Liver Histology According to Differing Alanine Aminotransferase Level in Immune Tolerance Phase Patients with Chronic Hepatitis B Virus Infection
- 1. Liver Disease Diagnosis and Treatment Center of Chinese PLA, the 88th Hospital of Chinese PLA, China
Abstract
Background: Normal alanine aminotransferase (ALT) levels do not necessarily imply normal liver pathology. We aimed to observe differencesin liver inflammation during the immune tolerance phase of chronic hepatitis B virus (HBV) infection according to two upper limits of normal (ULN) ALT standards (30 U/L and 19 U/L for males and females, respectively, vs. 40 U/L).
Methods: Two hundred and two patients were divided into low (≤30 U/L and ≤19 U/L for males and females, respectively) and high (31–40 U/L and 20–40 U/L for males and females, respectively) ALT groups. The Ishak and Metavir systems were used to evaluate liver inflammation and fibrosis, respectively.
Results: Apositive correlation was observed between ALT levels and both Ishak and Metavir fibrosis staging scores. The proportion of mild inflammation was 97.9% and 65.7% in the low and high ALT groups, respectively. Meta vir fibrosis staging in all low ALT patients was F0 and F1. However, in the high ALT group, the proportion of F0, F1, F2, and F3 was 51.4%, 39.0%, 7.6%, and 1.9%, respectively. Age and sex had a significant impact on the distribution of Meta Vir mild, moderate, and severe fibrosis staging, but HBV DNA levels did not.
Conclusions: For immune tolerance phase HBV patients, the lower ALT ULN suggested herein is better than the currently used ULN in evaluating liver histology. Furthermore, sex and age are associated with the degree of liver histology observed in low ALT-level patients.
Keywords
Liver histology; Persistently normal ALT; Chronic HBV infection; Immune tolerance phase; Upper limits of normal for ALT.
CITATION
He D, Shang Q, Zhang Y, An Y, Yi Q, et al. (2015) Liver Histology According to Differing Alanine Aminotransferase Level in Immune Tolerance Phase Patients with Chronic Hepatitis B Virus Infection. J Liver Clin Res 2(1): 1007.
ABBREVIATIONS
HBV, hepatitis B virus; HBeAg, hepatitis B e antigen; ALT, alanine aminotransferase; ULN, upper limit of normal.
INTRODUCTION
The initial phase of chronic hepatitis B virus (HBV) infection, also known as the immune tolerance phase, is characterized by positivity for hepatitis B e antigen(HBeAg), very high HBV DNA (>10? IU/mL) and normal alanine aminotransferase (ALT) concentrations.Minimum inflammation and fibrosis are observed by histology and this phase can last for 20–40 years with very little disease progression [1]. Evidently, normal ALT concentrations do not necessarily mean normal liver histology [2-4], and some patients who develop to end-stage liver disease have no history of active hepatitis or elevated ALT levels. In general, antiviral treatment for immune tolerance phase patients is not recommended without histological evidence of liver inflammation [5]. However, liver biopsy is the most common standard by which obvious histological inflammation is identified prior to antiviral treatment [6]. Therefore, it is necessary to evaluate the actual histological activity and choose the most suitable time for giving appropriate treatment.
As the gold standard to evaluate the degree of liver damage, liver biopsy is most useful in patients who do not meet clear-cut guidelines for antiviral treatment, especially for patients in the immune tolerance phase and when there is a lack of data to assess the severity of the disease [7]. Though providing potentially useful information to assess prognosis and guide treatment, liver biopsy is invasive for patients. Therefore, it is important to evaluate histological activity by non-invasive methods to complement or avoid a liver biopsy, including routine examination and analysis of related factors. A studyhas suggested that the upper limits of normal (ULN) for ALT should be decreased to 30 U/L for males and 19 U/L for females [8]. However, the current laboratory standard of ULN remains 40 U/L, regardless of sex. The difference between the two standards of ULN in evaluating the liver histological activity requires further investigation.
The aim of this study was to observe differencesin liver histology between the two ULN standardsin chronic HBV infection carriers in the immune tolerance phase, and to explore the association between liver histological inflammation and related factors (i.e., age, sex, and HBV DNA levels).
