The Relationship Between Fear of Falling, respectively, Fear of Choking and Emotional and Cognitive Functioning in Huntington
- 1. Department of Neurology, LUMC, The Netherlands
- 2. De Riethorst Stromenland, The Netherlands
- 3. Department of Primary and Community Care, Radboud University Medical Center, The Netherlands
- 4. Department of Health Services Research, Caphri – Care and Public Health Research Institute, Maastricht University, The Netherlands
- 5. Department of Family Medicine, Caphri – Care and Public Health Research Institute, Maastricht University, The Netherlands
Abstract
Context: Choking and accidental falls are common incidents in patients with Huntington’s disease (HD). It is not clear which emotional and cognitive factors contribute to the development of fear of choking (FoC) or fear of falling (FoF).
Objective: To explore the relationship between cognition, awareness and anxiety and experiencing FoC or FoF in HD, Parkinson’s disease (PD) and dementia. As the literature on HD is expected to be limited, the study population will be expanded by also looking at PD and dementia, both of which are neurodegenerative diseases that share symptoms and signs with HD.
Methods: A systematic review of English, German and Dutch articles using the electronic databases: MEDLINE, Embase, CINAHL and Psychinfo. Only studies describing the influence of cognition, awareness and anxiety on the outcome measures FoF and FoC in patients with HD, PD or dementia were included
Results: For HD, no reports were found related to the objective of the study and no studies on FoC were found for PD or dementia. The results of studies addressing FoF in PD and dementia were contradictory as far as the relationship with cognition (PD n=5; dementia n=8) and anxiety (PD n=2) was concerned. No study on FoF in relation to awareness was found in any patient group.
Conclusions: Although dysphagia and accidental falls are common symptoms of HD, PD and dementia, data on emotional and cognitive factors and their relationship with FoC and FoF are limited. Available data are inconsistent. Future research focusing specifically on these topics might lead to better insight into the relationship between FoC, FoF and cognitive, emotional and behavioral functioning of patients with these diseases. Better insight in these subjects could result in therapeutic options for patients or guidelines for caregivers, with regard to prevention and coping strategies, to improve quality of care.
Keywords
• Review
• Neurodegenerative diseases
• Accidental falls
• Choking
• Fear
Citation
Kalkers K, Derksen E, Neyens JCL, Schols JMGA, Roos RAC (2017) The Relationship Between Fear of Falling, respectively, Fear of Choking and Emotional and Cognitive Functioning in Huntington’s Disease, Parkinson’s Disease and Dementia: a Review. J Mem Disord Rehabil 2(1): 1006
ABBREVIATIONS
HD: Huntington’s Disease; PD: Parkinson’s Disease; Foc: Fear of Choking; Fof: Fear of Falling; MCI: Mild Cognitive Impairment
INTRODUCTION
Choking and accidental falls are common incidents in Huntington’s disease (HD); both can have major consequences for patients [1]. Better understanding of this process could lead to prevention, better treatment and better care. As the available literature on these problems in patients with HD is expected to be limited, the study population will be expanded by also looking at patients with Parkinson’s disease (PD) and dementia, both of which are neurodegenerative diseases that share signs and symptoms with HD. As PD and dementia share several clinical characteristics with HD and there are, in general, more studies addressing these diseases as a subject, they might offer some reference points for HD on the problems addressed in this article..
HD is a progressive neurodegenerative autosomal dominant disease caused by a mutant protein, Huntingtin, and resulting from an expanded CAG repeat on the short arm of chromosome 4 [2]. The main clinical characteristics of the disease are motor symptoms, cognitive dysfunction and psychiatric and behavioral symptoms [2]. PD is a progressive neurodegenerative disorder resulting from a combination of genetic and environmental factors, leading to a clinical picture of classical motor and non-motor symptoms [3]. Dementia is a clinical diagnosis that requires functional dependence on the basis of cognitive decline, caused by a variety of underlying pathophysiological processes [4]. These disorders have motor signs in common; cognitive dysfunction and psychiatric and behavioral symptoms [2-4].
