Facilitating A Combination of Western Prevention and Indigenous Practices for Malaria Prevention among Rural Communities in Ohangwena Region, Namibia
- 1. Department of Community Health Science School of Nursing and Public Health, University of Namibia, Namibia
- 2. Department of Microbiology, School of Medicine, University of Namibia, Namibia
- 3. Department of Public Health School of Nursing and Public Health, University of Namibia, Namibia
Abstract
Background: The Ohangwena region experiences outbreaks that occur annually with varying severity. The purpose of this research paper was to explore and describe perceptions and experiences of rural communities on the western and Indigenous practices of malaria prevention in the Ohangwena region
Method: A convergent parallel mixed method was used. The qualitative, explorative, contextual phenomenological, quantitative, descriptive, analytic, and cross-sectional study design was conducted. Multistage sampling was used, including random sampling with replacement and purposive sampling. The quantitative data was electronically analyzed with the Statistical Package of Social Science and manually using Tesch’s steps for qualitative data. The tools used were a survey and an interview. The information was collected with a questionnaire from 402 respondents. The interview guide was used in qualitative data from individual interviews and focus group discussions. The actual number of interviews was determined by saturation.
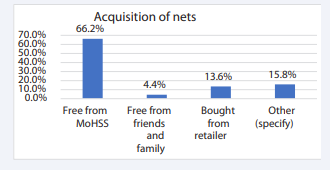
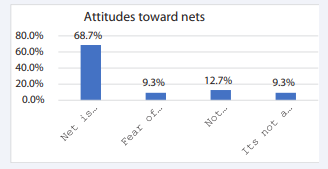
Results: Unemployment is high among the respondents, at 62.6%The finding indicated that the respondents obtained a mosquito net from free distribution, The Ministry of Health and Social Service accounts for 66.2%, followed by free donations from non-governmental organizations (NGOs) like Trans-Kunene initiatives, churches, and the Red Cross represented by 15,8 compared to 13.6% responded who bought nets for themselves. The lowest percentage, 4.4 %, received free nets from friends and family. The factors that prevent the use of the net are expensive, 68,7%, 12.7% of respondents experienced discomfort while fearing itching. and not a priority yielded 9.3%. Most of the respondents, 62,6%, are unemployed and depend on free net distribution. The findings revealed that the respondents are from low-salary occupations. prevent them from owning the net. The participants indicated that nets are not affordable and not user-friendly, as they cause discomfort, such as itching. On the other hand, problems of lack of income and unemployment make it difficult.
The three themes emerged: Dependency on free distribution of net, limited universal coverage and reduced utility of traditional preventive practices in the community, and low confidence in teaching undocumented information among health extension.
The findings confirmed that rural community depends solely on free net distribution campaigns of the MoHSS as the main source and some donor organizations.
They also narrated that there are no retail shops for net in the villages. The participants said they relied on the free net campaign, but they experienced waiting longer to receive. From the focus group discussion, participants perceive indoor residual sprays and nets as the best malaria prevention practices. However, they are not adequate for everyone. The indoor residual spray team is only applied in selected villages where confirmed positive cases are diagnosed. Despite positive diagnosis cases, some house structures are not accessible for spraying. We are not confident in indigenous practice, as they are not documented in the training manual.
Conclusion: The net free distribution creates dependency among rural communities. The inadequacy of Western interventions calls for strengthening the use of Indigenous practices in combating malaria to complement the insufficient for indoor residual sprays and long-lasting nets. It was recommended that Western intervention and Indigenous practices need equal advocacy and complement each other to achieve sustainable malaria prevention and care, maximize resources, and bridge the resource gap.
KEYWORDS
- Combination
- Western prevention
- Indigenous practices
- Malaria prevention
- Rural communities
CITATION
Uushona S, Sheehama J, Iita H (2025) Facilitating A Combination of Western Prevention and Indigenous Practices for Malaria Prevention among Rural Communities in Ohangwena Region, Namibia. J Immunol Clin Res 8(1): 1054.
