Primary Hydatid Cysts of the Mediastinum
- 1. Department of Thoracic and Cardiovascular Surgery, Tunis El Manar University, Tunisia
- 2. Department of Thoracic Surgery, Tunis El Manar University, Tunisia
Abstract
Introduction: Mediastinal primary hydatidosis (MH) is a very rare condition (0,3 to 1,3% of thoracic hydatidosis (TH)) it results from direct implantation and development of the parasite embryo in the mediastinum.
Material and methods: During a period of 30 years (1985 – 2014) we have observed 13 cases of mediastinal hydatidosis among 3142 cases of thoracic hydatidosis (0.4%). Diagnosis was based on clinical symptoms and chest radiography associated with transthoracic ultrasonography (TUS), computed tomography (CT) or magnetic resonance imaging (MRI). All diagnosed cases were proposed to surgical resection.
Results: There were 7 males and 6 females aged between 13 and 64 years (mean age 33.15). The cyst was unilocular (CE1) in one case and multilocular (CE2) in 12 cases. Cyst location was anterior mediastinum in 8 cases, middle mediastinum inCE 3 and posterior mediastinum in 2. A liver cyst was present in 4 cases and spleen cyst in 2. The surgical treatment consisted in cystectomy or pericystectomy in 12 cases; in one case a right pneumonectomy was necessary because the cyst had totally destroyed the right pulmonary artery in its mediastinal and intrapulmonary segments.
The postoperative course was uneventful in all cases. One patient relapsed ten years later and was reoperated.
Conclusion: Mediastinal hydatidosis is exceptional and must be distinguished from secondary mediastinal invasion that may be observed in secondary pleural hydatidosis or costo-vertebral hydatidosis.
Diagnosis may be made by modern imaging means associated with serological tests.
Surgical resection is the unique radical treatment.
Keywords
Primary Mediastinal Hydatidosis ; Diagnosis ; Surgery.
CITATION
Kilani T, Zribi H, Zairi S, Abdennadher M, Marghli A (2017) Primary Hydatid Cysts of the Mediastinum. J Liver Clin Res 4(1): 1033.
ABBREVIATIONS
CE: Cystic Echinococcosis; MH: Primary Mediastinal hydatid cyst; TUS: Transthoracic Ultrasound Examination; CT: Computed Tomography; MRI: Magnetic Resonance Imaging
INTRODUCTION
Primary mediastinal hydatidosis (MH) is a very rare condition which accounts for 0.3 to 1.3% of possible thoracic hydatid locations (TH) [1-3]. It results from direct implantation and development of the parasite in the mediastinum. It must be distinguished from local mediastinal extension of pleural or thoracic wall hydatidosis (spinal, costal or sternal location). Surgical resection remains the more efficient treatment.
MATERIAL AND METHODS
During 30 years (1985 – 2014), 13 cases of primary mediastinal hydatid cysts were managed among 3142 cases of thoracic hydatidosis (0.4%). Diagnosis was primarily based on clinical symptoms and chest radiography. Different imaging tools were associated to confirm the diagnosis such as transthoracic ultrasonography (TUS), computed tomography (CT) or magnetic resonance imaging (MRI). All of our patients underwent surgical resection. They didn’t receive any preoperative medical treatment.