PATIENTS AND METHODS
Patients and groups
This retrospective study included a sample of 202 chronic HBV infection carriers with immune tolerance undergoing liver biopsy in the period between January 2006 and January 2011. The demographic and clinical characteristics of the study population are shown in (Table 1).
Table 1: Demographic and clinical characteristics of the study patients.
#: <31 U/L for males, <20 U/L for females; *: 31–40 U/L in males, 20–40 U/L in females.
|
Characteristics |
Low ALT group # |
High ALT group* |
P value |
|
No. |
97 |
105 |
|
|
Male - no. (%) |
65 (67.0) |
71 (67.6) |
0.927 |
|
Age - years |
32.6 ± 8.1 |
34.9 ± 8.5 |
0.052 |
|
20-29 - no. (%) |
39 (40.2) |
29 (27.6) |
0.127 |
|
30-39 - no. (%) |
32 (33.0) |
37 (35.2) |
|
|
40-49 - no. (%) |
26 (26.8) |
39 (37.1) |
|
|
HBV DNA - log10 IU/Ml |
7.52 ± 0.30 |
7.48 ± 0.33 |
0.374 |
|
ALT - U/L |
18.8 ± 5.2 |
34.7 ± 3.9 |
1.35 × 10-58 |
|
Male - U/L |
21.3 ± 4.1 |
35.9 ± 2.6 |
1.41 × 10-45 |
|
Female - U/L |
13.7 ± 3.0 |
32.3 ± 4.8 |
9.16 × 10-26 |
Patients were divided into low and high ALT groups according to the mean of at least 2-year follow-up. According to the suggested ULN for ALT (30 U/L for males and 19 U/L for females) [8] and the currently used ULN (40 U/L),the high ALT level was assigned as31–40 U/L in males and 20–40 U/L in females, while the low ALT level was designated as ≤30 U/L in males and ≤19 U/L in females.
Inclusion and exclusion criteria
The criteria of diagnosis followed the European Association For The Study Of The Liver (EASL) guidelines [5]. Inclusion criteria were as follows: (a) a history of 2-year follow-up by monitoring at 3-month intervals; (b) persistentlyHBsAg positive, HBeAg positive, HBeAb negative, HBV DNA >1×107 IU/mL; (c) persistently normal ALT according to the current laboratory standard of ULN (40 U/L).
Exclusion criteria were: (a) clinical and/or biochemical signs of chronic active hepatitis and cirrhosis (spider angiomas, liver palm, or decreased serum albumin, etc.); (b) liver disease that was not due to hepatitis B, co-infection with hepatitis C virus, hepatitis D virus or human immunodeficiency virus, autoimmune diseases, or alcohol intake; (c) radiographic evidence of hepatic cell carcinoma, fatty liver, hepatic hemangioma, splenomegaly, or portal hypertension, etc.; (d) a history of antiviral treatment.
Serological assays
Routine biochemical tests were performed using automated techniques (Hitachi 7020, Japan). HBV markers were detected by electro chemiluminescence (Architect, Abbott Laboratories, Abbott Park, IL, USA). Serum HBV DNA was quantified with a commercially available polymerase chain reaction assay (LightCycler®480 Real-Time PCR System, Roche, and Basel, Switzerland).
Liver biopsy and histology
Liver biopsy was performed uniformly by skilled operators under ultrasound guidance. Liver samples were obtained by percutaneous needle biopsy, using a cutting needle (BardMagnum 16G, BARD, Murray Hill, NJ, USA). Biopsy samples were collected separately and coded without indications of biochemical and virologic results. They were processed according to standard histologic procedures. Liver tissue was fixed in 10% formalin and paraffin-embedded sections were stained by hematoxylineosin and Masson’s trichrome. The biopsies were evaluated by two experienced liver pathologists together to improve the reproducibility of the scoring. The histology was scored by an average of both pathologists’ evaluations. All liver specimens had at least 10 portal areas and were not fragmented enough to preclude recognition of acinar architecture. Liver histology wasscored according to the Ishak and Metavirscoring systems [9].
