Pneumonectomy in 57 Patients: Etiologies and Postoperative Follow-Up
- 1. Department of Thoracic Surgery, Hospital Center University Hassan Ii, Morocco
- 2. Department of Medicine and Pharmacy, Sidi Mohamed Ben Abdallah University, Morocco
Abstract
Introduction: Pneumonectomy presents an anatomical resection with a high rate of mortality and morbidity. This rate is still increased in the infectious affections such as destroyed lung. The serious complication after pneumonectomy remains bronchial fistula which requires an extended management.
Methods: It was a retrospective study including all patients who had benefited of a pneumonectomy. The aim is to characterize clinical, paraclinical, and operative data.
Results: Among 57 patients, there were 35 men and 22 women, with an average age of 42.6 years old. Respectively, pathological antecedents and clinical symptomatology were predominated by tuberculosis in 29 patients (50.8%) and the combination of haemoptysis with bronchorrhea in 23 patients (40.35%). imaging showed right-sided involvement in 28 patients (49.2%). The etiologies were predominated mainly by destroyed lung of tuberculosis origin in 34 patients (59.6%). Extrapericardial pneumonectomy was performed in 40 patients (70.1%), and intrapericardial in 15 patients (26.3%). 14 patients were presented a hemorrhage (24, 5%), postpneumonectomy empyema was recorded in 4 patients (7%), and death of 3 patients (5,2%). Long-term follow-up was 2 years without any marked recurrence.
Conclusion: Pneumonectomy is accompanied with a high rate of mortality and morbidity. A well analysis of risk factors and good selection of patients allows decreasing this rate.
Keywords
Pneumonectomy; Lung cancer; Bronchorrhea.
CITATION
Harmouchi H, Rabiou S, Belliraj L, Ammor FZ, Issoufou I, et al. (2018) Pneu monectomy in 57 Patients: Etiologies and Postoperative Follow-Up. J Liver Clin Res 5(2): 1052.
INTRODUCTION
The lung cancer remains the main indication for anatomical resections of the lung, especially in countries where screening methods for lung cancer are developed. In our context, anatomical resections of the lung are frequently used for infectious diseases, mainly for parenchymal sequelae of tuberculosis, such as bronchiectasis and aspergilloma [1,2]. Pneumonectomy, performed firstly by Graham and Singer in n1933 for a bronchogenic carcinoma [3], is a high-risk surgical procedure consisting of an anatomical resection of the entire lung. It is indicated in infectious pathology, mainly for destroyed lung, as long as the tumor pathology especially lung cancer. In this series, we will try to specify the particularity of the practice of pneumonectomy within our service.
MATERIAL AND METHODS
Into our department of thoracic surgery in CHU Hassan II Fez, all patients who received pneumonectomy over eight years (2010-2017) were included, by recording prospectively, clinical, paraclinical, and operative data. Our goal in this monocentric study is to specify the etiological profile of these patients, as well as the postoperative complications.
RESULTS
Among 57 patients, there were 35 men and 22 women, with a sex ratio of 1.59. The average age was 42.6 years old. pathological antecedents were predominant for tuberculosis in 29 patients (50.8%), chronic smoking in 11 patients (19.3%), closed chest trauma in 2 patients (3.5%), recurrent bronchopneumopathies in 2 patients (3.5%), and pulmonary epidermal carcinoma operated in a single patient (1.75%). clinical symptomatology was predominated by the combination of haemoptysis with bronchorrhea in 23 patients (40.35%), isolated haemoptysis in 14 patients (24.5%), dyspnea in 12 patients (21%), isolated bronchorrhea in 7 patients (12.2%), and a fortuitous discovery of a pulmonary nodule in the context of extension assessment in a single patient (1.75%). imaging showed right-sided involvement in 28 patients (49.2%), and left-sided involvement in 29 patients (50.8%). The chest CT scan showed a destroyed lung in 34 patients (59.6%), a tumor-like process in 15 patients (26.3%), and an endobronchial process in 3 patients (5.3%), an aspergilloma in 2 patients (3.5%), an aneurysm single-patient pulmonary artery (1.7%), left-sided bronchus rupture in one patient (1.7%), and post-traumatic stenosis in one patient (1.7%). The etiologies were predominated not the destroyed lung of tuberculosis origin in 34 patients (59.6%), and the tumoral pathology in 18 patients (31.5%) (Figure 1),
Figure 1: Operative piece showing a carcinoid tumor of the right upper bronchi extended to the main right bronchus.
and post-traumatic involvement of the left bronchus in 2 patients ( 3.5%), aspergilloma in 2 patients (3.5%), and aneurysm of the pulmonary artery by Behçet’s disease in a single patient (1.7%). All patients were treated by a posterolateral thoracotomy conservative of the chest wall muscles, mainly the latissimus dorsi muscle. The extra pleural plan was discussed in 37 patients (65%), and protection of the bronchial stump was performed in 52 patients (91.2%). extrapericardial pneumonectomy was performed in 40 patients (70.1%), and intrapericardial in 15 patients (26.3%), pleuropneumonectomy in one patient (1.7%), and completion pneumonectomy in one patient (1,7%). Extrapleural approach was done in 37 patients (64, 9%), and flap for bronchial stump was performed for all patients (100%). for complications, 14 patients were presented a heamorrhage (24,5%), postpneumonectomy empyema was recorded in 4 patients (7%), and death of 3 patients (5,2%). Long-term follow-up was 2 years without any marked recurrence (Tables 1-4).
