Thoracoscopic Treatment of Massive Hemorrhagic Complication Due to Diaphragm Injury after Radiofrequency Ablation of Hepatocellular Carcinoma
- 1. Department of Internal Medicine, Tainan Municipal Hospital, Taiwan
- 2. Department of Surgery, Tainan Municipal Hospital, Taiwan
Abstract
The clinical application of radiofrequency ablation (RFA) of hepatic tumor has gradually been accepted as an effective and safe method for the treatment of small hepatic malignant tumors. However, the potential complications were often overlooked. We report a case of hepatitis C related hepatocellular carcinoma (HCC), who developed a massive hemothorax after a RFA procedure for treatment of recurrent HCC. The cause of hemothorax was finally proved to be a RFA needle injury of a diaphragm vessel and successively treated by a minimally invasive thoracoscopic surgery. Hemothorax after RFA procedure was long been thought as intercostals arterial injury, however, our case demonstrated that diaphragm injury might be the cause of RFA related hemothorax rather than intercostal artery injury, at least in some cases
Keywords
epatocellular carcinoma; hepatic; Radiofrequency ablation.
CITATION
Mo LR, Wu HH (2016) Thoracoscopic Treatment of Massive Hemorrhagic Complication Due to Diaphragm Injury after Radiofrequency Ablation of Hepatocellular Carcinoma. J Liver Clin Res 3(1): 1022.
INTRODUCTION
Radiofrequency ablation (RFA) treatment for the malignant neoplasm of liver is now a widely accepted minimally invasive method [1]. The safety and efficacy in the treatment of hepatic malignancies have been reported extensively. Although RFA procedure is a relatively safe modality, some major complications and even mortality may occur after the procedure [2-4]. We report a rare case of massive hemothorax due to diaphragm injury and successfully treated with thoracoscopic suture of the bleeder.
CASE REPORT
A 67-year old female patient was admitted for the treatment of recurrent small hepatocellular carcinoma (HCC) at segment 7. She is a patient with hepatitis C related liver cirrhosis, Child-Pugh A, receiving regular ultrasound surveillance since the age of 52. in August 2002, a small hepatic tumor was found at segment 2 about 2 cm in diameter. She received a left lateral segmentectomy and the pathological report revealed a well differentiated HCC. After surgery, she received regular ultrasound surveillance every three months. During this period, 3 times of tumor recurrence were found in 2006, 2008, and 2009, respectively. She received RFA for the small HCC at each time of tumor recurrence uneventfully.
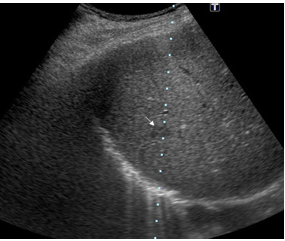
In August, 2012, a small hypo echoic tumor about 1.6 cm in diameter was found again on routine ultrasound surveillance at segment 7 of liver (Figure 1).
Figure 1: Ultrasound examination showed a small hypo echoic nodule (arrow) at S7. Biopsy showed well differentiated hepatocellular carcinoma.
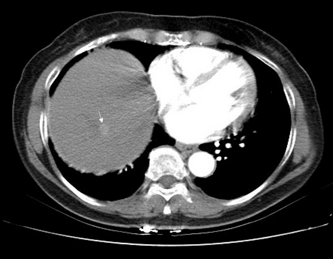
CT scan showed a small hyper vascular nodule at the same site (Figure 2).
Figure 2: CT scan showed a hyper vascular nodule at S7 (arrow).
