Association between Symptomatic Uterine Fibroids and Venous Thromboembolism Risk: A Correlational Descriptive Study in Riyadh, Saudi Arabia
- 1. Imam Abdulrahman Alfaisal Hospital, Saudi Arabia
ABSTRACT
Background: Many women develop uterine fibroids, which are benign but can cause discomfort such as pelvic pain, pressure, and excessive menstrual bleeding. While they are not usually a major health concern, some studies indicate that larger fibroids could contribute to an increased risk of venous thromboembolism (VTE), including DVT and PE. VTE is often underdiagnosed, particularly in women with conditions like uterine fibroids, but it’s still uncertain how much they contribute to the VTE risk. One possible explanation is that larger fibroids put pressure on major veins, such as the iliac veins or inferior vena cava, slowing blood flow and making clots more likely. The connection between symptomatic fibroids and VTE is something that needs more attention to improve patient care. Even though fibroids are quite common, there isn’t much research on how often VTE occurs in these patients, leaving an important gap in medical science.
Objectives: This study examines the occurrence of venous thromboembolism (VTE) in women with symptomatic uterine fibroids and its correlation with VTE risk. It also aims to explore strategies for managing and preventing VTE in this patient population.
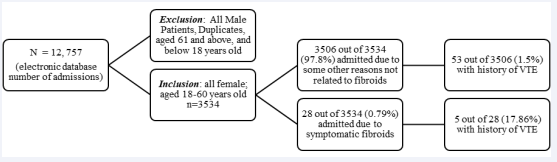
Methods: This study, conducted between January 2023 and May 2024 in Riyadh, Saudi Arabia, uses a correlational descriptive approach to explore the risk of VTE in women with symptomatic uterine fibroids. Researchers reviewed medical records from an electronic healthcare database, a VTE dashboard, and PACS, focusing on obstetric, medical, and surgical patients to assess VTE risk and the effectiveness of prophylaxis. Data from 3,534 female patients aged 18 to 60—including 28 diagnosed with symptomatic fibroids—were analyzed using SPSS, applying descriptive statistics and a two-tailed Pearson correlation test.
Results: A total of 12,757 admissions were recorded, with 3,534 female patients aged 18 to 60 meeting the study criteria. Among them, 1.5% (n = 53) of women had a history of VTE, including one case of hospital-acquired pulmonary embolism, 28 (0.79%) were admitted with symptomatic uterine fibroids, and 5 (17.86%) had a history of VTE. Statistical analysis revealed a significant correlation (r = 0.115, p < 0.001) between symptomatic uterine fibroids and VTE history, suggesting an increased risk in this group. Risk assessment showed that most fibroid patients fell into moderate to high-risk categories for VTE, and preventive interventions, including pharmacological and mechanical prophylaxis, were administered accordingly. Surgical management was required in 85.71% of fibroid cases, with no recorded morbidity or mortality.
Conclusions: Women with symptomatic uterine fibroids seem to be more vulnerable to VTE, especially when dealing with larger or multiple fibroids as findings show a significant correlation between fibroids and VTE history. This emphasizes the importance of early detection, thorough VTE assessment and prophylactic measures for this population, advocating for greater awareness and improved management protocols.
KEYWORDS
- Fibroids
- Venous thromboembolism
- Deep vein thrombosis
- Pulmonary embolism
- VTE prophylaxis
CITATION
Saab SM, Algarni AM, Saab MA, Daowd RAA, Almograbi MA, et al. (2025) Association between Symptomatic Uterine Fibroids and Venous Thromboembolism Risk: A Correlational Descriptive Study in Riyadh, Saudi Arabia. J Prev Med Healthc 7(2): 1038.
INTRODUCTION
Background of the Study
Uterine fibroids, or leiomyomas, are common benign growths in the uterus. They consist of smooth muscle cells and fibroblasts, along with a large amount of fibrous tissue, which contributes to their formation and growth [1]. According to Stewart [2], fibroids are especially common in women of reproductive age and can lead to heavy menstrual bleeding or symptoms caused by their size and location. Although hysterectomy is a highly effective treatment, there are several uterus-preserving options that should be considered and discussed with patients. While various factors are thought to play a role in fibroid development, their exact cause is still unknown. Most women with fibroids experience symptoms such as changes in their menstrual cycle or a sensation of pressure in the pelvic area [3].
Uterine fibroids are among the most common yet under- researched conditions affecting women of different ages. Though the majority of women with fibroids experience no symptoms, approximately 30% develop severe symptoms that require medical intervention. These symptoms may include abnormal uterine bleeding, anemia, pelvic pain and pressure, back pain, frequent urination, constipation, or infertility [4]. Fibroids may also be associated with more serious health concerns, including a potential link to venous thromboembolism (VTE). According to Onwuzo et al. [5], VTE is a common condition and a leading cause of preventable deaths in developed countries. It refers to the blood clots that form in the veins, and includes deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT occurs when a clot develops in a deep vein, typically in the lower leg, thigh, or pelvis, though it can also affect the arms. If part of the clot dislodges and travels to the lungs, it can lead to PE, a potentially life-threatening condition [6].