The combination of symptoms and signs leads to dysphagia in many patients with HD, PD and dementia [5]. Little is, however, known about the frequency and the development of dysphagia during these diseases [6,7]. Dysphagia can have serious consequences leading to acute respiratory distress, pneumonia, and subsequent death [5,7,8] and might, therefore, give rise to FoC [6].
The second important consequence of the combination of symptoms and signs in HD, PD and dementia is falling [9-11]. Falls can lead to hospitalization, early admission to a nursing home or even death [12]. In addition to physical injuries, falls can result in FoF and avoiding activities [13,14]. Paradoxically, FoF and consequently, avoiding activities are factors predictive of future falls in both fallers and non-fallers [13,15]. Activity restriction increases loss of muscle strength and postural control [16]. There is, however, some evidence that patients with HD experience less FoF compared to other patient groups, such as PD [9,17].
Anxiety arises when experience with or thinking about danger occurs. Anxiety is often a useful emotion leading to preventive actions [18]. Experiencing less fear, in general, may, therefore, influence the ability to act safely. In HD, reduced fear responses are reported [19,20]. Unawareness might be an explanation for experiencing less fear. In HD literature, the terms unawareness, self-awareness, anosognosia, insight and denial are often used interchangeably [21]. The following definition for unawareness is often used: The manifestations of disease and the consequences are obvious to and can be documented by an observer, but the individual underestimates or does not report experiencing symptoms or does not notice these changes or the impact [21]. Reduced self-awareness is described as a possible reason for falls in the elderly, whereby they take greater risks [22]. Unawareness is differentiated across different domains, e.g. physical and mental changes, and can appear at all stages of HD [23]. Presumably a combination of cognitive, physiological and psychological factors contributes to the loss of awareness of deficits in HD [23]. Also cognitive factors such as awareness of task demands, the ability to comprehend information [24] and the ability to evaluate possible consequences of behavior [9] can influence the extent to which fear is experienced.
Dysphagia and falls and related fear may be important negative consequences of the combination of symptoms and signs in HD, PD and dementia. By means of a literature review, this study aims to explore whether the emotional and cognitive factors, anxiety, awareness and cognition, are related to experiencing FoC or FoF in HD, PD and dementia.
METHODS
The search for the systematic review was conducted according to the PRISMA Statement [25,26].
Search Strategy
Literature searches were performed using the electronic databases MEDLINE (1966-December 2016), Embase (1974-December 2016), CINAHL (1982-December 2016) and Psychinfo (1987-December 2016). The last search was run on December 15 2016. MeSH terms (Medline), Thesaurus terms (EMBASE, PsycINFO, CINAHL) and free text words were used for the search. Search terms included: Huntington’s disease, Parkinson’s disease, dementia, elderly, aged, cognitive impairment, accidental falls, deglutition disorders, dysphagia, swallowing disorders, fear, anxiety and awareness. See appendix 1 for the Medline search strategy. In addition we manually searched reference lists of articles already included in the systematic review.
Study selection
Two reviewers (KK and ED) independently assessed the eligibility of studies on the following pre-established criteria:
- Types of studies: Observational studies, case-studies, and (systematic) reviews were included. Intervention studies, studies involving assessment of screening tools for fear of falling, editorials, comments and letters were excluded as well as study protocols and conference abstracts. No publication date restrictions were imposed. Searches were restricted to studies written in English, German or Dutch.
- Types of participants: Patients of any age with the diagnosis Huntington’s disease, Parkinson’s disease or dementia were included. Because dementia can be described in a different, revealing way, elderly subjects with cognitive impairment, global cognitive impairment or mild cognitive impairment were also considered. Animal studies were excluded.
- Types of outcome measure: Studies describing the influence of cognition, awareness, and anxiety on the outcome measures FoC and FoF were included. For FoF, all concepts and measures mentioned in the systematic review by Jørstad [27] were considered. There is no such concept for FoC.
