Treatment of Humerus Diaphyseal Fractures with Minimally Invasive Plate Osteosynthesis
- 1. Department of Orthopaedics, Postgraduate Institute of Swasthiyog Pratisthan Miraj, India
Abstract
Introduction: Humerus fractures remain to be in the spectrum of multiple treatments. With the evolution of surgical care, newer methods of treating humerus fractures are coming to light, most important being minimally invasive plate osteosynthesis (MIPO). MIPO has discreet advantages with regards to minimal dissection, preservation of fracture biology and rotator cuff, and providing stability with elasticity to the bone plate construct. It is evident that biological fixation is superior to mechanical fixation, which forms the basis of MIPO.
The aim of our study was to evaluate the functional and radiological outcome of MIPO.
Materials and methods: 33 cases were studied over 2 years. Closed and open fractures, polytrauma patients, unstable fractures were included in the study. Pathological fractures, non-unions and malunions, refracture, and patients presenting after a delay of 21 days were excluded. 8 cases were aided by external fixators. Patients were followed up with UCLA and MEPS scores.
Results: 100 % union was seen in our series with an average union time of 10.94 ± 2.4 weeks. Majority of the cases had excellent UCLA shoulder score and MEP scores. The 3 cases of post traumatic radial nerve palsy recovered after surgery. Mean angulations of 6.09° was seen postoperatively. Infection was seen in 2cases which resolved later.
Conclusion: MIPO brings out a balance in fracture stability and biology preservation. It is thus a very novel and successful way of treating humerus with careful patient selection and mastering the art of this surgery.
Citation
Kulkarni M, Kulkarni V, Kulkarni S (2017) Treatment of Humerus Diaphyseal Fractures with Minimally Invasive Plate Osteosynthesis. J Fract Sprains 1(1): 1007.
Keywords
• Humerus
• MIPO
• Exfix assisted
• Anterior bridge plating
ABBREVIATIONS
MIPO: Minimally Invasive Plate Osteosynthesis; IMN: Intramedullary Nailing; ORPO: Open Reduction Plate Osteosynthesis; UCLA: University of California; Los Angeles; MEPS: Mayo Elbow Performance Score
INTRODUCTION
The fractures of shaft humerus constitute around 1-2 % of all fractures in the human body and 14% of the entire humerus fractures [1]. These fractures are caused by direct or indirect trauma, ground level falls, road traffic accidents, with osteoporosis contributing to the intensity of the injury [2,3]. Radial nerve injury is most commonly encountered during diaphysis fractures on account of its anatomy.
Many methods, both surgical and nonsurgical have been developed to manage these fractures with a new method of Minimally Invasive Plate Osteosynthesis being currently studied [3,4].
As the surgical practices are evolving, more importance is now given to soft tissues, and fracture hematoma which are major factors in fracture healing.
MIPO is a non-extensile surgical method of fixing the fracture by preserving the fracture biology. Thus the stripping of tissues is prevented as well as the rotator cuff is spared from iatrogenic trauma [5].
The goal of treatment is to reduce the fracture, maintain reduction in proper alignment, length and rotation and facilitate early joint movement.
The aim of this study was to evaluate the new MIPO technique based on clinical radiological and functional outcomes.
The hypothesis to be tested in this study is that MIPO is a good method of treating humerus diaphysis fractures with regard to clinical and functional outcomes.
MATERIALS AND METHOD
This is an observational prospective study conducted at our institute from May 2014 to May 2016. A total of 33 patients were studied in this time frame. All patients were informed about the study and informed consent was obtained. Patients with diaphyseal fractures of humerus AO/OTA type A B C, open fractures type 1,2 and 3A 3B; polytrauma patients; unstable humerus fractures; age more than 18 years and patients in whom conservative management had failed were included in the study [6-9]. Patients having pathological fractures; open type 3C injuries; septic or aseptic nonunion of humerus; refractures of humerus and patients presenting with a delay of 21 days were excluded from the study [10]. In case of pathological fracture, manipulation of fracture fragments may cause further fracture, thus excluded from the study. In nonunion whether septic or aseptic, exploration of the fracture site is necessary and closed procedure should be avoided. Fractures in patients who presented with a delay of 21 days or more, demand an open procedure as it is difficult to attain reduction with the soft tissue interpositions and callus. Open trauma requires thorough debridement for which opening of fracture site is necessary and is thus excluded from our study. After thorough examination of the patient surgery was performed using the following method [11-13] shown in Figure 1.
