on the femoral crease, and moved slowly in a lateral-to-medial direction to identify femoral artery, vein and the nerve. After identification of the nerve, a skin wheal of local anesthetic was made approximately 1 cm away from the lateral edge of the transducer. A 26G needle was then inserted in plane in a lateral-to medial direction and advanced towards the femoral nerve. Once needle tip were positioned adjacent to the lateral aspect of the nerve, after careful aspiration, 1–2 mL of local anesthetic was injected to confirm proper needle placement, then 10–20 mL of 0.25% bupivacaine were injected and its proper deposition was observed by femoral nerve being displaced by the spread of the local anesthetic around the nerve. Then the patient was shifted to the post-operative ward where the vitals were monitored for 1 hour and then the patient was shifted to trauma unit.
Group B
Patients were administered with Intravenous (iv) Tramadol 1mg/kg injection.
The hemodynamic variables like heart rate, noninvasive blood pressure, oxygen saturation, respiratory rate and visual analogue scale were recorded and scored after 30 minutes of the block and iv tramadol injection. Followed at hourly intervals for 4 hour. After 4 hours of intervention, patient satisfaction was measured using 5 tiered Likert scale ranging from (1 to 5) highly satisfied – 5, satisfied - 4, Neutral and no opinion - 3, Not satisfied- 2 and Highly unsatisfied – 1.
Data analysis
The collected data were entered in MS Excel and were analyzed using SPSS (Statistical Package for the Social Sciences) version 19.0. Categorical variables in both NB (nerve block) and T (IV Tramadol) groups were expressed in frequencies, proportions and percentages. Continuous variables were expressed in mean and standard deviation. Chi-square test were used to find out the significant difference in proportions and significant difference of mean were calculated t-test. P value <0.05 was considered significant between the NB and T groups.
RESULTS
Table 1, of the total 108 subjects enrolled in the study with 54 each for Nerve block and tramadol groups.
Table 1: Sociodemographic details of the study participants
|
Variables |
NB group (n=54) |
T group (n=54) |
||
|
N |
% |
N |
% |
|
|
Age (in years) |
||||
|
<40 |
6 |
11.1% |
3 |
5.6% |
|
40 to 49 |
17 |
31.5% |
20 |
37.0% |
|
50 to 59 |
19 |
35.2% |
27 |
50.0% |
|
≥ 60 |
12 |
22.2% |
4 |
7.4% |
|
Gender |
||||
|
Female |
23 |
42.6% |
14 |
25.9% |
|
Male |
31 |
57.4% |
40 |
74.1% |
|
Diagnosis |
||||
|
Fracture Both Bone |
13 |
24.1% |
29 |
53.7% |
|
Fracture Tibia |
2 |
3.7% |
0 |
0% |
|
Intertrochanter Fracture |
25 |
46.3% |
23 |
42.6% |
|
Neck Of Femur |
2 |
3.7% |
0 |
0% |
|
Shaft Of Femur Fracture |
7 |
13.0% |
0 |
0% |
|
Subtrochanteric Fracture |
5 |
9.3% |
2 |
3.7% |
|
ASA status |
||||
|
1 |
40 |
74.1% |
45 |
83.3% |
|
2 |
14 |
25.9% |
9 |
16.7% |
Maximum subjects 19 (35.2%) and 27 (50%) were from 50 to 59 age group for NB and T group with mean (SD) 50.78 (7.9) and 50.39 (6.4) respectively. Majority were male 31(57.4%) and 40 (74.1%) in both the group. Intertrochanter fracture 25(46.3%) and fracture of both bone 29(53.7%) were reported maximum by NB and T group respectively. Majority of the subjects belonged to ASA status 1 in both the groups. The mean(SD) SBP and DBP were found to be 140(15.6), 148(12.3) and 85.7(9.7), 91(11.3) for NB and T groups respectively while the mean SBP is 8.38 mm hg less in NB than T group which is significant as p=0.03. The mean (SD) Pulse rate, respiratory rate and SPO2 were found to be 112(10.6), 113(14.7); 14.5(3.2), 15.8(4.5) and 99.4(1.0), 99.4(1.2) for both the groups.
Table 2, There is a significant difference in pain score between NB and T groups with 4.7, 5.4, 5.7, 5.9 and 6.0 score more in T group as compared to NB group at 1/2H, 1H, 2H, 3H and 4H timeline respectively and this mean difference is strongly significant at each level as P<0.001 in each case. The mean pain score before and after the nerve block and tramadol are 9.5(0.8), 1.3(1.4) and 9.61(0.52), 7.38(1.96) respectively (p<0.001 strongly sig.)
