Incomplete Strasberg E Injuries: A Roux-En-Y Jejunal Patch As An Alternative Surgical Treatment
- 1. Department of General Surgery, National Institute of Medical Sciences and Nutrition “Salvador Zubirán,” Mexico
Abstract
The aim of this work is to describe our experience with an alternate surgical technique utilized in incomplete Strasberg E bile duct injuries, refractory to percutaneous and endoscopic dilation. These incomplete bile duct injuries have partial patency and no loss of continuity; and, should be considered as complex lesions in most cases. Stepup approach should be regarded. The surgical technique used by our institution will be portrayed and its corresponding outcomes in our patients will be discussed.
Keywords
Bile duct injury; Biliary repair; Hepatojejunostomy; Incomplete Strasberg E injuries.
CITATION
Mercado MÁ, Domínguez I, del Valle DD, Hernández-Acevedo JD, Muñoz-González HR, et al. (2017) Incomplete Strasberg E Injuries: A RouxEn-Y Jejunal Patch As An Alternative Surgical Treatment. J Liver Clin Res 4(1): 1030.
INTRODUCTION
Surgical repair is the standard treatment for iatrogenic bile duct injuries when loss of continuity occurs. These complex lesions requiere a hepatojejunal anastomosis due to the presence of microvascular damage and the loss of confluence previously mentioned [1]. In some instances, a partial occlusion of the bile duct is detected. This might be a consequence of a focal injury generated by thermal damage and/or misplacement of surgical clips with concomitant ischemic damage of the duct. These injuries can be classified as Strasberg E and its subsets [2], however, there is partial patency of the bile duct and no loss of continuity. Endoscopic or radiological management of stenosis can be attempted with the goal of dilating it, with high probability of recurrence. When a surgical clip causes partial obstruction, it becomes very difficult to dilate, either endoscopically of radiologically.
Our group has treated most of these cases with a Roux-en-Y hepatojejunostomy, in concordance with an E injury (although restricted patency of the duct is observed). We have developed another surgical technique option for treatment of these lesions.
Technique
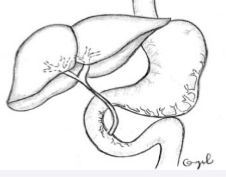
Dissection of the hilus is done. The duct is identified easily as there are only adhesions secondary to the cholecystectomy (Figure 1).
Figure 1 Longitudinal extrahepatic bile duct stenosis.
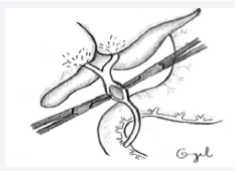
Careful dissection is performed to identify the site of structure with no dissection of the lateral aspect of the duct, in order to avoid devascularization. Anterior vertical opening is done with a fine knife, including the focal structure (Figure 2).
Figure 2 Longitudinal strictureplasty of the bile duct’s anterior aspect.
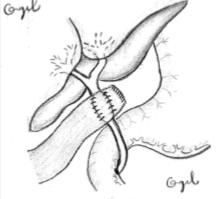
Bile duct dilators are inserted above and below the structure to find and remove residual stones. Instead of a hepatojejunal anastomosis or T-tube insertion, a Roux-en-Y jejunal patch is performed. A side-to-side anastomosis of the duct utilizing separated, everted knots of (5-0) absorbable monofilament is done, as wide as possible, but no more than a half inch (Figure 3).
Figure 3 Biliary duct plasty with mucosae patch.
The main objective is to replace the stenotic tissue with jejunal mucosae.
CASE REPORTS
During a 25-year period, nine cases have been treated in our center with this side-to-side technique with a mean follow-up of six years. None of them have developed cholangitis, cirrhosis or portal hypertension.
One case possessed a Morton neuroma, three had an incomplete obstruction of a clip, and five of them presented postoperative fibrosis of the duct. In one case, a control ERCP was done, reporting adequate passage of the injected contrast to the jejunal limb.