RESULTS
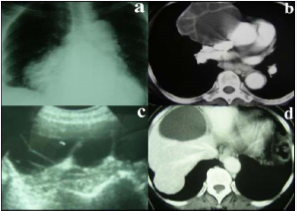
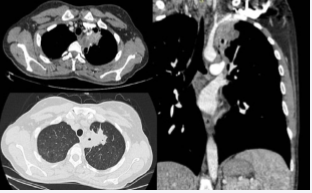
There were 13 patients, 7 males and 6 females aged between 13 and 64 years (mean age of 35.8). Two patients (15.4%) had previous surgery one for intra-abdominal hydatid cysts (in the liver and spleen) and the second for bilateral lung hydatidosis, respectively 9 and 15 years ago. The patients were symptomatic in 10 cases (77%). They presented with chest pain in 6 cases (46%), cough in 3 (23%), dyspnea in 3 (23%), supraclavicular mass in 2 (15%) and haemoptysis in 1 (7.5%). All patients had plain chest X-rays. CT-scan had been performed in 12 patients (92.3%) and MRI in 4 (60.7%). Partial calcifications of the pericystic wall were present in two cases (15.3%). The mediastinal mass had been investigated by TUS in 8 patients (61.5%), which showed multilocular hydatid cyst (CE2 stage of the WHO-IWGE classification) 7 cases (53.8%) and unilocular cyst (CE1 stage of the WHO-IWGE classification) in one (7.7%). Abdominal systematic screening with ultrasonography, revealed liver hydatid cysts in 4 cases (30.7%) (Figure 1, Case n°12) and spleen involvement in 2 cases (15.4%).
Figure 1: Chest CT-scan showing multilocular CE2 superior anterior right mediastinal hydatid cyst with an associated liver cyst (Abdominal ultrasonography and CT-scan). (Case n°12)
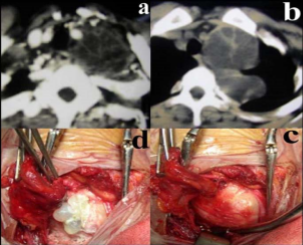
All of our patients underwent surgical resection through a posterolateral thoracotomy in 11 cases (84.6%) and a supraclavicular approach (Figure 2, Case n°8) in 2 cases for cervico-mediastinal hydatid cysts.
Figure 2: Cervico-mediastinal hydatid cyst operated through supraclavicular approach. (Case n°8)
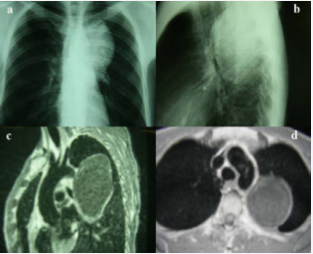
One patient with left posterior MH and hyperhidrosis had bilateral sympathectomy at the same time through a right VATS approach and left thoracotomy (Figure 3, Case n°13).
Figure 3: Chest X-ray and CT-scan images showing left posterior mediastinal hydatid cyst. (Case n°13)
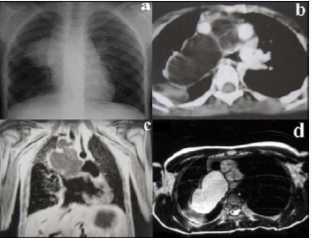
Intra-operatively, the cyst was unilocular in one case (CE1) and multilocular (CE2) in 12 cases (92.3%), with a mean size of 7.4 cm (4-15 cm). The antero-superior mediastinum was the main location in 8 cases (61.5%). The cervico-mediastinal region was involved in 2 cases (15.4%), the middle mediastinum in 1 case (7.7%) and the posterior mediastinum in 2 cases (15.4%). The diagnosis of primary mediastinal hydatid cyst is confirmed by the presence of a unique cyst into the mediastinal space covered with mediastinal pleura and without any associated regional primary cyst (in the lung or diaphragm or liver) that may have ruptured and induced a secondary hydatidosis. Surgical treatment consisted in cystectomy or pericystectomy in 12 cases (92.3%). A right pneumonectomy was performed in one case because of complete destruction of the right pulmonary artery in its mediastinal and intrapulmonary segments (Figure 4, Case n°7).
Figure 4: Chest CT-scan showing multilocular CE2, 8cm mediastinal mass with compression of the right PA, SVC and trachea. (Case n°7)
The postoperative course was uneventful in all cases. Antihelminthic treatment was associated for 6 months only in one case because of intra-operative accidental rupture of a tension multilocular left cervico-mediastinal cyst, which extended from the anterior to the posterior mediastinum under the thoracic duct arch and contracted dense adherences with the subclavian vessels and the spine without vertebral involvement (Case n°8). The same patient relapsed 10 years later. She presented with left subclavian pain and hydatid vomica. CT imaging showed left mediastinal muli-locular cyst, which had ruptured through a fistula into a segmental culminal bronchus (Figure 5).