INTRODUCTION
Combination of prevention practices refers to promoting the use of multiple prevention methods. The combination strategies enhance community engagement and are responsive to community needs in the fight against malaria transmission. Morbidity and mortality from malaria call for combining various preventative measures. The integration of traditional medicine and Western prevention is grounded in its effectiveness, availability, and affordability [1]. Globally, indigenous practices are culturally sustainable and accepted [2]. Resistance to insecticides and drugs is high; therefore, a booster solution that brings an impact is needed. Globally, the malaria burden is estimated at 249 million cases [3-6]. Sub-Saharan Africa has an estimated 233 million. Namibia has a burden of 13,740. The prevention of malaria disease and control of vectors calls for local relevance and responds to the context of regional needs [7]. Therefore, this paper focuses on the integration of Western interventions and indigenous prevention practices in the fight against malaria.
The purpose
The purpose of this study was to describe knowledge, attitudes, and practices as well as to explore the perceptions and experiences of rural communities on the combination of Western and Indigenous prevention practices of malaria in the Ohangwena region, Namibia
Objectives
The objectives for this study were to:
- Describe the knowledge, attitudes, and practices on Western and indigenous prevention.
- Explore the perceptions and experiences of rural communities on combining Western and Indigenous prevention practices of malaria in the Namibian context.
- Analyse the association between demographic data and knowledge, attitudes, and practices of Western and Indigenous preventive practices
METHOD
A convergent parallel mixed method was used. Quantitative and qualitative were carry equal weight. The descriptive, analytic, and cross-sectional designs were utilized for the quantitative and the following were used in the qualitative, explorative, contextual, and phenomenological. The study population was 220,683 individuals from 37,404 households. Probability and nonprobability were used with multistage sampling strategies. The nature of the study allows flexibility to involve simple random in quantitative, while in the qualitative approach, Snowball, purposive sampling found fit during the conducting of the study.
Furthermore, the sample size of 402 was determined with Yamane’s 1968 formula. In addition actual number of interviews was determined by data saturation. The 20 in- depth individual interviews, with the Head of Households, 8 focus group discussions, were conducted with Health extension workers.
The validity and reliability of the study were constituted of triangulation of methods and multiple instruments. The face and content validity assist to validate the instrument. Whereas Cronbach Alpha and the pilot study support the reliability of the study. The part of the quality improvement, the criteria of trustworthiness was constructed by maintaining credibility, through prolong engagement and collection of thick rich data. Equally important the method used helps with transferability and rigor used by supervisors and the presentation of data during peer review seminars confirms dependability. The study was open to external audit and confirmability was maintained. The research instruments were a questionnaire for a survey and an interview tool guide for interviews. The data were analysed based on the approach and design. Moreover, quantitative data were analysed with Statistical Package of Social Science, version 29, and qualitative data was analysed with ATLAS it and Tesch steps used to transcribe data.
ETHICAL CONSIDERATION
The clearance letter from the University of Namibia Research and Publication, currently known as the Decentralised Ethical Committee. Permission and approval from the Ministry of Health and Social Services, reference number 17/3/3 SU.
Informed consent was obtained both orally and written. Adherence to the principles of respect of respondents, autonomy, coded questionnaires barrier the information linked to participants, and no incentives used.
Caution was taken to adhere to beneficence and the respondents were exposed to no harm. The instrument content was the same and the respondents were accorded the same time duration to complete the tools as a demonstration of justice.
RESULTS
Results were analysed and presented separately to relate, validate, and be divergent. The findings are presented in frequency tables and figures (Tables 1-2 Figures 1-3).
Table 1: Comparison of use of Modern and traditional prevention practice per age group
|
Variables |
|
Modern practices |
Bitter bushes |
Tumble weeds |
Personal protection methods |
Other traditional Practices |
Total |
|
Age-groups |
18 |
20 |
2 |
1 |
1 |
1 |
25 |
|
|
19-24 |
60 |
2 |
1 |
0 |
0 |
63 |
|
|
25-29 |
45 |
3 |
2 |
1 |
1 |
52 |
|
|
30-34 |
37 |
0 |
1 |
2 |
0 |
40 |
|
|
35-39 |
26 |
1 |
1 |
0 |
0 |
28 |
|
|
40-44 |
31 |
0 |
0 |
0 |
1 |
32 |
|
|
45-49 |
33 |
1 |
1 |
0 |
0 |
35 |
|
|
50-54 |
18 |
0 |
2 |
0 |
2 |
22 |
|
|
55-59 |
29 |
1 |
1 |
0 |
0 |
31 |
|
|
60+ |
58 |
3 |
6 |
4 |
3 |
74 |
|
Total |
|
357 |
13 |
16 |
8 |
8 |
402 |
Table 2: Merged results and conclusion
|
Findings |
||
|
Quantitative |
Qualitative |
Conclusions |
|
value 0 .05)
prevention are influenced by many factors.