The first reviewer (KK) checked all titles and abstracts; the second reviewer (ED) screened a random selection of 85%. Initially all studies concerning falls and dysphagia or swallowing problems were included, because FoC and FoF may be secondary outcome measures. This also applies to the factors cognition, awareness, or anxiety. Subsequently the reviewers applied the inclusion criteria to all full-text articles that remained after the initial screening. The first reviewer assessed the eligibility of all studies; separately, the second reviewer checked 10% of these references using the same criteria. Because the results were consistent with the results of the first reviewer, other full-text articles were assessed by the first reviewer only. In all steps of the study selection process, disagreements between the two reviewers were discussed until consensus was reached.
Data Extraction
The following data were extracted by the first reviewer (KK) from the included studies: 1) study design; 2) research question; 3) characteristics of study participants (including number of participants, age and diagnosis); 4) main results with regard to the association between FoC or FoF and the factors cognition, awareness and anxiety.
Risk of Bias in Individual Studies
There are no gold standards for evaluating the methodological quality of observational research [28]. To appraise the selected studies, a checklist for etiological research [29] was used. Each article was rated by one author (KK), allocating a maximum of one point if a criterion was fulfilled (appendix 2); a total score was calculated and displayed in table 1 and 2.
|
Table 1: Studies of the relation between cognition, awareness and/or anxiety and experiencing fear of falling in Parkinson’s disease. |
|||||
|
Reference |
Design |
Objective |
Participants |
Main results |
Quality score |
|
#1 Brozova et al., 2009 (40) |
Cross sectional |
Assessment of the influence of gait disorders on quality of life in PD |
491 PD patients of a Movement Disorders Center, mean (SD) age 66.7 (9.4) years |
FOF (8-QGD) had a high association to the cognition sub score of PDQ-39. (R 0.34 (p=<0.001) |
0.5 |
|
#2 Jonasson et al., 2015 (30) |
Secondary analysis of a prospective longitudinal cohort study |
To identify explanatory factors of concerns about falling in people with PD by focusing on personal and environmental factors as well as PD-related disabilities. |
241 persons with PD (61% male), median age 70 years |
Anxiety (NMSQuest item17) and cognition (MOCA) did not significantly explain concerns about falling (FES-I) in a multivariate model |
4 |
|
#3 Lindholm et al., 2014 (39) |
Cross sectional study |
To investigate potential contributing factors to FoF among people with idiopathic PD |
104 people with PD receiving care at a university hospital, mean (SD) age 68 (9.7) years |
Cognition (MMSE) showed highly significant (p=0.027) bivariate relationships with FOF (FES-S), but was not independently associated with FOF when controlling for other independent variables. |
5 |
|
#4 Mak et al., 2014 (41) |
Prospective cohort study |
To examine whether impairment in executive function independently predicts recurrent falls in people with PD |
170 community dwelling individuals with PD, mean (SD) age 62.6 (7.8) years |
No association was found between executive function (MDRS-IP) and FoF (ABC) scores for RFs (p>0.05), whereas the 2 scores were significantly correlated for non-RFs (r=0.403 p<0.001) |
3.5 |
|
#5 Rahman et al., 2011 (31) |
Cross sectional study |
To identify the characteristics of FoF in PD and assess its impact on QoL |
130 individuals with PD (84% male) mean (SD) age 66.7 (8.5) years |
Anxiety (BAI) was a significant predictor for activity avoidance (SAFFE), but not for FoF (FES) and the perceived consequences of falling (CoF) |