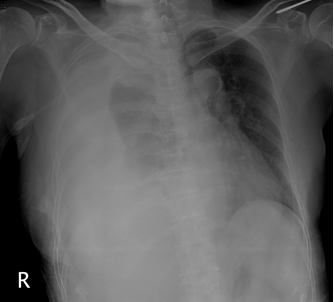
She was arranged for admission to receive another course of RFA. On admission, the laboratory test showed elevation of serum AST/ALT (89/104 IU/mL) with serum albumin 4.0 gm/L, AFP 2.5 ng/mL, and CBC count showed mild decrease of platelet 83,000/mL, hemoglobin 12.5 mg/mL. Prothrombin time was normal with INR 1.05. Under IV general anesthesia (propofol based), percutaneous RFA under ultrasound guidance was performed successively with Cool-tip needle (Radionics) successively. Unfortunately, the patient developed dyspnea and fainting spell about 4 hours after the procedure. A chest X-ray showed massive right pleural effusion (Figure 3)
Figure 3: Chest X-ray demonstrated massive pleural effusion.
and blood hemoglobin down to 7.0 gm/L. Hypo perfusion with low blood pressure down to 90/60 and pulse rate 124/minutes were also found. After fluid resuscitation and packed RBC transfusion, the vital signs gradually stabilized.
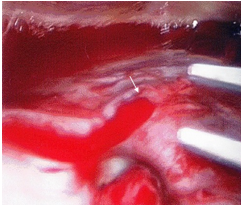
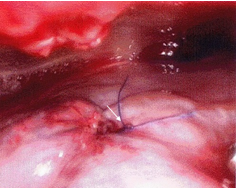
A chest tube (24 Fr.) was inserted to right pleural cavity and 1500cc bloody pleural effusion was drained out. The patient was then transferred to intensive care unit (ICU) for observation and intensive care. However, massive fresh blood was drained out from chest tube 12 hours after the RFA procedure. An emergent operation was performed with a thoracoscope inserted through the 10th intercostal space. Thoracoscopic view showed a vessel bleeding from the surface of diaphragm (Figure 4a).
Figure 4a: Blood oozing from diaphragm was demonstrated by direct thoracoscopic view.
Suture of the bleeding was immediately performed under thoracoscopic view. Immediate hemostasis was achieved. The patient’s condition was stabilized and discharged 4 days after operation (Figure 4b).
Figure 4b: Bleeding stopped after thoracoscopic suture ligation of the bleeder.
Follow-up chest X-ray film showed no more pleural effusion one month after discharge. The patient is survived till last visit at our hospital in November, 2015. CT scan showed well ablated tumor without new lesion.
DISCUSSION
The complication and mortality rates of RFA are low, making this procedure become a safe and feasible method in the treatment of hepatic malignancies [5]. The major complication rate of RFA was 2.0%-5.7% according to different reports [6]. It includes hemorrhage to peritoneum or pleural cavity, bile duct injury, bowel perforation, liver abscess, and tumor seeding [3-5].
Hemorrhage is the most common complication encountered in the procedure of percutaneous RFA [6]. Bleeding complications are more likely to occur in peritoneal site. In an early report of Mulier [7], they occurred in 0.7% of 3,670 procedures. Similar results were published by Livraghi [8](0.5% of 2,030 patients) and Curley [9] (0.9% of 608 patients) or in recent series by Goto [10] (0.7% of 4,133 patients). On the contrast, hemorrhage into the pleural space after percutaneous RFA was less common in comparison with intra-abdominal bleeding. According to the previous report, the incidence rate of hemothorax after RFA procedure was about 0.1%-0.3% [8,10]. The location of tumor and route of needle insertion were the major risk factors of hemothorax. According to the report of Goto [10], tumor located at S7 was the major risk factor of hemothorax after RFA. Hemothorax was usually thought due to intercostal artery injury during the insertion of the RFA needle. It was thought that an upward tilt during needle puncture was likely to injure the intercostal artery. In our present case, intercostal artery injury was also suspected before surgical intervention. However, after surgical intervention, diaphragm injury was proved by thoracoscopic view and treatment. Intercostal artery injury was not present in our case. Since the puncture through the pleura and diaphragm is inevitable for RFA of the tumor at this location, thermal coagulation of the needle tract by gradually withdrawal of the needle after completing the procedure, may reduce the risk of bleeding.
Treatment of hemothorax after RFA is usually conservative; the patient condition can usually be stabilized by fluid or blood infusion. Thoracocentesis is necessary if the respiratory distress still persists after the conservative treatment. Surgical intervention is required in patient with life threaten hemorrhage as in our case. To our knowledge, this is the first case report using thoracoscopic treatment of bleeding complication from diaphragm injury afer RFA.