68.9%
|
was acceptable
created dependence.
under five years.
difficult in breathing, and hot,.
..
advocating for use of traditional practices
“donor funded distribution stops” |
decision making.
prevention method .
experiences and acceptance..
preventive practices..
. |
Figure 1: Sources of net acquisition (self designed).
Figure 2: Attitudes toward the usage of net.
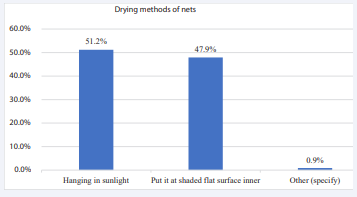
Figure 3: Drying methods of net.
Quantitative findings
Figure 1 above reflects the mechanism of how rural communities acquired nets. Of the high numbers over 80% receive nets from various sources, and only 13.6% afford to buy nets.
The respondents indicate different attitudes toward net use. The attitudes towards net use are socio-economic, with 68.2% having personal experiences of fear, and unmet needs, and being willing to prioritize net use.
The efficacy and effectiveness of the net is a challenge.
The drying method of hanging net in sunlight reduces lifespan of the insecticides and increases the worn out of the material, promoting net holes.
Table 1 revealed that Western interventions are used by many respondents when compared to traditional interventions.
Qualitative results
Based on the participants perceptions and experiences, the following themes were generated.
- Dependence.
- Limited universal coverage and reduced utility of traditional preventive practices in the community.
- Low confidence in teaching undocumented information among health extension.
Participants perceive indoor residual sprays and nets as trusted malaria prevention practices that are best. However, they are not adequate for everyone.
“Free net distribution is helps us a lot, especially, no income resulted sharing one net with my six grandchildren.” P. 6
The indoor residual spray team is only applied in selected villages where confirmed positive cases are diagnosed. “My hut was left , not sprayed, I use herbs to repel and kill mosquitoes.” P. 9.
Despite positive diagnosis cases, some house structures are not accessed for spray.
We are not confident in indigenous practices, they are not documented in the training manual.
“I find it difficult to talk of indigenous methods, no validation of efficacy and not documented in our training manuals.” P7 FGD.
Merging of results and conclusions
DISCUSSIONS
There is good knowledge for the utilization of Western and traditional prevention methods. The nets are free but not adequate for all. Similarly the findings indicates that Western interventions are not affordable,not accessible, they are distant from rural communities and have technical challeges [1]. These findings are in line with the study done in Ethiopia [8] and other part of the world [9]. The use of animal dung and plant materials burnt to deter mosquitos is in agreement with the study done in Zimbabwe [10].
Cost increases the gap in utility and access, similar to the studies from various authors [8,9,11]. The poverty reduction as stated in the sustainable goals document is still a theory. The results speak to the study done on universal coverage as a challenge in rural communities [12].
The multiple strategies have the potential to bring solutions considering that health is influenced by many determinant factors. However, the current malaria interventions of malaria prevention are Western prevention-dominated [13]. This finding is in line with the study of Greenwood [13]. The increased resistance to drugs and insecticides is inevitable [3]. The calls for additional methods that are responsive to sustainable development goals to meet the local needs of the served communities are observed in the Ohangwena region. The findings is in agreement with sub-Saharan Africa, [14], and with the study done else in the world [15].
The undocumented indigenous information makes it difficult for Health extension workers to impart oral information. Evidence of oral information is practice many part of the world is in agreement with the study done else in the world [14,15].The challenge of undocumented indigenous information makes it difficult for Health extension workers to impart oral information. Evidence of oral information is practiced many part of the world [14,16].
Recommendations
The use of Indigenous practices should use concurrently with Western prevention in areas where it is not feasible for targeted priorities.
It was recommended that Western intervention and Indigenous practices need equal advocacy.
Complement each other to achieve sustainable malaria prevention and care, maximize resources, and bridge the resource gap.
The net free distribution creates dependency among rural communities despite the lack of strengthening the use of Indigenous practices in complementing insufficient Western interventions. It was recommended that Western intervention and Indigenous practices need equal advocacy and complement each other to achieve sustainable malaria prevention and care, maximize resources, and bridge the resource gap as stipulated in the Sustainable Development Goal approach.
Limitations of the study
The information provided is only for the selected region, Ohangwena, in Namibia. There was no experiment conducted, so the data was generated from the responses of the participants/respondents.
