Gas Forming Pyogenic Liver Abscess around a Primary Hepatic Biliary Calculus
- 1. Medico Surgical Clinic and Hospital, India
Abstract
A report of a case of gas forming pyogenic liver abscess associated with a primary hepatic calculus. 51 year old diabetic patient on insulin underwent laparoscopic cholecystectomy for symptomatic cholelithiasis. Patient had uneventful postoperative course. She presented after three weeks with pain in right hypochondrium, fever and clinical and laboratory features of septicemia. Ultrasound and CT scan showed abscess in segment V and VI with gas within, normal IHBR and no calculi. Patient was treated with broad spectrum antibiotics and surgical drainage through right subcostal incision; a 1 cm calculus was found in the abscess cavity. Pus culture showed growth of E. coli. Though there are sporadic reports of gas forming hepatic abscess most are secondary to interventions like radiofrequency ablation, intra arterial embolisation or intra arterial infusion chemotherapy. But there is no report of gas forming abscess without such intervention. Gas forming hepatic abscess are associated with high morbidity and mortality. The present case was associated with primary hepatic calculus and recovered completely with surgical drainage and antibiotic therapy along with good blood glucose control.
Keywords
Liver abscess; Pyogenic liver abscess; Types and causes of liver abscess.
CITATION
Mehendale VG, Chaudhari N (2016) Gas Forming Pyogenic Liver Abscess around a Primary Hepatic Biliary Calculus. J Liver Clin Res 3(1): 1025.
ABBREVIATIONS
HCC: Hepato Cellular Carcinoma
INTRODUCTION
primary hepatic biliary calculus within such an abscess. We report a case of a 51 year old diabetic woman who developed a pyogenic abscess around a primary hepatic biliary calculus 3 weeks after she underwent laparoscopic cholecystectomy. The abscess was cured by open drainage
CASE PRESENTATION
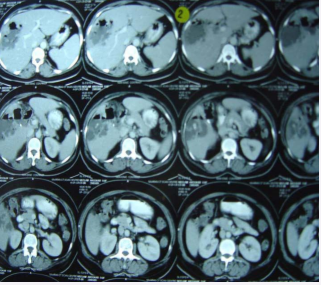
A 51 year old diabetic woman with symptomatic cholelithiasis was treated by laparoscopic cholecystectomy. Her pre operative abdominal ultrasonograhy showed multiple gall bladder calculi, common bile duct (CBD) size was 3mm, intrahepatic biliary radicles were normal. She required 28 units of human insulin per day for the control of blood sugar levels. Liver function tests were within normal limits. During laparoscopic cholecystectomy there was no spillage of bile or calculi into the peritoneal cavity. Three weeks after cholecystectomy the patient suffered from pain in the right hypochondrium and fever. She had stopped insulin therapy on her own after discharge from the hospital. She was hospitalized in septicemia. Her hemoglobin had come down to 8gm/dl, leucocyte count was 26000/mm3, serum bilirubin was 0.9mg/dl with direct bil. 0.4mg/dl and blood glucose level was 360mg/dl. She was treated with ceftizidime, gentamycin and metronidazole. Ultrasonography showed abscess in the right lobe of liver with air fluid level, post cholecystectomy status, no evidence of calculi. CT scan showed a large abscess in segment V and VI with gas within, normal intrahepatic biliary radicals and no evidence of calculi (Figure 1a).
Figure 1a C T scan showing gas filled abscess cavity in hepatic segments V and VI.
Patient was operated upon by right subcostal incision (Kocher’s). There was a large abscess in the lateralmost part of the right lobe of liver, pointing on the lateral surface. Incision was taken on this point and about 250ml of thick pus was drained. A 1cm diameter calculus came out along with pus (Figure 1b) .
Figure 1b Calculus found in the abscess cavity.
The abscess was in the segment V and VI of the liver and there was no communication with the gall bladder fossa. The gall bladder fossa was normal and the clips on cystic duct and the cystic artery were in place. Pus was sent for culture. 32 FG size drain was placed in the abscess cavity. There was luxuriant growth of E coli in the culture, sensitive to ceftizidime and amikacin. Drain was removed on the 4th post operative day and patient discharged on the 7th post operative day. Patient has been followed up for 3years and is symptom free.
DISCUSSION
There have been sporadic reports of gas forming liver abscesses in the literature [1-6]. But Chou et al in their retrospective study reported 36% incidence of gas forming abscesses amongst their study of 424 cases of hepatic abscesses [7]. In most of the reports the gas forming abscesses occurred following interventions like intra arterial infusion chemotherapy for hepatocellular carcinoma (HCC); intra arterial chemoembolisation, radiofrequency ablation or intra arterial embolisation for benign conditions like pseudoaneurysm [1,2,46]. In majority of the cases underlying cause for formation of gas forming abcesses is not found. But 57.5% of the cases in series were diabetic. In the remaining cases there were predisposing factors like hepatocellular carcinoma, cholecysto or choledocho lithiasis, biliary tract cancer [8]. Klebsiella pneumoniae has been commonest organism grown from these abscesses [7,8]. Out of 15 cases with Salmonella typhoid infection only one was associated with HCC [3]. Clostridium septicum was grown in only one patient of choriocarcinoma with hepatic metastasis [9].
Patients have been treated with medical treatment (antibiotics), aspiration, percutaneous drainage or operative drainage of the abscesses. Mortality is much higher in patients treated by medical treatment or aspiration only (44.4%) as compared to operative treatment [7]. The overall mortality in gas forming liver abscesses is much higher than in non gas forming liver abscesses[7,10].
In the present case the patient’s laparoscopic cholecytectomy was uneventful. There was no bile or stone spillage during surgery. Patient discontinued prescribed insulin therapy and developed septicaemia with gas forming abscess in the liver. Her preoperative and postoperative ultrasonography and CT scan did not reveal any evidence of primary hepatic biliary calculus. Operative drainage of the liver abscess revealed a centimeter size primary hepatic calculus in the abscess cavity occupying segment V and VI of the liver. The cavity did not communicate with the gall bladder fossa. Our patient suffered from diabetes mellitus which is a well known underlying condition in cryptogenic gas forming pyogenic liver abscess. But finding of a primary hepatic biliary calculus was a surprise. There was no other predisposing cause for gas forming liver abscess. E.coli were cultured from pus. This organism has been reported by others but not as commonly as klebsiella [6,7,10]. Early surgical drainage, appropriate antibiotic therapy, and control of diabetes mellituts and septicaemia saved our patient despite high morbidity and mortality associated with gas forming liver abscesses[7,10].