Table 2: Test of significance for mean pain score in test groups at various time intervals
|
Time interval |
Pain score Mean (SD) |
Mean difference (mmHg) more in T group |
95% CI of the Difference |
Sig. |
||
|
NB group (Nerve Block) |
T group (IV Tramadol) |
Lower |
Upper |
|||
|
PS_0 H |
9.556 |
9.611 |
-.0556 |
-.3232 |
.2121 |
P=0.682 |
|
(0.8393) |
(0.5290) |
Non sig. |
||||
|
PS_1/2H |
1.981 |
6.741 |
-4.7593 |
-5.3374 |
-4.1811 |
P<0.001 |
|
(1.3666) |
(1.6504) |
Strongly sig. |
||||
|
PS_1H |
1.630 |
7.093 |
-5.4630 |
-6.0526 |
-4.8733 |
P<0.001 |
|
(1.2483) |
(1.7938) |
Strongly sig. |
||||
|
PS_2H |
1.407 |
7.204 |
-5.7963 |
-6.4005 |
-5.1921 |
P<0.001 |
|
(1.3106) |
(1.8159) |
Strongly sig. |
||||
|
PS_3H |
1.370 |
7.333 |
-5.9630 |
-6.5969 |
-5.3290 |
P<0.001 |
|
(1.3500) |
(1.9230) |
Strongly sig. |
||||
|
PS_4H |
1.315 |
7.389 |
-6.0741 |
-6.7375 |
-5.4106 |
P<0.001 |
|
(1.4772) |
(1.9659) |
Strongly sig. |
||||
NB group (Nerve Block), T group (IV Tramadol)
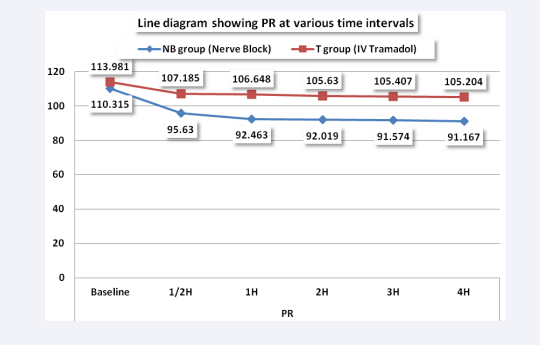
There is a significant difference in PR between NB and T groups with 11.5, 14.1, 13.6, 13.8 and 14.0 more in T group as compared to NB group and this mean difference is strongly significant at each level as P<0.001 in each case. Mean PR before and after the nerve block are 110.31(18.63) and 91.16 (5.98) respectively (p<0.001 strongly significant) whereas the same before after Tramadol are 113.98(14.5) and 105(12.0) [Figure 1].
Figure 1: Line diagram for mean PR in Test groups at various time intervals
There is a significant difference in mean SBP between NB and T groups with 5.2, 6.2, 7.6, and 8.4 mmHg more in T group as compared to NB group at 1H, 2H, 3H and 4H timeline respectively and this mean difference is strongly significant at each level as P<0.001 in each case. The mean systolic BP before and after nerve block are 148.79(12.36) and 131.98(9.86) mmHg respectively (p<0.001 strongly sig) [Table 3].
Table 3: Test of significance for mean systolic blood pressure in Test groups at various time intervals
|
Time interval |
SBP Mean (SD) |
Mean difference |
95% CI of the Difference |
Sig. |
||
|
NB group (Nerve Block) |
T group (IV Tramadol) |
Lower |
Upper |
|||
|
SBP_0 H |
148.79 (12.36) |
146.77 (15.90) |
2.01 |
-3.4178 |
7.4548 |
P=0.463 Non sig. |
|
SBP_1/2H |
139.05 (11.76) |
141.57 (14.46) |
-2.5185 |
-7.5485 |
2.5115 |
P=0.323 Non sig. |
|
SBP_1H |
135.92 (10.81) |
141.16 (14.07) |
-5.2407 |
-10.0292 |
-.4523 |
P=0.032 Strongly sig. |
|
SBP_2H |
134.20 (10.19) |
140.42 (13.51) |
-6.2222 |
-10.7885 |
-1.6559 |
P=0.008 Strongly sig. |
|
SBP_3H |
132.68 (10.31) |
140.33 (12.54) |
-7.6481 |
-12.0299 |
-3.2664 |
P=0.001 Strongly sig. |
|
SBP_4H |
131.98 (9.86) |
140.46 (13.08) |
-8.4815 |
-12.9030 |
-4.0600 |
P<0.001 Strongly sig. |
NB group (Nerve Block), T group (IV Tramadol)
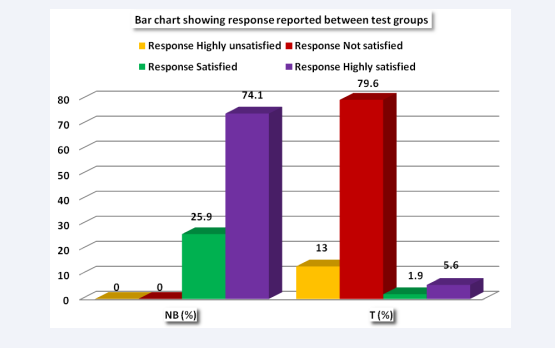
Maximum subjects in T group 43(80%) are not satisfied whereas 40(74%) subjects in NB group are highly satisfied with the treatment modality. This association is strongly significant as p<0.001 [Figure 2].