Statistical analysis
Continuous variables were expressed as mean ± SD for normal distribution or median (P25-P75) for abnormal distribution. The Pearson chi-square test, Kruskal-Wallis test, ANOVA, and Spearman’s (ρ) correlation were carried out as appropriate. All tests for significance and resulting p values were two-sided, with a level of significance of 0.05. The statistical software used for this analysis was SPSS 18.0.
Ethics
Written informed consent was obtained from each patient participating in the study. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the ethics committee of the 88th Hospital of the People’s Liberation Army.
RESULTS AND DISCUSSION
Ishak inflammation grading score of patients
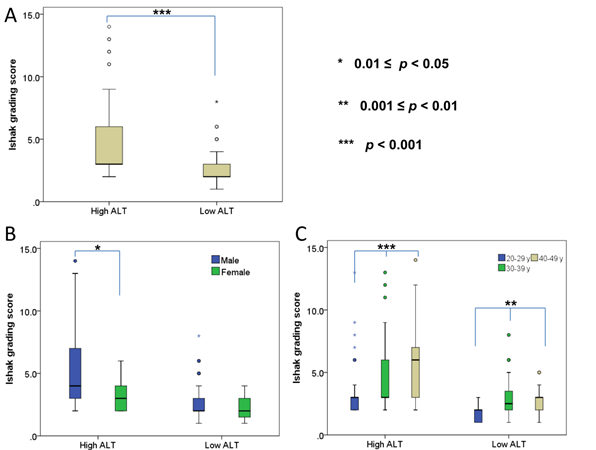
The median Ishakscore for patients was 3.0 (2.0–4.0). A significant difference was seen between the low and high ALT groups (p=1.55×10-11; Figure 1A). Significant differences between males and females were only seen in the high ALT group (p=0.011; Figure 1B). However, significant differences among age groups were seen in both the low ALT group (p=0.003; 20–29y vs. 40–49y, p=7.46×10-4; 20–29y vs. 30–39y, p=0.018; 30–39y vs. 40–49y, p=0.567) and high ALT group (p=9.36×10-4; 20–29y vs. 40–49y, p=2.06×10-4; 20–29y vs. 30–39y, p=0.044; 30–39y vs. 40–49y, p=0.066;( Figure 1C).
Figure 1 Ishak grading score in patients. (A) Comparison between low and high ALT groups (p=1.55×10-11). (B) Comparison between male and female in low ALT (p=0.209) or high ALT groups (p=0.011). (C) Comparison among age groups in low ALT (p=0.003) or high ALT groups (p=9.36×10- 4 ).
A positive correlation was seen between Ishak inflammation score and ALT levels (ρ=0.421, p=4.38×10-10), and age (ρ=0.407, p=1.87×10-9), but not HBV DNA levels (ρ=-0.068, p=0.337). In the low ALT group, no significant correlation was observed between Ishak inflammation score and ALT levels (ρ=0.097, p=0.345). However, a positive correlation was seen between age and Ishak inflammation score (ρ=0.285, p=0.005), but a negative correlation was evident between HBV DNA levels and Ishak inflammation score (ρ=-0.298, p=0.003). In the high ALT group, positive correlations were only seen between age and Ishak inflammation score (ρ=0.451, p=1.35×10-6). No significant correlation was seen between ALT levels (ρ=0.017, p=0.862) or HBV DNA levels (ρ=0.140, p=0.155) and Ishak inflammation score.