Prior studies demonstrated that there seems to be a connection between uterine fibroids and acute venous thromboembolism (VTE). Interestingly, rare case studies have pointed out the association between large uterine fibroids, acute deep venous thrombosis (DVT), and acute pulmonary embolism (PE). The association between uterine fibroids and VTE may be due to the way large fibroids put pressure on nearby veins, which can slow blood flow and cause venous stasis in the pelvis and lower limbs [7]. Shiota et al. [8], conducted a study to examine how preoperative DVT rates might be influenced by three risk factors including age, obesity, and uterine size or weight. Findings found that there was no statistical difference in the DVT rate for patients stratified by age or BMI. By contrast, the rate of DVT was significantly higher for patients with uterine weights of 1,000 gm or more compared with weights below 1,000 gm. Similarly Brewer et al. [9], noted that while uterine fibroids are benign and rarely cause complications, exceptionally large fibroids can compress the iliac veins, increasing the risk of venous thrombosis and, in severe cases, limb-threatening phlegmasia. Although independent risk factors for VTE and predictors of recurrence have been identified—and effective primary and secondary prophylaxis is available— the overall incidence of VTE remains steady or may even be rising [10].
Despite these findings, there is still a need for research specifically focusing on the correlation between symptomatic fibroids and venous thromboembolism and exploring some major risk factors for patients with fibroids developing VTE. Thus, by conducting this study in Riyadh, Saudi Arabia, this study aims to provide more information on this topic and contribute to better health outcomes for women affected by symptomatic uterine fibroids.
Aim of the Study
This study aims to evaluate the occurrence of Venous thromboembolism (VTE) in women with symptomatic uterine fibroids and determine its correlation between VTE risk among patients at Imam Abdulrahman Alfaisal Hospital from January 2023 to May 2024. It also seeks to explore whether the size of fibroids affects this risk. Lastly, this study aims to manage and prevent VTE in women with symptomatic uterine fibroids.
MATERIALS AND METHODS
Study Setting
A correlational descriptive study was used to identify the risk of VTE for women with symptomatic uterine fibroids who needed further management. An electronic healthcare database, a VTE electronic dashboard, and a picture archiving and communication system (PACS) were utilized to review the patient’s medical records and determine the VTE risks for obstetrics, medical, and surgical patients from January 2023 to May 2024.
Study Setting
The study was conducted at Imam Abdulrahman Al Faisal Hospital, a secondary hospital in Riyadh, Saudi Arabia to ensure that the research is performed in a healthcare setting where VTE risk assessment, prophylaxis protocols and surgical procedures for uterine fibroids are implemented.
Study Participants
Inclusion criteria include all female patients aged 18 to 60 receiving care from any specialty at IAFH admitted from January 2023 to May 2024. Patients were categorized into two groups – patients hospitalized with symptoms and complaints unrelated to uterine fibroids and patients with symptomatic uterine fibroids.Exclusion criteria were all male patients, female patients under 18 or over 60 years old, and duplicate records.
Statistical Analysis
All adult (≥ 18 years) patients were assessed using the Adult In-Patient Venous Thromboembolism (VTE) Assessment and Prophylaxis during admission and repeated if patient’s condition changed. The data was analyzed using SPSS software to determine descriptive statistics and correlations between variables. Descriptive statistics, including frequency distribution, percentage, mean, median and standard deviation were used to summarize the characteristics of the participants including age, VTE history, symptomatic fibroid presence, and risk factor scores. Two-tailed Pearson correlation test was conducted to show the correlation between symptomatic fibroids and VTE history. The correlation between symptomatic fibroids and a history of VTE was assessed using a two-tailed Pearson correlation test. The correlation coefficient (r = 0.115, p < 0.001) indicated that it is a statistically significant positive correlation which means that symptomatic fibroids are associated with VTE history.
RESULTS
A total of 12,757 admissions were recorded in the electronic database of Imam Abdulrahman Al Faisal Hospital from January 2023 to May 2024. Male patients, duplicate records, and patients younger than 18 or older than 60 were excluded (N=9,223). The study included all female patients between the ages of 18 and 60 (N=3,534). Out of 3534 admitted female patients who met the inclusion criteria, 3506 (97.8%) were being admitted due to some other reasons and treated for non-fibroid related problems. Of those patients, 53 (1.5%) had a prior history of VTE and one of the 53 developed hospitalacquired pulmonary embolism. Additionally, 28 patients (0.79%) were admitted with symptomatic uterine fibroids and required further management, including surgical intervention. Among them, 5 (17.86%) had a history of VTE; four were receiving therapeutic doses of anticoagulants, and one has a history of hospital-acquired VTE. Table 1 presents a descriptive analysis of the 3,534 valid cases for all the variables studied.