Figure 5: Recurrent CE2 MH close to the left subclavian artery invading the lung parenchyma and containing air signing bronchial fistulisation. (Case n°8)
The patient was reoperated through a postero-lateral thoracotomy and had subtotal pericystectomy for the mediastinal part and wedge resection of the parenchymal lesion. The details of our 13 cases are summarized in table[1].
|
Table 1 : |
|||||||
|
Case |
Sex |
Age |
Symptoms |
Chest X-Rays |
CT - MRI |
US |
Surgery |
|
1 |
M |
34 |
-Pain - Dyspnea |
-Right superior mediastinal shadow -Tracheal displacement to the left |
-CT: Multilocular 5cm mixed tumor |
Multilocular HC |
-Multilocular CE2 superior anterior right MC -Subtotal pericystectomy |
|
2 |
F |
57 |
-Pain - Dyspnea |
-Right anterior mediastinal shadow -Compression to the right lung and tracheo-bronchial tree |
-CT: Multilocular 15cm cystic mass in the anterior mediastinum extending from the apex to the diaphragm |
-Multilocular cystic mass: HC or lymphangioma? |
-Multilocular CE2 right mediastinal HC anterior to the pulmonary pedicle from the apex to diaphragm -Displacing SVC, IVC, esophagus and trachea -Subtotal pericystectomy |
|
3 |
F |
35 |
-Cough -Wheezing -Dyspnea |
-Right anterior mediastinal shadow -Tracheal displacement posteriorly to the left. |
-CT: Unilocular 6cm anterior cystic mass between vessels and trachea |
-Unilocular cystic mass -Spleen HC |
- Unilocular CE1 HC between trachea and brachiocephalic artery - Cystectomy |
|
4 |
M |
55 |
-Cough for 6 months |
-Right hilar shadow |
-CT: Multilocular 4cm right anterior and mid mediastinal cystic mass |
-2 liver cysts |
-Multilocular CE2 HC close to the superior right pulmonary vein Lymph node location? |
|
5 |
M |
52 |
-Surgery for liver cyst 9 years ago -Spleen and peritoneal hydatidosis |
-Left anterior mediastinal shadow |
-CT + MRI: Multilocular 12cm HC in the anterior left mediastinum |
Normal cardiac US |
-Multilocular CE2 HC close to aortic arch, main pulmonary artery superior pulmonary vein and left main bronchus -Cystectomy |
|
6 |
M |
18 |
-Pain for 2 months |
-Right latero-tracheal shadow |
-CT: Multilocular 7.5cm cystic mass close to trachea and ascending aorta |
|
-Multilocular CE2 HC in the anterior mediastinum close to sternum, SVC, right PA -Total pericystectomy |
|
7 |
F |
13 |
-Cough - Hemoptysis |
-Right mediastino-hilar shadow |
-CT + MRI: Multilocular 8cm mediastinal mass -Compression to right PA, SVC and trachea |
-Multilocular mediastinal cyst |
-Multilocular CE2 mediastinal and hilar HC destroying right PA -Cystectomy – right pneumonectomy |
|
8 |
F |
23 |
Left supra clavicular mass for 1 year |
-Left mediastinal shadow |
-CT: Multilocular 8cm left cervico-mediastinal mass |
-Multilocular MC |
-Supra clavicular approach -Multilocular CE2 HC - Cystectomy -Medical treatment 6 months -redo surgery at 10 years for local recurrence by left thoracotomy |
|
9 |
F |
39 |
-Cervicobrachial pain -Right supra-clavicular mass |
-Right cervico-mediastinal shadow |
-CT: 8cm multilocular cervico-mediastinal mass at the right of trachea and posterior to SVC and subclavian vessels |
-Multilocular HC |
-Supra clavicular approach -Multilocular CE2 HC -Cystectomy |
|
10 |
M |
34 |
-Dyspnea – Left thoracic pain for 6 months |
Left polycyclic anterior mediastinal shadow |
-CT: 5cm multilocular HC with calcifications left to main PA |
|
-Multilocular CE2 HC of the left thymic lobe -Total pericystectomy |
|
11 |
M |
32 |
-Left thoracic pain |
-Left costo-vertebral sinus shadow extending from T5 to T12 |
-CT + MRI: 12cm multilocular cystic mass in the Middle and posterior mediastinum -Partial calcification |
|
-Multilocular CE2 HC of the posterior mediastinum -No spinal or rib lesion -Subtotal pericystectomy |
|
12 |
F |
64 |
Asymptomatic -Surgery for lungs and liver hydatidosis 15 years ago |
-Right anterior cardio-phrenic angle shadow |
