Global Epidemiology of Asthma: An Ecological Study of GBD 2021 Results and Forecasts to 2040
- #. These authors contributed equally to this work
- 1. Postgraduate Training Base Alliance, Wenzhou Medical University, China
- 2. Wenzhou Institute, University of Chinese Academy of Sciences, China
- 3. The Department of Pediatrics, Ruijin Hospital, Shanghai Jiao-tong University School of Medicine, China
Abstract
Background: Asthma is a prevalent chronic respiratory disorder with marked regional management disparities; comprehensive epidemiological research is critical to guide targeted interventions.
Methods: This ecological study utilized de-identified aggregate data from the Global Burden of Disease Study (GBD) 2021, covering 204 countries/territories and all age groups (0–95+ years). The Bayesian Age-Period-Cohort (BAPC) model was employed to forecast asthma burden trends from 2022 to 2040, with age-standardized rates and 95% uncertainty intervals (UI) used for statistical analysis.
Results: In 2021, 260.5 million global asthma cases were reported (age-standardized prevalence rate [ASPR]: 3,340.1 per 100,000), a 38.7% decrease since 1990 (EAPC:
-1.59, 95% CI: -1.74 to -1.43). Low sociodemographic index (SDI) regions saw increased cases (42.9 million) but decreased ASPR, while other regions declined in both. An unbalanced-M shaped association between SDI and age-standardized disability-adjusted life year (DALY) rate was identified (1990–2021, P ≤ 0.001). By 2030, global cases are projected to reach
292.3 million (95% UI: 201.7–384.9) as a primary benchmark aligned with UN Sustainable Development Goals (SDGs); 2040 estimates are 321.0 million (95% UI: 113.5–528.6), interpreted as a plausible scenario due to long-range uncertainties. Low SDI regions face greater growth, while high SDI regions maintain higher ASPR (3,508.4 per 100,000 by 2040).
Conclusions: This study reveals a multifaceted asthma epidemiological pattern marked by declining ASPR and an SDI-linked bimodal DALY burden. While global burden has plateaued, high and low SDI regions require tailored interventions to address distinct challenges, providing evidence for global asthma prevention strategies.
Keywords
• Asthma; Epidemiology; Global Burden of Disease; Sociodemographic Index; Forecast
Citation
Zhu H, Wen Y, Wu Y, Xia Z, Wu Q, et al. (2026) Global Epidemiology of Asthma: An Ecological Study of GBD 2021 Results and Forecasts to 2040. J Prev Med Healthc 8(1): 1043.
BACKGROUND
Bronchial asthma (asthma), a prevalent chronic respiratory disorder, is characterized by recurrent and persistent attacks that significantly impair patients’ quality of life, leading to substantial psychological strain and financial burdens. Its etiology is multifactorial, encompassing the interplay of genetic predisposition, environmental influences, immune dysregulation, and other contributing elements [1]. According to Global Initiative for Asthma 2024 (GINA2024), approximately 300 million people around the world have asthma. It is becoming more prevalent in many economically developing countries. Asthma poses an escalating challenge for patients, communities, and healthcare systems worldwide. It significantly disrupts individuals’ work, education, and family dynamics, particularly when children are affected. Despite advancements, asthma remains a life-threatening condition, claiming lives globally, including those of young individuals. Notably, nearly 96% of asthma-related deaths occur in low- and middle-income countries [2]. Currently, individualized treatment strategies are advocated to optimize asthma control, given the recurrent and persistent nature of the condition. For patients with suboptimal control, conventional therapies such as glucocorticoids and β-receptor agonists may prove insufficient, necessitating advanced interventions like biological agents. Beyond environmental and genetic influences, advancements in diagnostic and therapeutic approaches are exacerbating disparities in asthma management across countries and regions [3,4].
The Global Burden of Disease (GBD) 2021 study indicates that asthma-related mortality rates are highest in low and middle sociodemographic index (SDI) countries, whereas prevalence rates peak in high SDI nations. Further epidemiologic studies of asthma spanning the globe are warranted to inform actions deliberately targeting the decrease of disease burden, and the equity in asthmatic prevention, diagnosis and treatment.
METHODS
This is an ecological study based on secondary aggregate data from the GBD 2021 database, which covers 204 countries and territories worldwide and spans all age groups (0–95+ years) from 1990 to 2021. No individual level data were accessed, and the study population was defined as all individuals included in the GBD 2021 asthma burden estimates.
Data Sources and Disease Definition
The data utilized in this study were sourced from GBD 2021 database, a comprehensive repository of global public health information encompassing epidemiological data on diseases, injuries, and risk factors. The GBD employs standardized methodologies to integrate diverse data sources, including population censuses, disease registries, hospital records, and national surveys. These data are refined and supplemented using Bayesian statistical models and machine learning algorithms, enabling high precision estimations of disease burden. The GBD utilizes the Disease Modeling-Bayesian Meta-Regression (DisMod MR) framework to estimate asthma prevalence, incidence, and mortality, while also calculating age-standardized rates and disability-adjusted life years (DALYs) based on demographic data. To address data scarcity in certain regions, the GBD applies space-time Gaussian process regression (ST-GPR), ensuring both global comparability and regional specificity in its findings.The data used to estimate asthma burden are accessible via the GBD 2021 database (https://vizhub.healthdata. org/gbd-results/).