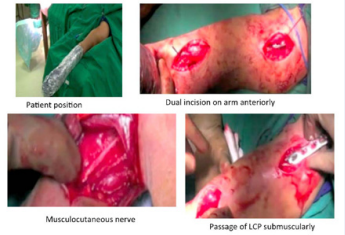
Figure 1: Position and incision in MIPO
In supine position with shoulder abducted 90° and elbow extended and supinated, two anterior incisions were taken. The distal incision was taken 4 cm from the elbow crease being 5-7 cm in length. Plane was developed by retracting the biceps medially and visualizing the brachialis and musculocutaneous nerve. The brachialis was split in the middle and the anterolateral surface of humerus is exposed. Routinely the radial nerve was not dissected but in certain cases of distal shaft fractures, it was necessary. Proximally Coracoid process of the scapula is palpated and an incision 5-6 cm vertically was made 5 cm inferior to it. Deltopectoral plane was used to approach upper end of humerus. Certain fibers of pectoralis major and deltoid were released for better plate positioning.
In cases where external fixator was applied to the humerus, two small incisions were taken on the lateral aspect of the humerus, on the medial epicondyle and proximal humerus. Care was taken not to injure the axillary nerve by proximal pin. 4 mm schanz pins were inserted and fracture reduced under image intensifier guidance and external rod applied, as shown in Figure 2.
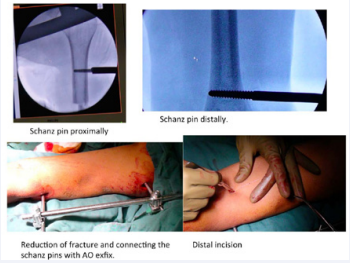
Figure 2: Exfix assisted MIPO
From the distal to the proximal incision a tunnel was made sub-muscularly by a tunneling instrument, forceps or in our case a 4.5mm locking plate. Locking plate was used for its obvious advantages [14-19].
The plate is passed close to the bone and exited from the proximal site. Under the image intensifier the plate is positioned on the anterior surface of the bone and temporarily fixed by 2 1.2 mm K-wires in each segment, as shown in Figure 3.
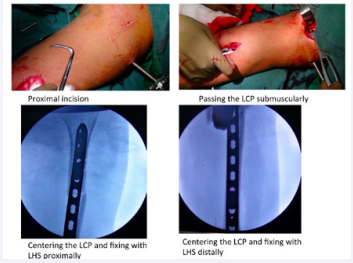
Figure 3: Passage of plate in sub muscular tunnel.
The reduction is checked under image intensifier. The elbow is flexed at 90° to relax the brachialis muscle, aiding the reduction.
Reduction being a blind procedure here, the step sign used by Krettek et al., in distal femur was used to maintain rotation and alignment [20].
In each segment a cortical screw was inserted and then the K-wires removed. A total of 3 locking head screws per fragment were inserted thus making the construct not too rigid [3,11,14,21].
Patients were started on postoperative antibiotics for a total of 3 days. Physiotherapy was started on day 3 as the pain permitted. Patients were followed up every 15 days for 2 months then monthly. During the post-operative follow-up, UCLA and MEP scores were assessed for shoulder and elbow function respectively.
Union time was determined on visualizing at least 3 cortises on anteroposterior and lateral radiographs of the humerus.
RESULTS
The study included 33 patients within the age group of 16 years to 77 years (mean 40.5 ± 16 years), of whom all were available for follow up (Figure 4).
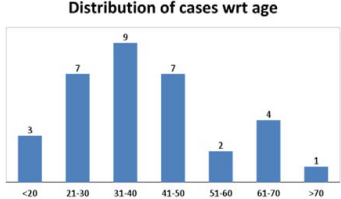
Figure 4: Age wise distribution of cases
The study has taken place from May 2014 to May 2016,
There were 24 males and 9 female patients as depicted below in Figure 5.