Table 1: Descriptive analysis of the participants.
|
|
N |
Minimum |
Maximum |
Mean |
Std. Deviation |
|
AGE |
3534 |
18 |
60 |
36.27 |
10.442 |
|
VTE History |
3534 |
1 |
2 |
1.98 |
.126 |
|
Symptomatic Fibroid |
3534 |
1 |
2 |
1.99 |
.089 |
|
Risk Factor Score |
3534 |
1 |
8 |
4.21 |
2.432 |
|
Valid N (listwise) |
3534 |
|
|
|
|
The cases’ ages ranged from 18 to 60 years, with an average age of 36.27 years and a standard deviation of 10.442 which indicates a moderate variability in patients’ age. In VTE history, the mean score was 1.98 in which 1 = Yes 2 = No, with a narrow standard deviation of 0.126, suggesting that most participants had no history of VTE as the VTE score was close to the mean. Similarly, symptomatic fibroids were also coded as 1 = Yes 2 = No, with a mean score of 1.99 and a standard deviation of 0.089 which means that most participants did not have symptomatic uterine fibroids. Lastly, the risk factor score, which categorizes patients based on their level of VTE risk, ranged from 1 to 8, with a mean and standard deviation of 4.21 and 2.432 respectively. These cases were initially screened for VTE assessment and prophylaxis upon admission and were reassessed if their condition changed. The total number of inclusion cases from the database was 3534. Table 2 presents the risk categorization of these patients across medical, surgical and obstetric cases as well as the cases associated with symptomatic uterine fibroids. Medical and surgical cases were categorized as <1 (low risk), 2 (moderate risk), 3-4 (high risk), and ≥5 (highest risk), while obstetric cases were categorized as low, intermediate, and high risk.
Table 2: Risk Categorization for Medical, Surgical, Obstetric, and Symptomatic Fibroid Cases (N=3534).
|
Risk Category |
N |
VTE history |
HA- VTE |
|
Medical and surgical cases |
|
|
|
|
< 1 (Low risk) |
770 |
0 |
0 |
|
2 (Moderate risk) |
576 |
0 |
0 |
|
3-4 (High risk) |
519 |
7 |
1 |
|
≥5 (Highest risk) |
247 |
38 |
0 |
|
Obstetric cases |
|
|
|
|
Low risk |
214 |
0 |
0 |
|
Intermediate risk |
1178 |
7 |
0 |
|
High risk |
3 |
0 |
0 |
|
Total |
3506 |
52 |
1 |
|
Symptomatic fibroid cases |
28 |
4 |
1 |
|
Grand Total |
3534 |
58 |
|
In the medical and surgical cases, 770 patients (21.78%) were identified as low risk and 576 (16.29%) were considered moderate risk, with no VTE history. In the high-risk category, 519 (14.68%) were classified with 7 having a history of VTE and were receiving therapeutic doses of enoxaparin, while 1 (one) developed hospital-acquired pulmonary embolism and 511 cases were identified with no history of VTE. Finally, within the medical and surgical cases, 247 (6.99%) were categorized as highest risk, with 38 having a history of VTE and 209 without a history of VTE. In obstetric cases, out of 3534 cases, 214 (6.1%) were categorized as low risk with no history of VTE, 1178 (33.3%) were classified as intermediate risk, with 7 having a history of VTE and 1171 without, and finally, 3 cases (0.08%) were considered high risk, and none had a history of VTE or developed HA-VTE. Lastly, 28 patients were admitted due to symptomatic fibroids where four had a history of VTE, and one developed HA-VTE. Findings showed that the highest number of VTE cases was observed in the highest-risk category under the medical and surgical cases. Additionally, patients with symptomatic fibroids showed a slightly higher proportion of VTE history and HA-VTE.
Pearson’s correlation analysis was used to determine the association between symptomatic uterine fibroids and VTE history. The results [Table 3], show a significant positive correlation (r = 0.115, p < 0.001) between the presence of symptomatic uterine fibroids and a history of VTE at the 0.01 level (2-tailed). This suggests that symptomatic uterine fibroids may contribute to an increased risk of VTE; Therefore, there is a need for careful monitoring and preventive measures for patients with fibroids, particularly those with additional risk factors for VTE. A total of 28 cases (0.79%) of symptomatic uterine fibroids were identified among 3534 participants, who were stratified according to their VTE risk levels.
Table 3: Correlation between symptomatic fibroid and VTE.
|
|
Symptomatic Fibroid |
VTE History |
|
|
Symptomatic Fibroid |
Pearson Correlation |
Yes |
.115** |
|
|
Sig. (2-tailed) |
|
<.001 |
|
|
N |
3534 |
3534 |
|
VTE History |
Pearson Correlation |
.115** |
1 |
|
|
Sig. (2-tailed) |
<.001 |
|
|
|
N |
3534 |
3534 |
Five patients (17.86%), were classified as low risk, with 1 having a history of VTE and was on a therapeutic dose of anticoagulants. Six patients (21.43%) fell into the moderate-risk category, including 1 with a history of VTE. The largest group, 14 patients (50%), were classified as high risk, though none had a prior history of VTE. Finally, 3 patients (10.71%) were categorized as highest risk, including 1 with hospital-acquired VTE. According to the World Health Organization (WHO), hospital-acquired venous thromboembolism (HA-VTE) is a leading cause of death and disability, particularly in low- and middle-income countries. It results in more fatalities and complications than nosocomial pneumonia or adverse drug events. This finding is consistent with the study conducted by Huang et al. [11], which found a strong association between uterine leiomyoma and VTE across different patient models, propensity score-matched model, and frequency-matched model. Women with uterine leiomyoma aged 45 and older had a lower risk of VTE, while those with cancer, coronary artery disease, anemia, or heart failure had a higher risk of VTE. Table 4 provides the characteristics of patients diagnosed with symptomatic uterine fibroids. Based on the findings, 28 participants aged 18-60 were found to be admitted due to symptomatic uterine fibroids and requiring immediate intervention with the median age of 43.