Figure 2: Bar chart showing details of patient satisfaction scale.
DISCUSSION
From our study, there is significant difference in mean systolic blood pressure and pulse rate observed between two groups and that there is no significant difference in the diastolic blood pressure, respiratory rate and oxygen saturation. The mean (SD) systolic blood pressure was found to be 140(15.6) and 148(12.3) for nerve block and Tramadol groups respectively P=0.03 (strongly significant). Buttner et al. [11], in their study compared ultrasound guided peripheral nerve block with systemic analgesic in emergency department to determine which of these modalities effectively reduced pain intensity and severity. They concluded that ultrasound guided nerve block effectively reduced the pain, which was in concurrence with our study. In our study there was significant decrease in mean systolic blood pressure and pulse rate observed in nerve block group which may be attributed to the fact that catecholamine surge in response to fracture had subsided well in the nerve block group when compared to the weak opioid analgesic tramadol, whereas in the above study done by Buttner et al. [11], there was no significant difference in the hemodynamic parameters between the two groups, which may have been due to the use of highly potent opioid analgesic in the control group. In their study, hypoxemia had occurred in two cases which was attributed to the use of midazolam, fentanyl. Whereas, in our study no patients had hypoxemia and this may be due to the use of intravenous tramadol which is less prone to cause respiratory depression at therapeutic dose and pain is a physiological antagonist to respiratory depression caused by opioids.
Our study result was in concordance with the study by Nejati A et al. [3], where they observed a significant decrease in mean systolic blood pressure and pulse rate after the nerve block. The mean systolic blood pressure before and after nerve block was 125.3 ± 5.3 and 119.7 ± 4.8 mmHg, respectively (p < 0.001). Also, mean pulse rate before and after nerve block were 94.76 ± 4.4 and 87.23 ± 5.6, respectively (p < 0.001). Our study demonstrated that pain relief was superior in the nerve block group compared with the tramadol group during the preoperative period. This observation was similar to the study results conducted by Yanhui ma et al. [12], in which they compared the efficacy of ultrasound guided fascia iliaca block and systemic analgesics for preoperative pain management in hip fracture patients with pain score using visual analogue scale (VAS) as the primary outcome . They concluded that ultrasound guided nerve block provides better control of pain than systemic analgesics with significant reduction in the VAS pain score observed in nerve block group both at rest (p=0.023) as well as during passive movement (p<0.05) which may be due to the use of ultrasound in identification of the fascia allowing real time imaging of the needle while performing blocks and to confirm the spread of drug under the fascia.
Similar results were observed in a study conducted by Lee et al. [13], where they observed a significant difference in the reduction in pain score (P<0.001); the number of patients whose pain score decreased to less than 4 after the pain treatment was 9 out of 22 (40.9%) in the control group, and 24 out of 25 (96.0%) in the study group. The magnitude of the decrease in the pain score was also significant (P<0.001); the difference between the initial pain score and the pain score at maximum pain relief was 7 (Interquartile range (IQR), 6 to 7) in the regional anesthesia group, and 4 (IQR, 3 to 5) in the morphine group. Decrease in pain score was significantly higher in patients who received nerve block compared to those who received intravenous morphine (P<0.001) after 4 hours of intervention. When a three-in-one femoral nerve block is performed under ultrasound guidance, the local anesthetic is more accurately injected into the desired region (perineurally) enhancing the nerve blockade thereby better pain relief.
A study by Beaudoin et al. [14], reported similar results to our study who compared ultrasound guided nerve block with parenteral opioids for analgesia in patients with femoral neck fractures in the emergency department. They observed that over the 4-hour study period, the median pain score in the nerve block group reduced from a mean NRS of 8 at baseline to 4 after 4 hour and there was significant decrease in pain intensity in patients in the FNB (femoral nerve block) group (p<0.01) when compared to parenteral opioid group. The results of study is in concordance with our study where patient who received ultrasound guided nerve block experienced significantly greater pain relief than those who received parenteral tramadol (p <0.001).
In the study done by Buttner et al. [11], wherein they compared the analgesic efficacy of ultrasound guided nerve blocks with systemic analgesics for extremity injury in emergency department. Patients satisfaction with either mode of intervention were assessed using 6 tiered likert scale. They found that better patient satisfaction was observed in the peripheral nerve block group with a mean score of 1.2±0.6 compared to systemic analgesic group with a score of 2.0±1.5. All patients of the Peripheral nerve block group and only 50.0% of the systemic analgesic group would recommend their respective technique (p<0.01).