CONCLUSION
There is a need to adopt non-resistance Western and traditional practices in malaria control. Create awareness of the risk of malaria aligned with strengthening basic local available practices, establish initiatives and collaboration, and improve the malaria program with adequate funds. Learn from the best practices of countries that successfully achieve elimination.
ACKNOWLEDGEMENT
We acknowledge the University of Namibia for permission for this study and the Ministry of Health and Social Services for Approval to conduct the study and provide as chance to participate in collaborative call for malaria emergence within the Ohangwena Region Health Directorate. Thank you for the Namibian Nursing Association funding the conference logistics. We are grateful ECSACONM, by invitation and acceptance of the paper. TESA Project III and EDCTP, your valuable contribution is immersed for capacity building. Many thanks and we are very much grateful for all study participants for their contributions.
REFERENCES
- Million E, Mulugeta T. Traditional Medicine Practice and Its Role in the Management of Malaria in Jimma Town , Oromia, Dovepress Infect Drug Resist. 2022; 15: 2187-2198.
- Olango TM, Tesfaye B, Catellani M, Pè ME. Indigenous knowledge, use and on-farm management of enset (Ensete ventricosum (Welw.) Cheesman) diversity in Wolaita, Southern Ethiopia. J Ethnobiol Ethnomed. 2014; 10.
- Tizifa TA, Kabaghe AN, Mccann RS, Berg H Van Den, Vugt M Van, Phiri KS. Prevention Efforts for Malaria. Curr Trop Med Reports. 2018; 5: 41-50.
- WHO. Report 20-23.
- Organization WH. World malaria World malaria report report. Geneva: World Health Organization; 2023; 1-356 p.
- Leal Filho W, May J, May M, Nagy GJ. Climate change and malaria: some recent trends of malaria incidence rates and average annual temperature in selected sub-Saharan African countries from 2000 to 2018. Malar J [Internet]. 2023; 22: 1-14.
- Gachelin G, Garner P, Ferroni E, Verhave JP, Opinel A. Evidence and strategies for malaria prevention and control : a historical analysis. Malar J [Internet]. 2018; 17: 1-18.
- Ea O, Napier M, Garner P. Housing interventions for preventing malaria ( Protocol ). 2019; 2019: CD013398.
- Sitepu R, Marsaulina I, Ashar T. Community-based malaria prevention policy model in Rampah Village , Kutambaru District , Langkat Regency , Indonesia. J Infrastructure, Policy Dev. 2024; 8: 1-19.
- Makuvara Z, Magano SR, Mugumbate G. Malaria control and treatment : the role of indigenous practices in Zimbabwe. Cogent Public Heal [Internet]. 2024; 11: 1-16.
- Ahorlu CS, Adongo P, Koenker H, Zigirumugabe S, Bright SS, Koka E, et al. Understanding the gap between access and use : a qualitative study on barriers and facilitators to insecticide - treated net use in Ghana. Malar J [Internet]. 2019; 18: 1-13.
- Taek MM, Ew BP, Agil M. The Prevention and Treatment of Malaria in Traditional Medicine of Tetun Ethnic People in West Timor Indonesia. J Complement Altern Med. 2019; 1: 76-84.
- Greenwood B, Cairns M, Chaponda M, Chico RM, Dicko A, Ouedraogo JB, et al. Combining malaria vaccination with chemoprevention : a promising new approach to malaria control. Malar J [Internet]. 2021; 20: 1-7.
- Suleman S, Beyene Tufa T, Kebebe D, Belew S, Mekonnen Y, Gashe F, et al. Treatment of malaria and related symptoms using traditional herbal medicine in Ethiopia. J Ethnopharmacol. 2018; 213: 262-279.
- Deressa A, Gamachu M, Birhanu A, Ayana GM. Malaria Risk Perception and Preventive Behaviors Among Elementary School Students , Southwest Malaria Risk Perception and Preventive Behaviors Among Elementary School Students , Southwest Ethiopia . Generalized Structural Equation Model. Infetion Drug Resist. 2023; 1-15.
- Mekonnen LB. Journal of Traditional and Complementary Medicine In vivo antimalarial activity of the crude root and fruit extracts of Croton macrostachyus ( Euphorbiaceae ) against Plasmodium berghei in mice. J Tradit Chinese Med Sci [Internet]. 2015; 5: 168-73.