Table 4: Participants with symptomatic fibroid characteristics.
|
Participant |
n = 28 |
|
Age (Median, years) |
43 [18-60] |
|
With the history of VTE |
|
|
- Yes |
4 (14.29 %) |
|
- No |
23 (82.14 %) |
|
- HA-VTE |
1 (3.57%) |
|
Number of fibroids |
|
|
- 1-2 |
20 (71.43 %) |
|
- 3-4 |
5 (17.86 %) |
|
- 5 or more |
3 (10.71 %) |
|
Size (Median, in cm) |
7.5 cm |
|
Risk Factor Score |
|
|
- Low risk |
5 (17.86 %) |
|
- Moderate risk |
6 (21.43 %) |
|
- High risk |
14 (50 %) |
|
- Highest risk |
3 (10.71 %) |
|
Prophylaxis |
|
|
- Enoxaparin Sodium Injection |
6 (21.43 %) |
|
- Mechanical (SCD) |
10 (35.71 %) |
|
- Both |
7 (25 %) |
|
- None |
5 (17.86%) |
|
Surgical procedure |
|
|
- Myomectomy |
24 (85.71 %) |
|
- Hysterectomy |
2 (7.14 %) |
|
- Hysterotomy |
1 (3.57 %) |
|
- TAHBSO |
1 (3.57 %) |
|
LOS (median, days) |
5 |
Among these cases, majority had no pre-existing history of VTE or were VTE-free during their hospital stay with a frequency of 23 (82.14%), while 4 (14.29%), had a pre-existing history of VTE, and 1 (3.57%), developed hospital-acquired VTE. This study also seeks to explore the size of fibroids of the patients. Based on the findings, the number of fibroids of patients varied, 20 out of 28 cases (71.43%), had 1-2 fibroids, 5 cases (17.86%), had 3-4 fibroids, and 3 cases (10.71%), had 5 or more fibroids, with a median fibroid size of 7.5 cm. According to Lacharite-Roberge et al. [12], the connection between uterine fibroids and VTE is likely due to large fibroids pressing on veins, which can slow blood flow in the pelvis and legs. Since poor circulation increases the risk of blood clots, their findings suggest that fibroid-related vein compression may be a risk factor for VTE and could eventually lead to chronic thromboembolic pulmonary hypertension (CTEPH). Risk factors were also assessed initially and adjusted as the patient’s situation changed. In terms of VTE risk, 5 cases (17.86%), were classified as low risk, 6 cases (21.43%), as moderate risk, 14 cases (50%) as high risk, and 3 cases (10.71%), as the highest risk, indicating that the majority had an increased likelihood of developing VTE. Based on the risk factor score, prophylaxis was administered. The pharmacological prophylaxis includes the administration of enoxaparin injection, and heparin injection while the mechanical intervention is by the application of a sequential compression device.
Five cases (17.86%), did not receive any pharmacological or mechanical intervention as they were deemed low risk and were advised ambulation. To manage the risk for other patients, 6 cases (21.43%) received pharmacological intervention by enoxaparin sodium injection, 10 cases (35.71%), underwent mechanical intervention with the use of a sequential compression device, and 7 cases (25%) received both pharmacological and mechanical intervention. Surgical treatments were also performed, with 24 cases (85.71%) undergoing myomectomy, 2cases (7.14%) undergoing hysterectomy, 1 case (3.57%) undergoing hysterotomy, and 1 case (3.57%) undergoing TAHBSO. Following close observation, no morbidity or mortality was recorded in these cases, and they were discharged with a median length of stay of 5 days.
DISCUSSION
This study has reported the occurrences of VTE in women experiencing symptomatic uterine fibroids which reveals a significant positive relationship between the two, suggesting that symptomatic uterine fibroids may contribute to an increased risk of VTE. According to Pandor et al. [13], hospital-acquired thrombosis makes up a significant portion of all venous thromboembolism (VTE) cases. However, the risk of developing hospital-acquired VTE can be significantly reduced through accurate risk assessment and the use of personalized pharmacological thromboprophylaxis. VTE is a condition in which a blood clot (thrombus) forms in a vein, most commonly in the deep veins of the legs, known as a deep vein thrombosis (DVT).The thrombus can dislodge from its original site and travel in the blood (embolism). If it becomes lodged in the lungs, a condition known as a pulmonary embolism (PE) arises and can cause sudden death. Hospital-acquired thrombosis is avoidable and unfortunately kills patients under the hospital care. Uterine fibroids are common, affecting over two-thirds of women of reproductive age, though only about onequarter require treatment Figure 1.
Figure 1: Reference source not found.: Figure shows the data selection process of the study from the electronic database of the hospital.