3.5 |
|
#6 Thomas et al., 2010 (38) |
Cross sectional study |
To investigate the relationship between fear of falling and fall frequency among patients with idiopathic PD |
102 individuals with idiopathic PD, mean age 70.8 years |
FoF (FES) was negatively correlated with cognition (MMSE), r=-0.41, p<0.001 |
3 |
|
PD: Parkinson’s Disease; FoF: Fear of Falling; PDQ-39: Parkinson’s Disease Questionnaire-39; NMSQuest: Non-motor Symptoms Questionnaire; MOCA: Montreal Cognitive Assessment; FES-I: Falls Efficacy Scale-International; FES-S: Falls Efficacy Scale-Swedish version; MDRS-IP: Mattis Dementia Rating Scale-subset Initiation/perseveration; ABC: Activities-specific Balance Confidence Scale; RF: Recurrent Faller; QoL: Quality of Life; BAI: Beck Anxiety Inventory; SAFFE: Survey of activities and fear of falling in the elderly: FES: Falls Efficacy Scale; CoF: Consequences of Falling |
|||||
|
Table 2: Studies of the relation between cognition awareness and/or anxiety and experiencing fear of falling in dementia. |
|||||
|
Reference |
Design |
Objective |
Participants |
Main results |
Quality score |
|
#7 de Melo Borges et al., 2014 (55) |
Case-control study |
To evaluate the occurrence of previous falls, FoF, and falls self-efficacy in older adults with MCI and mild AD. |
104 community dwelling elderly, 60 years and older AD n=26 MCI n=42 Cognitively healthy n=36 |
Older adults with MCI more often reported FoF (single question yes/no) than patients with AD (respectively 74% and 31%, P ≤ .002) and scored higher on the FES-I (29.7 and 23.8, respectively, P ≤ .01). FoF: MCI>Cognitively healthy>AD FES-I: MCI>Cognitively healthy>AD |
4 |
|
#8 Delbaere et al., 2012 (47) |
Prospective cohort study |
To investigate whether MCI is associated with falls in older people |
419 people age 70-90 years, mean (SD) age 77.8 (4.6) years |
No significant difference between people with and without MCI with regard to FOF (FES-I), with a mean (SD) of 22,3 (5,9) and 23.6 (8.0), respectively |
3 |
|
#9 Hauer et al., 2003 (48) |
Experimental three group design |
To investigate the influence of dual tasks, cognitive strategies, and FoF on postural control in geriatric patients with or without cognitive impairment and with a history of falls resulting in injury |
40 geriatric patients 70 years and older with a recent history of serious falls (1) with and (2) without cognitive impairment and 20 young healthy controls |
No significant difference between patient groups with (MMSE score 17-23) and without (MMSE score >23) cognitive impairments with regard to FoF (single question with a score ranging from 1 to 4). Mean (SD) 2.1 (0.9) for both groups |
2.5 |
|
#10 Otaki et al., 2015 (49) |
Cross sectional study |
To clarify reliability of memories of falling in elderly patients with dementia |
62 elderly patients in long term care diagnosed with dementia, mean age (SD) 82.9 (7.8) |
No correlative relationship between cognition (MMSE) en FoF (VAS and FPRS) |
2 |
|
#11 Shirooka et al., 2016 (59) |
Cross sectional study |
To explore the association between cognitive function and FoF in frail/non-frail community dwelling older adults |
483 community dwelling elderly, 65 years and older mean (SD) age 73.3 (5.1) |
Cognitive impairment (MMSE ≤26) was not significantly associated with FoF (single question yes/no) in the sample as a whole nor in the non-frail group. However, in the frail group, the presence of cognitive impairment was independently associated with the absence of FoF (OR 0.04, 95% CI 0.00–0.50, P = 0.012) |
3.5 |
|
#12 Uemura et al., 2012 (56) |
Cross sectional study |
To determine which cognitive function is related with the prevalence of FoF in older adults |