Table 1 describes further clinical data of the case series.
|
Table 1: Demographics and clinical data of 9 cases that underwent a jejunal patch. |
||||||
|
Case |
Age |
Time after cholecystectomy (months) |
Diagnosis ERCP/RMN |
Jaundice/or cholangitis |
Post op Months |
Post op ERCP |
|
1 |
30 |
<12 |
ERCP |
+ |
60 |
- |
|
2 |
39 |
<12 |
RMN |
+ |
60 |
- |
|
3 |
42 |
6 |
ERCP |
+ |
48 |
- |
|
4 |
44 |
4 |
ERCP |
+ |
48 |
- |
|
5 |
40 |
6 |
ERCP |
+ |
48 |
- |
|
6 |
35 |
8 |
RMN |
+ |
48 |
- |
|
7 |
64 |
12 |
ERCP |
+ |
48 |
+ (stone removal) placement of endoprothesis |
|
8 |
57 |
1 |
ERCP |
+ |
24 |
- |
|
9 |
20 |
1 |
RMN |
+ |
6 |
- |
REFERENCES
DISCUSSION
Surgical repair is commonly performed for bile duct injuries with loss of continuty [3]. Devascularization of the duct and loss of substance is the mainstay finding. This is the main reason to discourage an end-to-end anastomosis of the duct. In this situation, a tension-free, non-ischemic anastomosis is difficult to achieve. This is the opposite scenario of a duct-to-duct anastomosis in liver transplantation, where two well-preserved, non-ischemic ducts are anastomosed. Nevertheless, this anastomosis is not exempt from structure.
Even though the duodenum has been advocated as a favorable option to create the anastomosis because of its anatomical location, [4] it remains questionable since it is a fixed limb, generating tension of the anastomosis and gastric contents may cause a sump syndrome with recurrent cholangitis. Hepatoduodenal anastomosis is an adequate choice for unresectable pancreatic cancer with biliary obstruction, in which a dilated duct is found; and, unfortunately long-term survival is not expected. In nonmalignant biliary obstruction, hepatojejunostomy is the surgical treatment of choice that allows a patent, wide, tension-free, non-ischemic anastomosis [5]. Partial occlusion of the duct is a multifactorial condition. In some instances, this occlusion is consequence of ischemic damage of the duct with a secondary scar; other times, it results from thermal injury. Development of a Morton neuroma and clip misplacement have also been described as causes. These injuries can be treated initially by means of endoscopic dilation and/or placement of endoscopic stents. This step-up approach is not always successful, with the disadvantage of stone formation and recurrent colangitis [6]. These injuries can be classified as Strasberg D or E. Type D injuries are lateral injuries that can be treated by lowering the bile duct, preserving it by using sphincterostomy and/or stent. The final outcome might be unpredictable and related to the size, location and ischemic status of the duct. Partial occlusion of the duct, should be considered as a complex injury (circumferential) in most cases. If only a small structure of the lumen is observed, multidisciplinary step-up approach of the injury is recommended. If a significant structure of the lumen is detected (perhaps 30%), a surgical procedure should be considered as initial treatment. Despite that the hepatojejunostomy has been our preferred choice, a side-toside hepatojejunostomy, made exactly at the level of the structure is another technical option, instead of closing the structure over a T-tube. This approach has several advantages: The stenosis is resolved “de facto” and continuity of the duct is mantained, which would allow an endoscopic approach posteriorly, in case necessary. Although, this has not been the case in our patients. This type of repair is, by far, the easiest option that can be done. Our series (although small) represents almost 1% of the total cases we have treated and has shown adequate long-term results. These cases had been excluded from our previous publications in view of controversy at the time of classification. We did not classified them as postoperative injuries with complete loss of continuity since they presented a preserved and patent duct. Now that our experience has grown and our institution is considered a national reference center for repair, we propose this approach as an alternative surgical choice.