Managing VTE in these patients can be challenging due to the increased risk of bleeding associated with anticoagulation, especially in women with heavy menstrual bleeding or menorrhagia. Research suggests that larger fibroids may increase the risk of deep vein thrombosis (DVT) by pressing on major veins, like the iliac veins or the inferior vena cava. However, some cases of pulmonary embolism (PE) occur without DVT in the legs, and the location of fibroids and blood clots don’t always match. This suggests that the link between uterine fibroids and blood clots is more complex than simply hormonal changes or venous pressure [14].
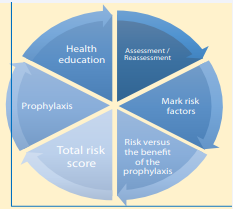
The Adult In-Patient Venous Thromboembolism (VTE) Assessment and Prophylaxis
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) in the legs or pelvis and pulmonary embolism (PE), is a serious but preventable condition that affects both hospitalized and non-hospitalized patients. It is a major reason for longer hospital stays and is the leading cause of preventable hospital deaths both in the United States and worldwide. While risk assessment and prophylactic measures have been proven effective, several factors limit their widespread use, compliance, and effectiveness. These challenges may explain why VTE remains a persistent issue in healthcare despite decades of awareness and prevention efforts [15].
Assessment / Reassessment
The first step involves identifying risk factors, which
are scored 1, 2, 3, or 5 based on the factors identified. The initial VTE assessment is conducted upon admission and is repeated if there are changes in the patient’s condition.
According to Painter [16], doctors and nurses have an important role in regularly checking on their patients, not just assessing them once. Patient assessment is a continuous process, helping medical staff track any changes in a patient’s condition—whether they are improving, getting worse, or staying the same. Similarly, Imtiaz et al. [17], recommend that VTE risk should be reassessed after 24 hours of admission or if the patient’s condition changes, such as after surgery, to help prevent complications.
Risk versus the benefit of prophylaxis
After marking the risk factors, the next step includes assessing the risk versus the benefit of prophylaxis in patients. In this step, contraindications and warnings/ precautions should be evaluated, and if the patient has any of the contraindications, mechanical prophylaxis should be considered, such as the sequential compression device (SCD), properly fitted graduated elastic compression stockings (ECS), and electric stimulation device.
Guidelines for venous thromboembolism (VTE) prevention recommend assessing a patient’s risk level using risk estimation models. Patients are classified as either high risk or low risk, and based on this, they receive either medication or chemical prophylaxis or mechanical prevention methods such as compression devices [18]. Additionally, in a study conducted by Huang [19], they reviewed different risk-assessment models (RAMs) designed to help doctors identify non-surgical patients who may need VTE prophylaxis. However, their study found that many of these published RAMs lack generalizability and are not well-validated. As electronic health records become more common, there is a growing need for reliable, real-time RAMs that can accurately assess VTE risk during patient care.
Total risk score
The calculation of total risk factor score is done after marking the risk factors. Each risk factor score should be multiplied by the number of marked factors and adding up all values to get the total. To determine the risk level, the calculated overall risk score is placed into score categories of 0-1, 2, 3-4, and 5 or higher. Based on the score, we’ll classify the risk level as low, moderate, high, or highest.
Risk scores help sort people into different risk levels based on their health factors. A higher score means a higher risk [20]. According to Kennedy [21], these scores help doctors and healthcare providers find people who may need extra screening or follow-up care. By using risk scores, hospitals and clinics can group patients into low, medium, or high risk so they can keep a closer watch on those who might need more medical attention.
Prophylaxis
Treatment options may be pharmacologic, mechanical, or both, based on the patient’s risk score and risk level. The recommended Low Molecular Weight Heparin (LMWH) could be an alternative, depending on the facility’s drug formulary. For specific surgeries such as oncology, orthopedic (TKR, THR, HFS), abdominal, and bariatric surgeries, extended prophylaxis post-discharge (1-4-5 weeks) with enoxaparin or Direct Oral Anticoagulants (DOACs) should be considered. Any reasons for not prescribing prophylaxis should also be specified.
Low-molecular-weight heparins (LMWHs), such as dalteparin and enoxaparin, are blood thinners used to prevent and treat blood clots. They help lower the risk of VTE in patients who are admitted to the hospital, whether for an emergency or a planned procedure [22]. According to Champagne and Laryea [23], patients at high risk for VTE, but not at high risk for bleeding, should receive both pharmacologic and mechanical prophylaxis, like compression devices. The choice of treatment usually depends on hospital guidelines, cost, and availability.
Health education
Additionally, the final step includes medical and nursing staff interventions and patient education about VTE. Healthcare providers empower them to understand the risk factors, symptoms, and importance of adherence to treatment and prophylaxis. Patients who are well- informed about VTE are more likely to adhere to medication regimens and lifestyle modifications, reducing the risk of complications and recurrence. Also, education facilitates early recognition of symptoms, prompting timely medical intervention and improving overall outcomes.
Educating patients about their treatment helps them understand the importance of their medication, reduces concerns about side effects, and may help prevent serious health complications [24]. Popoola [25], introduced a patient-centered approach to educating both patients and their families about VTE risks and the importance of prevention in hospitals. Their study found that most patients prefer to learn about VTE directly from their doctor, but they also benefit from videos, nurse-led discussions, and written materials Figure 2.