-CT: 10cm multilocular anterior and inferior right mediastinal cyst -Liver cyst |
-Multilocular mediastinal HC -Unilocular liver cyst |
-Multilocular CE2 anterior MC -Thoraco-phrenotomy -Cystectomy -Pericystectomy for liver cyst |
|
13 |
M |
33 |
-Symptom free for HC -Hyperhidrosis
|
-Left posterior mediastinal shadow suggestive of neurogenic tumor |
-MRI: 9cm posterior left mediastinal cystic mass close to the descending aorta |
-Liver cyst -Mediastinal left HC |
-Bilateral sympathectomy -Simultaneous right VATS and left thoracotomy -Multilocular CE2 posterior left mediastinal cyst treated by cystectomy |
DISCUSSION
Primary mediastinal hydatidosis results from parasite seeding through the systemic mediastinal arteries. After going through or bypassing the liver and lung filters, the echinococcal embryo freed from the ingested egg reaches the aortic arterial bloodstream and then the mediastinum. The parasite implantation may occur through: the mediastinal arteries which spring from the thoracic descending aorta and irrigate the mediastinal soft tissues, the bronchial and intercostal arteries which give rise to small branches for the lymphatics of the mediastinum, or the thymic arteries originating from the subclavian arteries. The significant thymic blood supply, mainly in young patients, may explain the high frequency of thymic locations of MH [1]. Like any other mediastinal tumor, MH may be silent for a long time. Symptoms are related to the cyst’s size and impingement on neighboring organs. Signs like dry cough, chest pain, left recurrent laryngeal nerve paralysis, Horner syndrome, or superior vena cava syndrome may be present. Initially, young cysts are unilocular, with a germinative membrane, surrounded by the pericystic wall, which consists of compressed surrounding host tissues. Cyst’s development leads to parasite suffering with endogenous multiloculation (development of daughter cysts) and then enlargement of the cyst with possible calcification of the pericyst [1-5]. Erosion or destruction with rupture in surrounding structures is the main risk. The cyst may rupture into the pleural cavity with the development of secondary pleural hydatidosis. Hydatid cyst rupture into the aorta or pulmonary artery results in systemic or pulmonary artery hydatid emboli [6,7]. Among our patients, we reported complete destruction of the right pulmonary artery which extended from its mediastinal retro-caval segment to its basal part. There was a great damage and no arterial reconstruction feasible. Therefore, right pneumonectomy was performed (Case n°7). Diagnosis of mediastinal involvement is made according to the imaging features. Thoracic chest x-rays may show a mediastinal mass shadow. Arcuate peripheral calcifications may be observed. If the lesion is reachable through the chest wall or the cervical region, ultrasound investigation may confirm the cystic nature with the typical “double contour” feature of the germinative membrane, or a multilocular highly suggestive aspect of numerous intra-cystic daughter cysts. The WHO-IWGE ultrasound classification [8] have been described and is mainly used for liver and abdominal CE, in the thorax and especially in the mediastinum the reported cases are mainly represented by CE1 (young unilocular cysts) or CE2 (multilocular cysts) CT or MRI generally confirms the diagnosis showing a typical cystic unilocular tumor or a complex mass with daughter cysts. High density complex cysts are more difficult to assess [8]. If epidemiological suspicion is present, serological tests may be helpful if they are positive. We do not use these tests routinely because of their high rates of false negative and false positive results in endemic region population [2,9]. MH is generally a unique cystic compressive mediastinal mass, which may be unilocular (CE1) or multilocular (CE2). Differential diagnosis may be discussed with other cystic mediastinal tumors, such as: thymic cyst, bronchogenic cyst, pleuro-pericardial cyst for unilocular MH and with lymphangioma (Figure 6)