|
Table 1: Patient characteristics. |
|
|
|
|
Number of patients (Percentage) |
|
|
median age |
42.6 years |
|
|
sex: -male -female |
35 (61,4%) 22 (38,6%) |
|
|
Pathological antecedents: -Tuberculosis -Chronic smoking -Recurrent bronchopneumopathies -Closed chest trauma -Pulmonary epidermal carcinoma operated |
29 (50.8%) 11 (19.3%) 2 (3.5%) 2 (3.5%) 1 (1.75%) |
|
|
Clinical symptomatology -haemoptysis with bronchorrhea -isolated haemoptysis -dyspnea -isolated bronchorrhoea -fortuitous discovery of a pulmonary nodule |
23 (40.35%) 4 (24.5%) 12 (21%) 7 (12.2%) 1 (1.75%) |
|
|
Table 2: Radiological features of patients. |
|
|
|
Number of patients (percentage) |
|
side reached: -Right -Left |
28 (49.2%) 29 (50.8%) |
|
Chest CT scan: -Destroyed lung -Tumor-like process -Endobronchial process -Aspergilloma -Aneurysm single-patient pulmonary artery -Left-sided bronchus rupture -Post-traumatic stenosis |
34 ( 59.6%) 15 (26.3%) 3 (5.3%) 2 (3.5%) 1(1.7%) 1(1.7%) 1(1.7%) |
|
Table 3: Indications of pneumonectomies. |
|
|
|
Etiologies |
Number of patients (percentage) |
|
|
Destroyed lung after tuberculosis carcinoid tumor Adenocarcinoma Epidermal carcinoma Aspergilloma Closed chest trauma Aneurysm of the pulmonary artery pneumoblastoma |
34 (59.6%) 5 (8,7%) 9 (15,7%) 3 (5,2%) 2 ( 3.5%) 2 ( 3.5%) 1 (1.7%) 1 (1.7%) |
|
|
Table 4: Complications of pneumonectomies in our series. |
|
|
|
Number of patients (percentage) |
|
Heamorrhage |
14 (24,5%) |
|
Empyema postpneumonectomy |
4 (7%) |
|
Death |
3 (5,2%) |
DISCUSSION
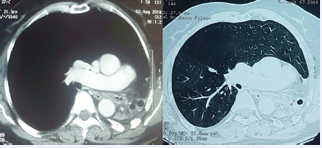
Lung cancer is known the leading cause for pneumonectomy, because of development of screening methods, and the decrease of infectious pathology in the world by therapeutic advances. Therefore, Tuberculosis remains a significant public health problem in Morocco, whose determinants are mainly represented by adverse socio-economic conditions, which explains the rate of pneumonectomy made for destroyed lung and aspergilloma in this series to 63,1%. Pneumonectomy differs in some points according to whether the etiology is infectious or tumoral. Clinically, the tumoral pathology is manifested mainly by hemoptysis, thoracic pain, whereas in the infectious pathology is especially discovered by hemoptysis and bronchorrhea (76, 5% in our series). On the respiratory functional plane, the patients carrying a destroyed lung (Figure 2)
Figure 2: Computed CT objectifying a left destroyed lung post tuberculosis with mediastinal deviation.
are accustomed with this parenchymatous destruction, and in our experience the realization of pneumonectomy remains feasible on the respiratory level, except in cases where forced expiratory volume in one second is very low. While in a patient with lung cancer of the right upper lobe that invades the fissure for example, resection of the healthy pulmonary parenchyma is performed, which makes the respiratory function of the patient altered postoperatively, Surgically, sequels of tuberculosis, such as the bronchiectasis and the aspergilloma is accompanied by a important bleeding complications, because of the importance of pleuroparietal adhesions, collateral arterial circulation, and sometimes calcifications in the hilar region (24,5% of bleeding complications in our series). While in tumor affections, lung is not very adherent to chest wall, and so the liberation of the lung is easy and not bleeding. All this data explains the increase rate of mortality and morbidity of pneumonectomy for chronic inflammatory pathologies than other affections [4,5].
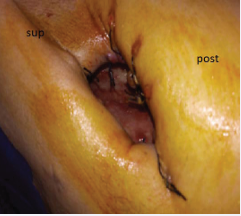
The most feared complication for any thoracic surgeon after pneumonectomy is the bronchial fistula, which leads to postpneumonectomy empyema, requiring a prolonged management by thoracostomy (Figure 3) or thoracmyoplasty [6].
Figure 3: Patient receiving a thoracostomy after an empyema postpneumonectomy.
Of the 4 patients with postpneumonectomy empyema in this study, 3 had a right location. Several series in the literature have shown that the risk of empyema postpneumonectomy and death is higher when pneumonectomies are realized on the right side compared to the left side, without an unambiguous physiological explanation [7,8]. In other words, mortality at 30 days postoperatively is more important after right pneumonectomy than left pneumonectomy, and this right pneumonectomy is a risk factor independent of occurrence of broncholpeural fistula [9]. Thus, in order to avoid this serious complication, we perform systematically a flap of adjacent tissues to protect the bronchial stump, most often by pleural, intercostal, or thymic tissue. Our attitude is to don’t drain patients with pneumonectomy after surgery intervention in order to reduce the risk of postpneumonectomy empyema [10]. Also, the preservation of the latissimus dorsi muscle in the thoracotomy finds its place for eventual thoracomyoplasty in case of empyema of the cavity. Operative mortality from pneumonectomy has been reported to be between 5% and 20% [11,12]. The mortality rate in our series was to 5,2%, which corresponds to the literature.
CONCLUSION
The high incidence of morbidity and mortality after pneumonectomy implies a good selection of patients based on the analysis of well-defined risk factors before making the decision to perform a pneumonectomy. This will lead to a significant decrease in postoperative complications. This study precise the frequency of infectious pathology in the realization of pneumonectomy and its operative and postoperative difficult management.