Figure 2: Reference source not found.: It illustrates the Adult In-Patient Venous Thromboembolism (VTE) Assessment and Prophylaxis process utilized for all adult patients aged 18 years and above.
While many efforts have successfully increased the prescription of VTE prevention treatments, a major issue remains- many hospitalized patients do not take their prescribed doses, often because they refuse treatment. Haut [26], shows that providing clear, timely, and targeted education can significantly reduce patient refusal, ensure more patients receive VTE prevention treatment, and improve overall hospital care.
The accurate diagnosis of VTE is crucial for evaluating the effectiveness of prevention efforts. Diagnosing VTE can be challenging due to the nonspecific clinical features and the potential for testing to yield false positive or negative results. As a result, both clinical assessment and objective testing are necessary. Risk scores for suspected VTE involve the clinical assessment of the pretest probability (PTP) of the disease. Early and proper use of thromboprophylaxis is both safe and effective in reducing the risk of HAVTE. However, in some cases, despite the implementation of effective prophylactic measures, some patients may still experience VTE.
The significance of identifying the potential risk
factors for VTE
Identifying risk factors for VTE is important because it helps prevent serious health complications to patients especially for women with uterine fibroids. By knowing who is at higher risk, healthcare providers can take early steps to protect their patients, such as using blood thinners medications or mechanical prophylaxis like compression devices. This can lower the chance of dangerous blood clots and improve patient safety. Table 5 shows the Adult VTE Checklist used by the AIFH which was used for all adult patients aged ≥ 18 years.
Table 5: The Adult VTE checklist.
|
ADULT IN-PATIENT VENOUS THROMBOEMBOLISM (VTE) ASSESSMENT AND PROPHYLAXIS |
||||||
|
Note: (To be assessed for all adult (≥ 18 years) patients during admission and repeated if patient’s condition changed) |
||||||
|
Date & Time of Admission: Diagnosis: BMI: |
||||||
|
? Admission ? Post-surgical procedure ? Change in condition ? Other |
||||||
|
STEP 1: MARK RISK FACTORS THEN CALCULATE THE TOTAL SCORE: |
||||||
|
Risk Factor Score = 1 |
Risk Factor Score = 2 |
Risk Factor Score = 3 |
||||
|
under G.A ?Laparoscopic surgery (>45 minutes) ?Patient confined to bed (>72 hours) ?Immobilizing plaster cast for lower limbs (< 1 month) ?Central venous access |
|
||||
|
Risk Factor Score = 5 |
||||||
(< I month)
|
||||||
|
Total Risk Factor Score: 1x__+ 2x__ + 3x __ + 5x __= |
||||||
|
STEP 2: ASSESS THE RISK VERSUS THE BENEFIT OF PROPHYLAXIS IN THE PATIENTS WITH ANY OF THE FOLLOWING: |
||||||
|
Contraindications |
Warning/Precaution |
|||||
|
|
|||||
heparin-induced thrombocytopenia) |
|
|||||
|
|
|||||
|
|
|||||
|
|
|||||
|
If the patient has any of the above or is contraindicated to anticoagulation, order Mechanical Prophylaxis
|
||||||
|
if there are any contraindications to (SCD) & (ECS): Gangrene; Recent Skin Graft; Suspected existing lower limb Deep Venous Thrombosis: Use an electric stimulation device. |
||||||
|
STEP 3: BASED ON TOTAL RISK FACTORS, SELECT ONE OF THE FOLLOWING: |
||||||
|
RISK SCORE |
RISK LEVEL |
PHARMACOLOGICAL |
MECHANICAL DEVICE |
|||
|
|
|
|
|||
|
|
BID (If BMI ≥ 40)
|
? +/- SCD |
|||
|
|
|||||
|
|
|
|
||||
Venous thromboembolism (VTE) risk scores have been developed to classify patients based on general risk factors, but a newer scoring system offers a more precise and personalized assessment. This helps determine the most suitable type and duration of prophylaxis to administer [27]. The Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI) has acknowledged hospital-associated VTE as a major patient safety concern and an essential safety requirement (ESR). There is significant scientific evidence supporting the effectiveness of implementing a mandatory VTE program to reduce the incidence of hospital-associated VTE. Adhering to best clinical practices for VTE can potentially decrease both the frequency and severity of identified hospital-associated VTE events. Full adoption of national VTE guidance and quality standards, along with ensuring that every patient undergoes a VTE risk assessment upon admission to the hospital, will enhance patient care and outcomes. Reporting all identified cases of VTE and conducting root cause analysis for every hospital-associated event will ensure that care and service delivery issues are highlighted, and education and action points are identified. Upon admission to the hospital, all adult patients must be assessed for their risk of VTE (venous thromboembolism) and bleeding. Immediate medication should be administered based on the assessment. A senior clinician (consultant or registrar) needs to review the risk assessment decision within 24 hours if the patient remains hospitalized. BMI should be calculated during the VTE assessment to ensure accuracy in scoring. If there are changes in the patient’s clinical situation, their risk of VTE and bleeding must be reassessed, and VTE prophylaxis should be prescribed based on national guidelines. The VTE risk assessment must be documented either in a hard copy of the Risk Assessment Model (RAM) or electronically according to the hospital/ clinical area’s protocol. Patients should receive written and verbal information about their VTE risk, prevention methods, and the signs and symptoms of DVT and PE when admitted and during the discharge process. Patients should not be transferred from one clinical area to another unless their VTE risk assessment and documentation are up to date, and appropriate thromboprophylaxis has been prescribed. Patients with anti-embolism stockings must have them fitted and monitored according to best practice guidelines. Preoperative and postoperative VTE assessments should be carried out, especially if the patient’s score varies in the surgery department.