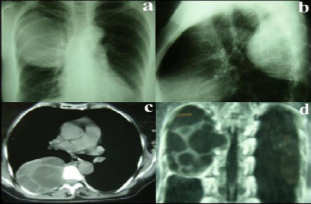
Figure 6: Chest X-ray, CT-scan and MRI showing multilocular cyst extending from the anterior to the posterior mediastinum and surrounding the superior vena cava = cystic lymphangioma that may be confused with mediatinal hydatidosis
for multilocular MH. Diagnosis may also be discussed with the other aspects of thoracic hydatidosis that may develop close to the mediastinum. Secondary hydatidosis must be evoked in multiple cysts and patients previously operated for hydatidosis. Secondary pleural hydatidosis is generally multi-focal, mainly located in pleural sinuses. It may “invade” the mediastinum and complicate in it. Costo-vertebral hydatidosis may extend to the mediastinum with the development of para-vertebral hydatid abscesses [10]. Vertebral bodies or ribs destruction on CT or MRI may confirm the diagnosis (Figure 7).
Figure 7: Chest X-ray and CT-scan showing multilocular CE2 hydatid cyst in the posterior mediastinum with vertebral involvement and scalloping on the ribs = spinal hydatid cyst extended to the mediastinum.
These hydatic locations need extended resection of “infected” bone structures to avoid recurrence. We think that some reported cases of posterior mediastinal cysts are in fact, vertebral cysts with spinal destruction and spinal canal invasion. This may explain why some publications consider that posterior mediastinum is the main location of MH [11,12]. Mediastinal hydatidosis requires surgical treatment. Surgery has to eradicate the parasite, avoiding intra-operative dissemination. The pericyst is treated if possible by total pericystectomy. Resection of pericystic parts close to the heart, vessels or esophagus may be risky. Therefore, they may be left in place when necessary, taken that all the parasitic material is removed. The operative field needs to be washed with a scolicidal solution. Formalin is not used in the thorax because of its high toxicity. Hypertonic sodium chloride solutions (20% or more) may be caustic and may cause hypernatremia. Cetrimide is an effective scolicidal solution that may cause methemoglobinemia and metabolic acidosis [13,14]. We routinely use 10% Hydrogen peroxide solution. In a personal in-vitro study, we have demonstrated the efficiency of hydrogen peroxide compared to hypertonic saline solution [15]. High concentration or high doses use, or irrigation under high pressure of hydrogen peroxide may lead to gaseous emboli in exceptionally reported cases [16,17]. Medical treatment with benzoimidazole carbamates (Albendazole or Mebendazole) remains insufficiently efficient in complex hydatidosis. These drug effects are variable, because of bad uptake and low bioavailability in the blood stream and into the cyst, despite the necessity of a 6 to 12-month-treatment and a significant toxicity (hepatic, hematologic and hair loss). This therapy must be reserved to inoperable cases [18-20]. We do not use medical treatment in hydatid disease routinely, neither for therapeutic nor preventive purposes and in our reported series we observed a recurrence of the disease despite 6 months of postoperative medical treatment (case n°8).
CONCLUSION
Mediastinal hydatidosis is exceptional and have to be distinguished, from secondary mediastinal invasion that may be observed, in secondary pleural hydatidosis, or costo-vertebral hydatidosis. Diagnosis may be made by different imaging techniques, associated with serological tests. Surgical resection is the unique efficient treatment. Although exceptional MH have to be kept in mind and should be evoked in case of a mediastinal cystic lesion in endemic areas.