Ishak fibrosis staging score of patients
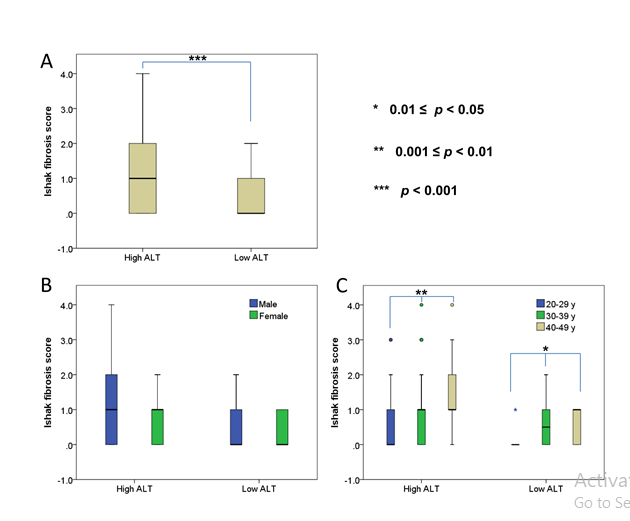
The median fibrosis staging of patients was 1.0 (0–1.0), with a significant difference observed between the low and high ALT groups (p=6.15×10-5; Figure 2A). However, no significant differences between males and females were seen in either the high (p=0.547) or low ALT groups (p=0.315; Figure 2B). Significant differences among age groups were seen in both the low ALT (p=0.010; 20–29y vs. 40–49y, p=0.005; 20–29y vs. 30– 39y, p=0.016; 30–39y vs. 40–49y, p=0.661) and high ALT groups (p=0.001; 20–29y vs. 40–49y, p=3.37×10-4; 20–29y vs. 30–39y, p=0.064; 30–39y vs. 40–49y, p=0.042; Figure 2C).
Figure 2 Ishak fibrosis staging score in patients. (A) Comparison between low and high ALT groups (p=6.15×10-5). (B) Comparison between male and female in low ALT (p=0.315) or high ALT groups (p=0.547). (C) Comparison among age groups in low ALT (p=0.010) or high ALT groups (p=0.001).
Positive correlation was also seen between Ishak fibrosis staging score and ALT levels (ρ=0.223, p=0.001), and age (ρ=0.384, p=1.73×10-8), but not HBV DNA levels (ρ=-0.045, p=0.522). In the low ALT group, a positive correlation was seen between Ishak fibrosis score and age (ρ=0.252, p=0.013), but no significant correlation was observed betweenIshak fibrosis staging score andALT levels (ρ=0.056, p=0.589), or HBV DNA levels (ρ=-0.182, p=0.074). Similarly, in the high ALT group, a positive correlation was only seen between age and Ishak fibrosis staging score (ρ=0.437, p=3.12×10-6), with no significant correlation observable forALT levels (ρ=-0.069, p=0.485), or HBV DNA levels (ρ=0.066, p=0.503).
Metavir grading of patients
The aim of liver biopsy in immune tolerance phase patients is to determine treatment strategy. However, the Ishak score system seems too complex. Therefore, we evaluated the histological inflammation of patients based on the Metavir grading algorithm. The proportion of mild, moderate and severe inflammation was 81.2% (164/202), 15.3% (31/202), and 3.5% (7/202), respectively. In the low ALT group, the proportion of mildinflammation was 97.9% (95/97), with no severe casesidentified in this group. However, in the high ALT group, the proportion of mild, moderate and severe inflammation was 65.7% (69/105), 27.6% (29/105), and 6.7% (7/105), respectively.
As cumulatively, 94.7% (36/38) of patientswith moderate orsevere histological activity was seen in the high ALT groupand 34.3% (36/105) of high ALT group demonstrated moderate orsevere inflammation, we focused on this group to analyze the correlation between Metavir grading and associated factors. A significant difference was observed for age, with the mean age of mild, moderate, and severe inflammatory activity being 32.7 ± 8.1 years, 38.5 ± 7.9 years, and 41.1 ± 6.8 years, respectively (p=7.74×10-4). However, no significant difference was seen for sex or HBV DNA level (Table 2).
Table 2: Comparison of the proportion of mild, moderate and severe Metavir inflammation activity in high ALT group according to age and sex.
|
Category |
Mild |
Moderate |
Severe |
p value |
|
Sex |
|
|
|
|
|
Male - no. (%) |
42 (59.2) |
22 (31.0) |
7 (9.9) |
0.058 |
|
Female - no. (%) |
27 (79.4) |
7 (20.6) |
0 (0) |
|
|
Age (years) |
|
|
|
|
|
20-29 - no. (%) |
24 (82.8) |
4 (13.8) |
1 (3.4) |
0.031 |
|
30-39 - no. (%) |
25 (67.6) |
9 (24.3) |
3 (8.1) |
|
|
40-49 - no. (%) |
18 (46.2) |
18 (46.2) |
3 (7.7) |
|
HBV DNA levels in patients demonstrating mild, moderate and severe inflammation was 7.44 ± 0.33 log10 IU/mL, 7.59 ± 0.32 log10 IU/mL, and 7.50 ± 0.39 log10 IU/mL, respectively (p=0.144).