Individualized VTE risk stratification allows providers to identify patients who have a favorable risk/benefit ratio for pharmacological prophylaxis and patients whose risk/benefit relationship is unfavorable or unknown. VTE, which includes DVT and PE, can lead to serious health complications. Acute PE is linked to high rates of illness and death, and VTE often occurs during hospitalization [28-31].
CONCLUSION
This study investigated the occurrence of venous thromboembolism (VTE) in women with symptomatic uterine fibroids and its association with VTE risk at Imam Abdulrahman Alfaisal Hospital. Between January 2023 and May 2024, 28 cases of VTE were recorded in women diagnosed with symptomatic uterine fibroids who were admitted to the hospital. The findings revealed a significant positive correlation between symptomatic uterine fibroids and a history of VTE (r = 0.115, p < 0.001), suggesting that fibroids may contribute to an increased risk of VTE. Although most hospitalized patients did not have fibroids or a history of VTE, 17.86% of those with fibroids either had a previous VTE or developed one during their hospital stay. Additionally, larger fibroid sizes and multiple fibroids appeared to be associated with higher risk categories. It is crucial to conduct a thorough assessment for VTE to proactively prevent and effectively manage VTE events in all patients especially in women with fibroids. Prophylactic interventions, including pharmacological and mechanical strategies, along with timely surgical intervention, should be considered to decrease VTE risk in high-risk patients. Future research is needed to explore the role of fibroid size and surgical interventions in VTE prevention and management.
ETHICAL CONSIDERATIONS
The study encompassed gathering data obtained from the data based to examine the association between symptomatic Uterine Fibroids and Venous Thromboembolism risk and determine its correlation between VTE risks among patients at Imam Abdulrahman Alfaisal Hospital. The researchers ensured the ethical standards and protocols in conducting the research study, which required addressing important ethical considerations such as informed consent, confidentiality, and data integrity.
The following measures were undertaken: Informed Consent
Informed consent from respondents was secured, as this is a cornerstone within ethical research protocols. The researchers ensured that those who participated in the study received comprehensive information regarding the research’s objectives, importance, role, potential risks, and benefits. However, this study were waived the human participation consent form, because no human was participated in the study. All data were gathered through data repository record of the locale of the study.
Confidentiality
The confidentiality of respondents’ personal data and responses was preserved, which is of utmost importance. The researchers guaranteed that all data gathered from data-based were anonymous and archived safely. Access to the data was restricted to authorized personnel only, and identifiable information was redacted.
Data Integrity
To ensure the integrity of research data and uphold the credibility and validity of the study findings, reliable data collection methods were employed, and meticulous attention was paid to the accuracy and completeness of the data. Ethically, there was no manipulation or falsification of data, thereby preserving the trustworthiness of the research outcomes. Transparent reporting of research methods and findings was prioritized, reinforcing integrity and promoting the reproducibility of results.
Minimization of Harm
The researchers ensured that no potential harm or discomfort was caused to the respondents. The researchers underscored the importance of prioritizing the well-being and dignity of all participants, prompting the researchers to actively address and mitigate any adverse effects resulting from their research activities.
Overall, the data gathered from the respondents/ participants was kept confidential, retrieved only on the data repository and used only for the purpose of the research study.
ACKNOWLEDGMENT
All of the authors of the study would like to express their sincerest gratitude to all the persons behind the success of the manuscript. To all their friends, co-workers, doctors, staffs, respondents and to their family, thank you so much.
REFERENCES
- Stewart EA, Laughlin-Tommaso SK, Catherino WH, Lalitkumar S, Gupta D, Vollenhoven B. Uterine fibroids. Nat Rev Dis Primers. 2016; 23: 16043
- Stewart EA. Uterine fibroids. NEJM. 2015; 372: 1646-1655.
- Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014; 6: 95-114.
- Giuliani E, As-Sanie S, Marsh EE. Epidemiology and management of,uterine fibroids. Int J Gynaecol Obstet. 2020; 149: 3-9
- Onwuzo C, Olukorode J, Sange W, Tanna SJ, Osaghae OW, Hassan A, et al. A Review of the Preventive Strategies for Venous Thromboembolism in Hospitalized Patients. Cureus. 2023; 15: e48421
- U.S. Centers for Disease Control and Prevention. About venous thromboembolism (Blood clots). Venous Thromboembolism (Blood Clots). 2024.