101 older adults, mean age 75.1 years |
Memory (WMS-LM 1) is independently associated with FoF, single question with a score ranging from 1 to 4 (OR 1.20 95% C.I. 1.07-1.35; p=0.002). Lower prevalence of FoF is associated with memory decline among older adults. There was no association with general cognitive function, processing speed or executive function. |
3.5 |
|
#13 Uemura et al., 2014 (58) |
Cross-sectional study |
To determine whether the status of cognitive impairment affects the prevalence of FoFin community dwelling older adults |
4474 community dwelling older adults 65 and older Classified into 3 groups: cognitively healthy, MCI, GCI |
The prevalence of FoF (single question with a score ranging from 1 to 4) was differed significantly per group (p<0.001; healthy: 43.6%, MCI: 50.6%, GCI: 40.6%). Participants with MCI showed the highest prevalence of FoF, while those with GCI showed the lowest prevalence of FoF although they had the lowest physical function comparing with the other groups (p < 0.001). |
3 |
|
#14 Uemura et al., 2015 (57) |
Prospective cohort study |
To determine whether MCI affects the development FoF in older adults |
1700 community dwelling adults aged 65 years or older without FoF at baseline |
MCI was independently associated with FoF (single question with a score ranging from 1 to 4) development |
3 |
|
FoF: Fear of Falling; AD: Alzheimer Disease; MCI: Mild Cognitive Impairment; FES-I: Falls Efficacy Scale-International; MMSE: Mini-Mental State Examination; VAS: Visual Analogue Scale; FPRS: Faces Pain Rating Scale; WMS-LM: Wechsler Memory Scale-Logical Memory; GCI: Global Cognitive Impairment |
|||||
RESULTS
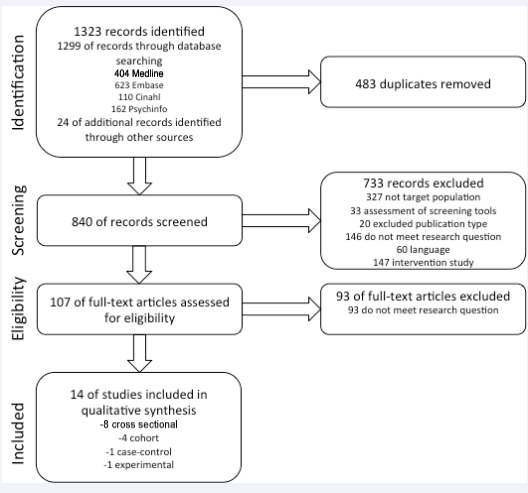
The electronic search provided 1299 studies. 404 in MEDLINE, 623 in Embase, 110 in CINAHL and 162 in Psychinfo. An additional 24 articles were identified from reference lists. Removing duplicates resulted in 840 articles. From this list, 725 records were excluded during the screening process of title and abstract. Of the remaining 115 records, 101 were excluded after assessment of the full-text. The different steps of this search are summarized in figure 1.
Figure 1: Flow chart of literature search.
No articles were found for HD. The main characteristics of the remaining studies are summarized for PD (n=6) in table 1 and for dementia (n=8) in table 2.
Fear of Choking and Fear of Falling related to anxiety, awareness and cognition in Huntington’s disease
For patients with HD, no reports were found related to the objective of this study.
Fear of Choking and Fear of Falling related to anxiety, awareness and cognition in Parkinson’s disease
No studies concerning FoC related to anxiety, awareness or cognition were found for PD.
Six studies focused on FoF in relation to anxiety and cognition; two of them [30,31], considered the relationship between FoF and anxiety. In one of these [30], the score on item 17 from the Non-motor Symptoms questionnaire [32], about feeling anxious, frightened or panicky, did not significantly explain concerns about falling. Concerns about falling during physical and social activities were measured with the Falls Efficacy Scale International (FES-I [33]). In the second study [31], the score on Beck’s Anxiety Inventory (BAI [34]), a 21-item self-report inventory for measuring the severity of anxiety, was a significant predictor for activity avoidance measured using the Survey of Activities and Fear of Falling in the Elderly [35]. In the same study confidence about avoiding a fall during physical and social activities as measured with the Falls Efficacy Scale (FES [36]) and four types of feared consequences of falling measured with the Consequences of Falling scale [37], were not significantly predicted by the score on the BAI.