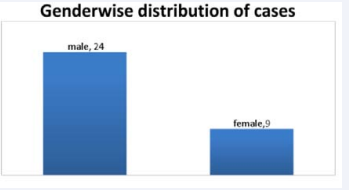
Figure 5: Sex wise distribution of cases
Out of the 33 cases, majority (90.9%) were closed fractures while the remaining 3 (9.1%) cases were open fractures.
Maximum numbers of cases were due to road traffic accidents (79%) as shown in Figure 6.
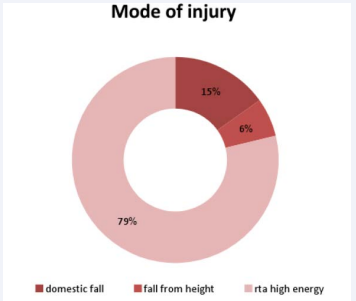
Figure 6 Mode of injury in humerus fractures (rta-road traffic accident)
This was followed by domestic fall and fall from height.
As shown in the Figure 7
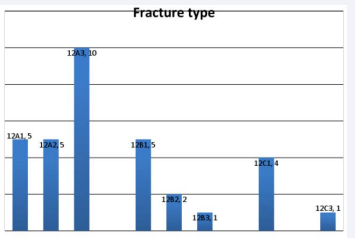
Figure 7 Case distribution according to fracture type
maximum cases fall in the 12 A3 type, followed by A1, A2 and B1. Time between admission and surgery ranged from 1 to 8 days with mean time of 3.6 ± 1.8 days and mean hospital stay lasted for 10.52 ± 5 days.
Appearance of Callus ranged from 4 weeks to 18 weeks with average at 10.94 ± 2.4 weeks, with 100% union in our series. Union time was expressed in weeks and ranged from 12 weeks to 30 weeks as shown below in Figure 8.
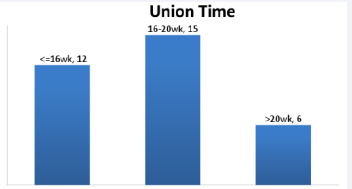
Figure 8 Union time.
It was observed that union time was less than 20 weeks for 81% (27/33) cases. Average union time was 18.3 ± 2.4 weeks.
UCLA score is graded as excellent if it is more than 27 and poor if it is less. It was observed that majority of the cases had excellent or good UCLA, with an average of 18.3 ± 4.0 shown in Figure 9.
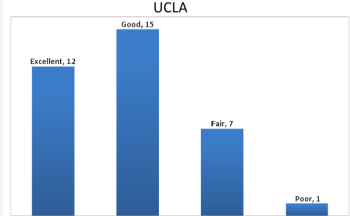
Figure 9 UCLA grading in MIPO follow-up
Only 1 case had a poor score.
MEP score is graded as excellent more than 90, good from 75- 89, fair from 60-74 and poor less than 60. 2 cases had less than excellent MEP score, while the rest had excellent score, shown in Figure 10.
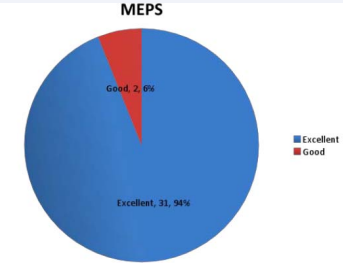
Figure 10 MEPS grading
The means of the shoulder movement is given below in Table 1.
| Table 1: range of motion of shoulder joint. | ||
|
Shoulder movement |
Range(degrees) |
Mean ± sd (degrees) |
|
abduction |
80-180 |
126.36 ± 26.55 |
|
Forward flexion |
80-180 |
110.91 ± 21.12 |
Only 8 patients had shoulder abduction less than 110 degrees shown in Figure 11.