- Lacharite-Roberge AS, Raza F, Bashir R, Dass CA, Moser GW, Auger WR, et al. Case series of seven women with uterine fibroids associated with venous thromboembolism and chronic thromboembolic disease. Pulm Circ. 2019; 9: 2045894018803873
- Shiota M, Kotani Y, Umemoto M, Tobiume T, Tsuritani M, Shimaoka M, et al. Deep-vein thrombosis is associated with large uterine fibroids. Tohoku J Exp Med. 2011; 224: 87-89
- Brewer MB, Woo K, Weaver FA. Venous thromboembolism secondary to uterine fibroids: a case of phlegmasia cerulea dolens and review of the literature. Ann Vasc Surg. 2015; 29: 364.e5-364.e9
- Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015; 12: 464-474.
- Huang HK, Kor CT, Chen CP, Chen HT, Yang PT, Tsai CD, et al. Huang CH. Increased Risk of Venous Thromboembolism in Women with Uterine Leiomyoma: A Nationwide, Population-Based Case-Control Study. Acta Cardiol Sin. 2018; 34: 66-76
- Lacharite-Roberge A, Raza F, Bashir R, Dass CA, Moser GW, Auger WR, et al. Case series of seven women with uterine fibroids associated with venous thromboembolism and chronic thromboembolic disease. Pulmonary Circulation. 2018; 9: 1-7.
- Pandor A, Tonkins M, Goodacre S, Sworn K, Clowes M, Griffin XL, et al. Risk assessment models for venous thromboembolism in hospitalised adult patients: a systematic review. BMJ Open. 2021 29; 11: e045672.
- Latif H, Sosa VB, Farid S, Fernandez S, Hazen N, Morozov V, et al. Venous Thromboembolism in Women with Uterine Fibroids. Blood. 2020; 136: 28-29.
- Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015; 12: 464-474
- Painter R. Patient reassessment is a key physician and nursing responsibility | Painter Law Firm Medical Malpractice Attorneys. 2022.
- Imtiaz H, Nguyen TV, Vy Thai TT, Kouklidis G, Horgan M, Vijayaraghavan R. et al. Evaluating the Compliance to 24-Hour Venous Thromboembolism Risk Re-assessment Following Orthopaedic Surgery at a Tertiary Center: A Closed-Loop Clinical Audit. Cureus. 2024; 16: e74882.
- Chaudhary R, Damluji A, Batukbhai B, Sanchez M, Feng E, Chandra Serharan M, et al. enous Thromboembolism Prophylaxis: Inadequate and Overprophylaxis When Comparing Perceived Versus Calculated Risk. Mayo Clin Proc Innov Qual Outcomes. 2017; 1: 242-247.
- Huang W, Anderson FA, Spencer FA, Gallus A, Goldberg RJ. Risk- assessment models for predicting venous thromboembolism among hospitalized non-surgical patients: a systematic review. J Thromb Thrombolysis. 2013; 35: 67-80
- Davies MJ, Gray LJ, Ahrabian D, Carey M, Farooqi A, Gray A, et al. A community-based primary prevention programme for type 2 diabetes mellitus integrating identification and lifestyle intervention for prevention: a cluster randomised controlled trial. Southampton(UK): NIHR J Library. 2017.
- Kennedy S. Explaining the basics of patient risk scores in healthcare. Healthtech Analytics. 2023.
- Solari.F, Varacallo MA. Low-Molecular-Weight Heparin (LMWH). National Center for Biotechnology Information. 2025.
- Champagne B, Laryea J. Venous thromboembolism prophylaxis. Clinics in Colon and Rectal Surgery. 2013; 26: 153-159.
- Clarkesmith DE, Pattison HM, Lip GY, Lane DA. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One. 2013; 8: e74037
- Popoola VO, Lau BD, Shihab HM, Farrow NE, Shaffer DL, Hobson DB, et al. Patient Preferences for Receiving Education on Venous Thromboembolism Prevention - A Survey of Stakeholder Organizations. PLoS One. 2016; 11: e0152084.
- Haut ER, Aboagye JK, Shaffer DL, Wang J, Hobson DB, Yenokyan G, et al. Effect of Real-time Patient-Centered Education Bundle on Administration of Venous Thromboembolism Prevention in Hospitalized Patients. JAMA Netw Open. 2018; 1: e184741
- Caprini JA. Risk assessment as a guide for the prevention of the many faces of venous thromboembolism. Am J Surg. 2010; 199: S3-S10
- Flanagan L, Bassa BA, Moriarty JM, Lyons F, Sands F, Comer C, et al. F. N. Hospital PERT: Bridging VTE care across all disciplines. Thrombosis Update. 2016.
- Agnelli G, Anderson F, Arcelus J, Bergqvist D, Brecht J, Greer I, et al. Venous thromboembolism (VTE) in Europe. Thrombosis and Haemostasis. 2007; 98: 756-764.
- Henke PK, Kahn SR, Pannucci CJ, Secemksy EA, Evans NS, Khorana AA, et al. Call to action to prevent venous thromboembolism in hospitalized patients: A policy statement from the American Heart Association. Circulation. 2020; 141.
- Hunt BJ. Preventing hospital-associated venous thromboembolism.BMJ. 2019b.