Metavir fibrosis staging of patients
The proportion of patients showing stages F0, F1, F2 and F3 was 66.3% (134/202), 28.7% (58/202), 4.0% (8/202), and 1.0% (2/202), respectively. No patients were found to demonstrate stage F4. In the low ALT group, the proportion of F0 and F1 was 82.5% (80/97) and 17.5% (17/97), while in the high ALT group, the proportion of F0, F1, F2, and F3 was 51.4% (54/105), 39.0% (41/105), 7.6% (8/105), and 1.9% (2/105), respectively (p=1.79×10-5).
We further focused on the high ALT group to analyze the correlation between Meta vir fibrosis staging and associated factors. A significant difference was seen in sex and age (Table 3),
Table 3: Comparison of the proportion of F0, F1, F2, and F3 Metavir fibrosis staging in high ALT group according to age and sex.
|
Category |
F0 |
F1 |
F2 |
F3 |
p value |
|
Sex |
|
|
|
|
|
|
Male - no. (%) |
30 (42.3) |
31 (43.7) |
8 (11.3) |
2 (2.8) |
0.023 |
|
Female - no. (%) |
24 (70.6) |
10 (29.4) |
0 (0) |
0 (0) |
|
|
Age (years) |
|
|
|
|
|
|
20-29 - no. (%) |
22 (75.9) |
5 (17.2) |
2 (6.9) |
0 (0) |
0.008 |
|
30-39 - no. (%) |
21 (56.8) |
12 (32.4) |
3 (8.1) |
1 (2.7) |
|
|
40-49 - no. (%) |
11 (28.2) |
24 (61.5) |
3 (7.7) |
1 (2.6) |
|
with the mean age of F0, F1, F2, and F3 fibrosis staging being 31.5±8.1 years, 38.5 ±7.0 years, 37.4 ± 9.5 years, and 43± 5.7 years, respectively (p=1.66×10-4). However, no significant difference was seen for HBV DNA levels, as HBV DNA levels of patients demonstrating F0, F1, F2, and F3 fibrosis staging were 7.43 ± 0.32 log10 IU/mL, 7.55 ± 0.34 log10 IU/mL, 7.50 ± 0.38 log10 IU/mL, and 7.46 ± 0.55 log10 IU/mL, respectively (p=0.386).
DISCUSSION
During the natural history of HBV infection, the immune tolerance phase is characterized by persistently normal ALT levels and a high viremia, which is probably a result of clonal deletion of T cells against HBV in the fetus induced by in-utero exposure to HBeAg [1]. Persistently normal ALT is associated with excellent long-term prognosis [10]. However, a normal ALT level does not mean normal liver histology. Chotiyaputta reported that significant liverdisease was observed in 20% ofpatientswhohad normal ALT [11]. Alam reported that 52.7% of HBeAg-positive chronic hepatitis B patients with normal ALT had histological activity index ≥4. In HBeAg-negative chronic hepatitis B patients with normal ALT status, the proportion was 23.1% [12]. Although transient elastography, ultrasound and other serum markers have a particular significance [13] and despite the risk of severe complications (1/4,000–10,000), liver biopsy has been the gold standard to evaluate liver histology.