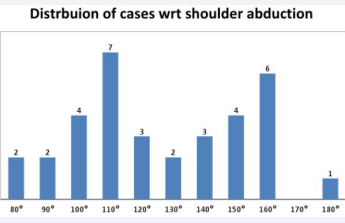
Figure 11 Shoulder abduction in MIPO
The elbow range of motion ranged from least of 100 to maximum of 140 degrees depicted in Table 2.
|
Table 2: Elbow movement in MIPO. |
||
|
elbow |
Range |
Mean ± sd |
|
flexion |
100-140 |
115.75 ± 13.46 |
|
Flexion deformity |
0-20 |
3.03 ± 5.4 |
Some cases had flexion deformity owing to the brachialis injury while fixation of the fracture. It was intermittent and recovered in a few months. The mean of flexion deformity was of 3.03°
There were17 cases which required less than 120 minutes for surgery, while 16 cases required more. Mean surgical time was 116min ± 17 min depicted in Table 3.
|
Table 3: surgical time required in MIPO. |
|
|
No. of cases |
Surgical time |
|
17 |
< 120 mins |
|
16 |
> 120 mins |
COMPLICATIONS
There were 2 cases (Case 1 and 2)
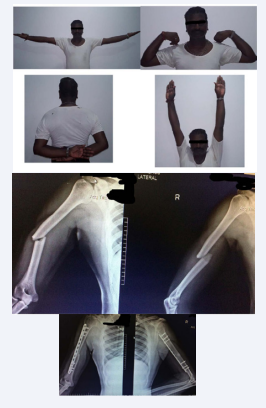
Case 1 Pre-op and Post op X-Ray with good union and full range of motion.
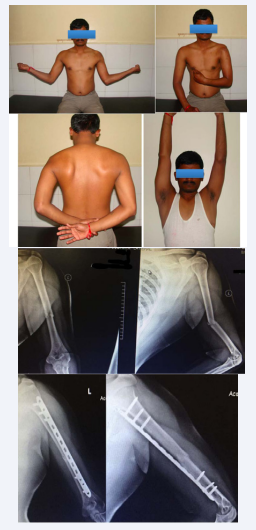
Case 2 40 year old man with MIPO technique with good range of motion
in which infection was detected. Both the cases had a compound injury. The infection was dealt with repeated debridement and antibiotic bead insertion, responding with total elimination of infection.
We had 4 cases of intraoperative radial nerve injury that recovered postoperatively. One case of intraoperative radial nerve injury occurred while placing the schanz pin, which recovered.
One patient had elbow stiffness. It resolved completely after removal of splint used for forearm injury.
Thus the complication rate was 12% (4/33). The valgus and varus angulation was calculated on the AP and lateral X--rays and shown as follows in Table 4.
|
Table 4: angulation in the follow up cases. |
||
|
angulation |
Range |
Mean ± sd |
|
anteroposterior |
0-18° |
4.94 ± 4.3° |
|
varus angulation |
0-20° |
6.09 ± 4.7° |
DISCUSSION
Humerus fractures till recent years have been treated by a number of ways ranging from bracing to Ilizarov ring fixators [2]. Currently intramedullary nailing (IMN), open reduction plate osteosynthesis (ORPO), Enders nails are most widely used. It has been observed by many studies that AO/OTA type A fractures and long oblique fractures do not respond well to nonsurgical treatment [3,22,23]. Surgery has been instituted in patients for better rehabilitation and early joint mobility [5,10,24].
In this era of minimally invasive surgery, soft tissue mportance has increased tremendously. MIPO was first developed for its use in tibia and femur [25], and was popularized for humerus by Apivatthakakul in 2005(5). It revolves around the principle proposed by Hunter and Haller that bone healing occurs in response to vascular injury around the fracture site [26].
MIPO bridge plating uses the plate as an extramedullary splint, fixing the two main fragments while the intermediate zone is left untouched. Anatomical reduction of the fracture is not necessary. Direct manipulation of the fragments risks the blood supply [27]. As the soft tissues are preserved and fragments relatively aligned, healing is predictable [11]. Humerus tolerates 10-20 degrees of sagittal plane deformity and up to 30 degree of rotational deformity.
The vascular anatomy of humerus is favorable for MIPO with respect to the constancy of nutrient artery [27-29].