Five studies [30,38-41] examined the relationship between cognition and experiencing FoF. Two of them [30,39] found no relationship. In the first study [30], the score on the Montreal Cognitive Assessment [42], a brief cognitive screening tool, did not significantly explain concerns about falling measured with the FES-I. Although there was a significant relationship between the cognition score of the Mini Mental State Examination (MMSE [43]) and FoF measured with the FES, there was no independent association when controlling for other independent variables [39]. Two studies did find a relationship between cognition and FoF [38, 40]. In the first [40], a question about limitations of activities due to FoF from the Questionnaire of Gait Disorders (8- QGD [40]) showed an association with the cognition subscore of the PD questionnaire for assessment of health-related quality of life (PDQ-39, [44]), meaning that more cognitive difficulties were associated with more limitations due to fear of falling. Higher MMSE cognition scores were associated with lower FES scores in the other study [38], meaning that better cognitive functioning is associated with higher confidence about avoiding a fall during activities. Finally, in one study [41], there was an association between executive function and FoF for non-recurrent fallers, but not for recurrent fallers. Non-recurrent fallers with a higher score, indicating better executive function, had more balance confidence. Executive function was assessed with a neuropsychological instrument, the Mattis Dementia Rating Scale Initiation/Perseveration subtest [45]. For FoF, patients were asked to rate their self-perceived balance confidence when performing daily activities, using the Activities-specific Balance Confidence Scale [46]. No studies concerning the relation between FoF and awareness were found for patients with PD.
Fear of Choking and Fear of Falling related to anxiety, awareness and cognition in dementia
No studies concerning FoC related to anxiety, awareness and cognition were found for patients with dementia. Nor were any studies concerning the relation between FoF and anxiety and awareness found for patients with dementia.
Eight studies focused on FoF related to cognition in dementia. In three of these [47-49], no relation was found between cognition and FoF. There was no significant difference between participants with and without Mild Cognitive Impairment (MCI, [50,51]) on the FES-I score [47]. There were no significant differences between people with a score above or below 23 on the MMSE with regard to a single question on FoF [48]. Finally, there was no correlative relationship between the MMSE score and a Visual Analogue Scale (VAS) and the Faces Pain Rating Scale (FPRS) regarding FoF [49]. The VAS [52,53] involves placing a mark above a 10-cm straight line to indicate the extent of FoF. The FPRS [54] uses six images of facial expressions to indicate FoF.
Five studies [55-59] found a relation between cognition and FoF. All used the single question: ‘are you afraid of falling?’ with two [yes/no] [55,59] or four (a score ranging from 1 to 4) possible answers to measure FoF. One study [55] combined this question with the FES-I.
In another of these studies [56], a lower prevalence of FoF was associated with memory decline among older adults. There was no association with general cognitive function, processing speed and executive function. For these cognitive domains, the following assessments were used: Alzheimer’s Disease Assessment Scale [60] and MMSE [43] for general cognitive function; Wechsler Memory Scale subtest Logical Memory-I [61] and the three-word recall test from the MMSE for memory function; Wechsler Adult Intelligence Scale (WAIS) subtest digit symbol coding [62] for processing speed; Trailmaking test part B [63], WAIS subtest Digit span forward and backward and letter and category fluency [64] for executive function.
In three studies [55,57,58], participants with MCI reported FoF more often than healthy controls. In addition, 2 of these studies [55,58] indicated that with an increase in cognitive impairment, such as in patients with Alzheimer’s disease or Global Cognitive Impairment, there is less FoF compared to MCI and healthy controls. Finally, the absence of FoF is associated with cognitive impairment in frail elderly but not in non-frail older adults [59].
DISCUSSION & CONCLUSION
Choking and accidental falls are common adverse events of Huntington’s disease. Even though these incidents may have serious consequences, research into the emotional consequences is limited. FoC and FoF would seem to be an area of HD research, which has so far been neglected. Their relation with cognitive and emotional functioning is totally absent. As PD and dementia share several clinical characteristics with HD, they might offer some reference points. However, research into FoC in dementia and Parkinson’s disease is also lacking. Most articles identified for this review concern the relationship between FoF and cognitive functioning in both PD and dementia. The relationship between FoF and anxiety has been studied to a lesser extent. Although in fall literature, lack of awareness is frequently mentioned as a fall risk [22,55], there are no studies, which address this relationship in these three diseases.