The ULN of ALT levels is an interesting topic. A study of 6835 blood donors and 209 persons with anti-HCV antibodies (131 with HCV viremia) showed that serumALT activity was independently related to body mass index and to laboratory indicators of abnormal lipid or carbohydrate metabolism [8]. Updated ULNof 30 U/L and 19 U/L, for males and females, respectively, were lower than current limits of 40 U/L and 30 U/L, for men and women, respectively.During a6-month follow-up, the updated, lower ULN showed superior sensitivity in identifying participants with HCV viremia [8]. Furthermore, the increased sensitivity targeted patients with minimal to mild histologic lesions [8]. However, the question of whether there is any difference in the histological activity between low ALT (below the updated standard) and high ALT (between the updated standard and the current laboratory standard) groups in chronic hepatitis B virus carriers with persistently normal ALT remained to be answered.
Furthermore, though the prevalence of chronic HBV infection in females is similar to males, the rate of active hepatitis in females is significantly less than in males [14]. Since perinatally acquired HBV is the main model for chronic HBV infection in China, age is considered to be an important factor associated with the progression of HBV-related disease.Serum HBV DNA level is an important marker in immune tolerance phase patients. Several important issues remained to be elucidated, including any potential relationship between liver histological activity and sex, age, or HBV DNA levels in patients with normal ALT, andin the absence of liver biopsy evidence, how the degree of liver histology should be determined by other means.
In this study, ALT level showed a significant positive correlation with both inflammation and fibrosis score. Almost all patients in thelow ALT groupdemonstrated mild histological inflammation and fibrosis. The Ishak inflammation grading and fibrosis score of the low ALT group were significantly lower than in the high ALT group. Therefore, the new suggested ULN is more accurate than the currently used laboratory standard in evaluating mild inflammation. In reality, the low ALT group is more consistent with the characteristics of “immune tolerance” compared withthe high ALT group. According to this result, for most low ALT group patients, liver biopsy is seemingly unnecessary, and currently, antiviral treatment is not recommended for “immune tolerance phase” patients.
In addition, in the high ALT group, over a third of cases showed moderate or severe inflammation and nearly 1/10 cases had F2 or F3 Metavir fibrosis staging. According to this result, for high ALT group patients, over 30% of “immune tolerance phase” patients should be considered for antiviral treatment to relieve the observed liver inflammation. Therefore, more factors should be considered in the high ALT group in view of a higher proportion of moderate/severe inflammatory activity.
We further sought to determine whether patients could be screened for moderate/severe inflammation or fibrosis in the high ALT group according to sex, age, and HBV DNA levels.In this study, age was found to be a positively correlating factor with inflammation or fibrosis score, whether in the low or high ALT group. Histological score of inflammation or fibrosis increased with age, but not with HBV DNA or ALT levels. In China, HBV is most frequently transmitted perinatally from infected mothers to neonates. Undersuchapresupposition, age means the time of HBV infection. Therefore, according to this study, age is an important factor to judge liver histology. Furthermore, inflammation or fibrosis scores in maleswere significantly higher than in females. However, HBV DNA level did not correlate with inflammation or fibrosis. Yuen reported that there was no association between HBV DNA levels and liver histology in HBeAg-positive patients [15]. Conversely, Bai reported that there was a positive correlation between serum HBV DNA level and hepatic inflammation in both HBeAg-positive and HBeAg-negative patients aged ≥35 years,but in patients aged <35 years, positive correlation was only observed in HBeAg-negative patients [16]. According to this study, in the high ALT group, males aged >40 years are associated with moderate/severe inflammation and would seemingly need to undergo liver biopsy to judge the true extent of liver pathology
To our knowledge, the presentwork is the first histology study during the immune tolerance phase to take different ALT levels into account. Although the histological inflammation and fibrosis of patients over 50 years and less than 20 years of age were not included in our study, the improved treatment strategy of those patients aged between 20 years and49 years should play a key role in the prognosis of end-stage liver disease.
CONCLUSION
In conclusion, the newly suggested ULN of ALT is better than the currently used standard in evaluating liver histology in immune tolerance phase patients. For patients with ALT levels >30 in males or >19 in females, sex and age, but not HBV DNA levels, are associated with the degree of inflammation and fibrosis.
ACKNOWLEDGMENTS
We wish to acknowledge Chengyu Yan and Jinfeng Li for their operation of liver biopsy. We wish to acknowledge helpful suggestions, discussions and excellent technical assistance fromProf. TianfuGan.