According to the principles of working length, MIPO can be used for diaphyseal humerus fractures with proximal and distal extensions. This has been shown successfully by multiple publications by Apivatthakakul et al., Zhiquan An et al., Wang et al., Shetty et al., and many more [12,21,30-35].
A newer development in MIPO was devised by Lee et al., who used intraoperative external fixator to guide the fracture reduction [36]. This aided easier reduction and faster operative time. We operated 8 such cases with positive results.
Certain complications are associated with this procedure as it has a lengthy learning curve [37]. The surgical time required in our series had a mean of 116 ±17 mins.
MIPO can be successfully used in post traumatic radial nerve palsy, with gradual recovery seen post operatively [38,39]. It has been seen in 3 of our cases.
The radial nerve is closely related to the humerus. The study by Apivatthakakul describes the danger zones in screw placement in MIPO [40]. Radial nerve damage can occur in this procedure during manipulation more than during screw placement. We had 4 cases of intraoperative nerve palsy, and neuropraxia recovered soon after.
During surgery as the brachialis is handled, elbow function can be stiffened, but generally improves with physiotherapy. Mild Malunion is evident, as the fracture is reduced indirectly. In open fractures, it is mandatory to treat the wound else leading to infection, which may lead to implant failure and nonunion. In our study, there were 2 infected cases but no event of nonunion occurred.
Many studies comparing MIPO with other traditional methods Many studies comparing MIPO with other traditional methods
Studies by Baltov et al., and Ikpeme et al., enumerated that rotator cuff damage can occur with IMN, by the protrusion of the nail and collection of reamed debris underneath the cuff [48,49]. Also distraction at the fracture site can occur owing to the flattened anatomy of the distal humerus, leading to nonunion. ORPO involves stripping of the periosteum and devitalizing the tissues, leading to excessive blood loss, scarring and nonunion [41,44].
MIPO involves minimal blood loss, preservation of fracture biology and is a more cosmetic procedure. Considering the advantages and drawbacks of all procedures, MIPO emerges as a better option with regard to patient function and radiological outcome.
Table 1: range of motion of shoulder joint.
| Shoulder movement | Range(degrees) | Mean ± sd (degrees) |
| abduction | 80-180 | 126.36 ± 26.55 |
| Forward flexion | 80-180 |
Table 2: Elbow movement in MIPO.
| Elbow | Range | Mean ± sd |
| flexion | 100-140 | 115.75 ± 13.46 |
| Flexion deformity | 0-20 | 3.03 ± 5.4 |
Table 3: surgical time required in MIPO.
| No. of cases | Surgical time |
| 17 | < 120 mins |
| 16 | > 120 mins |
Table 4: angulation in the follow up cases.
| Angulation | Range | Mean ± sd |
| anteroposterior | 0-18° | 4.94 ± 4.3° |
| varus angulation | 0-20° | 6.09 ± 4.7° |
CONCLUSION
MIPO merits an overwhelming advantage compared to other conventional methods. Thus the proper selection of patients, the learning curve of the surgery, and the surgeon’s acumen play an important role in successful outcome following MIPO of shaft humerus. The hypothesis of our study is accepted.
ACKNOWLEDGMENTS
I would like to thank Dr. Prasad Pawar, our physiotherapist for rehabilitation and Mrs. Swati Raje for analyzing my data.
REFERENCES
3. Garnavos C. Humerus shaft fractures. rockwood and greens fractures in adults. 2015.
11. Pol Rommens PT. MIO approach for shaft humerus fractures.
15. Greiwe RM, Archdeacon MT. Locking plate technology: current concepts. J Knee Surg. 2007; 20: 50-55.
18. Dickson KF, Munz J. Locked Plating: Clinical Indications. Tech Orthop. 2007; 22: 181-185.
28. Laing PG. The arterial supply of the adult humerus. J Bone Joint Surg Am. 1956; 38-A: 1105-1116.








































































































