The studies reported in this review showed varying results: although anxiety in PD was not associated with most measures for FoF, activity avoidance was predicted by anxiety [30,31]. In addition, in PD, less FoF was associated with better scores in cognition measures [38,40], but other studies showed no association between FoF and cognitive functioning [30,39]. In one study [41] there was an association between executive function and FoF for non-recurrent fallers, but not for recurrent fallers. In the case of dementia, some studies found no association between different measures for FoF and cognitive functioning [47-49]. In others, both a lower and higher prevalence of FoF was associated with increased cognitive impairment [56,59,65]. Some studies indicate that the relation between FoF and cognition depends on the severity of the cognitive problems [55,58]. Fall history and frailty also appear to be risk factors for FoF in PD and dementia, respectively.
Comparisons across studies are difficult because of the different diseases, differences in disease stages, study designs and measures applied. With regard to the latter, a review of fall-related psychological outcome measures [27] reveals there are many different measures related to FoF. In the studies identified for this review, instruments based on different constructs and variants of the same instrument based on the same construct, were used. Different methods were used for the measurement of cognition and anxiety. As for different diseases and disease stage, the results of two studies [55,58] indicate that the relation between FoF and cognition depends on the severity of the cognitive problems. Little research has, however, been conducted into FoF in people with cognitive problems because of a lack of validated measures and expectation of methodological problems for this population [65].
There are some limitations in this review: only articles in English, German and Dutch were included. Moreover, because of our broad definition of dementia, the articles concerning dementia were highly heterogeneous. By including this group, however, it was possible to study the relationship between FoF and cognitive functioning. Finally, the limited number of included studies makes it difficult to draw consistent conclusions.
This review shows that there are very few data on FoC and FoF and their relation with cognition, awareness and anxiety in HD, PD and dementia and they often lead to inconsistent results. Future research on dysphagia, accidental falls, FoC and FoF from the patient’s and caregiver’s perspective, as well as the impact of cognition, anxiety and awareness of dysphagia and fall risk on FoC and FoF, respectively, might improve insight into the cognitive, emotional and behavioral functioning of patients with these diseases. It is expected that cognitive impairment (e.g. on executive functioning and working memory), lack of awareness in self-functioning and a reduced ability to experience anxiety can lead to less FoC and FoF. In these patients, interventions will mainly focus on the patients’ environment rather than on the patients themselves. Better insight in these issues could lead to therapeutic options for patients, or guidelines for caregivers regarding prevention and coping strategies, with the aim of improving quality of care.
ACKNOWLEDGEMENTS
This research was sponsored by ‘CZ fonds’.
REFERENCES
1. Roos RA. Huntington’s disease: a clinical review. Orphanet J Rare Dis. 2010; 5: 40.
2. Walker FO. Huntington’s disease. Lancet. 2007; 369: 218-228.
3. Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015; 386: 896-912.
4. Cunningham EL, McGuinness B, Herron B, Passmore AP. Dementia. Ulster Med J. 2015; 84: 79-87.
6. Heemskerk AW, Roos RA. Dysphagia in Huntington’s disease: a review. Dysphagia. 2011; 26: 62-66.
7. Suttrup I, Warnecke T. Dysphagia in Parkinson’s Disease. Dysphagia. 2016; 31: 24-32.
11. Shaw FE. Falls in cognitive impairment and dementia. Clin Geriatr Med. 2002; 18: 159-173.
51. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004; 256: 183-194.
52. Aitken RC. Measurement of feelings using visual analogue scales. Proc R Soc Med. 1969; 62: 989-993.
61. Wechsler D, Stone CP. Wechsler memory scale-revised: Psychological Corporation; 1987.
62. Scale WDWAI. (WAIS-III). San Antonio, TX: The Psychological Corporation. 1997.