Our study has similar results to the study conducted by Yanhui et al. [12], they observed better patient satisfaction scores in the nerve block group when compared to the systemic analgesic group (P<0.001) which was in concordance with our study where 74% of the patients in the nerve block group reported a higher satisfaction score when compared to only 3% in the intravenous tramadol group. This association is strongly significant as p<0.001. Nejati A et al. [3], conducted a study to investigate the efficacy and feasibility of ultrasound-guided nerve blocks in emergency department and satisfaction of the patient with the intervention. It was measured using a 5 tiered likert scale. In their study 54.3% of the patients were highly satisfied (Likert scale 5), and 32.6% were satisfied (Likert scale 4) with ultrasound guided peripheral nerve block which was in concordance with our study. They also concluded that Ultrasound guided nerve block of extremities is a safe and effective method that can be used for pain management in the emergency department.
CONCLUSION
With this study, ultrasound guided peripheral nerve block was found to be a safe and effective method of providing pain relief when compared to conventionally used intravenous tramadol in patients with fresh fracture of lower limb at our emergency department. This was better in terms of hemodynamic parameters, pain score and overall patient satisfaction. All these are statistically proven in our study. Thus we recommend the use of ultrasound guided nerve blocks for pain relief in fresh fractures on arrival at emergency department.
REFERENCES
- Ritcey B, Pageau P, Woo MY, Perry JJ. Regional Nerve Blocks for Hip and Femoral Neck Fractures in the Emergency Department: A Systematic Review. CJEM. 2016; 18: 37-47.
- Cheung CL, Ang SB, Chadha M, Chow ES, Chung YS, Hew FL, et al. An updated hip fracture projection in Asia: The Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia. 2018; 4: 16-21.
- Nejati A, Teymourian H, Behrooz L, Mohseni G. Pain management via Ultrasound-guided Nerve Block in Emergency Department; a Case Series Study. Emerg (Tehran). 2017; 5: e12.
- Zaki HA, Iftikhar H, Shallik N, Elmoheen A, Bashir K, Shaban EE, et al. An integrative comparative study between ultrasound-guided regional anesthesia versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: A systematic review and meta-analysis. Heliyon. 2022; 8: e12413.
- Riddell M, Ospina M, Holroyd-Leduc J. Use of Femoral Nerve Blocks to Manage Hip Fracture Pain among Older Adults in the Emergency Department: A Systematic Review. CJEM. 2016; 18: 245-252.
- Reavley P, Montgomery AA, Smith JE, Binks S, Edwards J, Elder G, et al. Randomised trial of the fascia iliaca block versus the ‘3-in-1’ block for femoral neck fractures in the emergency department. Emerg Med J. 2015; 32: 685-689.
- Rowlands M, Walt GV, Bradley J, Mannings A, Armstrong S, Bedforth N, et al. Femoral Nerve Block Intervention in Neck of Femur Fracture (FINOF): a randomised controlled trial. BMJ Open. 2018 10; 8: e019650.
- Marhofer P, Schrögendorfer K, Wallner T, Koinig H, Mayer N, Kapral S. Ultrasonographic guidance reduces the amount of local anesthetic for 3-in-1 blocks. Reg Anesth Pain Med. 1998; 23: 584-588.
- Abrahams MS, Aziz MF, Fu RF, Horn JL. Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2009; 102: 408-417.
- Ningawal BK, Acharya G, Arora KK. Preoperative Femoral Nerve Block In Extracapsular Femoral Neck Fractures: A Clinical Evaluation Of Pain Relief During Transportation To Operation Theatre Wjpmr. 2016; 2: 143-146.
- Büttner B, Mansur A, Kalmbach M, Hinz J, Volk T, Szalai K, et al. Prehospital ultrasound-guided nerve blocks improve reduction- feasibility of dislocated extremity injuries compared to systemic analgesia. A randomized controlled trial. PLoS One. 2018; 13: e0199776.
- Ma Y, Wu J, Xue J, Lan F, Wang T. Ultrasound-guided continuous fascia iliaca compartment block for pre-operative pain control in very elderly patients with hip fracture: A randomized controlled trial. Exp Ther Med. 2018; 16: 1944-1952.
- Lee HK, Kang BS, Kim CS, Choi HJ. Ultrasound-guided regional anesthesia for the pain management of elderly patients with hip fractures in the emergency department. Clin Exp Emerg Med. 2014; 1: 49-55.
- Beaudoin F, Haran J, Liebmann O. A Comparison of Ultrasound-guided Three-in-one Femoral Nerve Block Versus Parenteral Opioids Alone for Analgesia in Emergency Department Patients with Hip Fractures: A Randomized Controlled Trial. Acad Emerg Med. 2013; 20: 584-591.