Forecasting
The Bayesian Age-Period-Cohort (BAPC) model, combined with nested Laplace approximation, is employed to forecast disease prevalence trends from 2022 to 2040. As a statistical tool, the BAPC model enables the analysis and prediction of age, period, and cohort effects on population level events, including mortality and disease incidence. Combining the strengths of Bayesian statistics, the model handles complex data structures and uncertainty. The BAPC model disentangles the data by separating age, period, and cohort effects, facilitating a comprehensive analysis of disease burden trends. By integrating the INLA algorithm, the model effectively combines sample and prior information to estimate the posterior distribution, avoiding complexities associated with mixing and convergence. In comparison to other models utilizing GBD data, the BAPC model exhibits reduced error rates and enhanced coverage, solidifying its widespread application in forecasting future disease burdens. The BAPC model was selected over alternative forecasting frameworks (e.g., autoregressive integrated moving average, ARIMA) due to its superior ability to disentangle age, period, and cohort effects—critical for analyzing long-term asthma burden trends across demographic strata. Its integration of the INLA algorithm also reduces computational complexity and improves uncertainty interval coverage compared to Markov chain Monte Carlo (MCMC) methods, making it optimal for large-scale GBD dataset analysis.
Statistics and Plotting
Age-standardized prevalence rates (ASPR) were calculated using the GBD 2021 reference population to ensure cross-regional comparability, presented as estimates per 100,000 population along with their 95% uncertainty intervals (UI). Percentage change was utilized to quantify variations in prevalence, incidence, and mortality rates between 1990 and 2021. Estimated Annual Percentage Change (EAPC) was calculated to quantify the velocity of trends in prevalence, incidence, and mortality rates between 1990 and 2021. Specifically, we used a linear regression model where the dependent variable was the natural logarithm of age-standardized rates, and the independent variable was the calendar year. EAPC values and 95% confidence intervals (CI) were derived from the regression coefficient, with EAPC = (exp(β) - 1) × 100% (β = regression coefficient). EAPC values and 95% CIs were reported alongside absolute percentage changes to reflect both magnitude and annual velocity of trends. All statistical analyses and visualizations were performed using RStudio IDE (version 2022.07.1 Build 554) with R language (version 4.2.1), incorporating the R packages BAPC (version 0.0.36), INLA (version 23.04.24), and ggplot2 (version 3.5.1). P-values less than 0.05 (two tailed) were considered statistically significant for all analyses. Figures were edited using Adobe Illustrator software (version 2020).
RESULTS
Prevalence and trends (1990–2021)
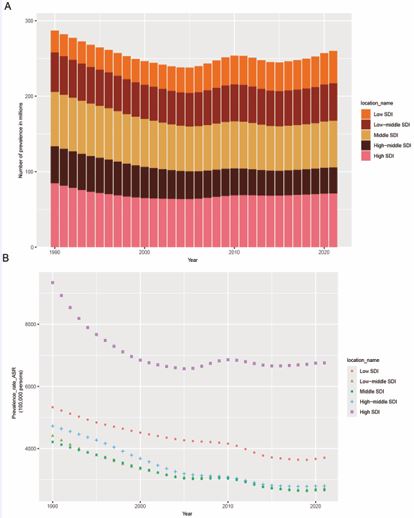
Globally, approximately 260.5 million individuals were affected by asthma in 2021, with an age-standardized prevalence rate (ASPR) of 3,340.1 per 100,000 population, marking a notable 38.7% decrease since 1990 (EAPC: -1.59, 95% CI: -1.61 to -1.43) (Table 1). Across the five sociodemographic index (SDI) regions, the number of asthma cases in 2021 increased in low SDI regions compared to 1990 (14.0 million increase, EAPC: -1.22, 95% CI: -1.28 to -1.15), while other SDI regions experienced a decline during the same period (Table 1). Over the past three decades (1990–2021), the burden of asthma has displayed distinct trends among the five SDI regions (Figure 1). High-middle SDI regions demonstrated the steepest decline in case numbers (14.6 million decrease,EAPC: -1.83, 95% CI: -1.99 to -1.67), whereas low SDI regions showed a gradual rise, aligning with the data presented in Table 1 (Figure 1A). In high SDI regions, the ASPR trend exhibited greater volatility but a consistent downward EAPC (-0.75, 95% CI: -0.98 to -0.51) and remained elevated compared to other regions, where a steady decline was observed (Figure 1B). Age-stratified analysis revealed distinct lifecycle trajectories. The 0–14 years group had a 42.0% ASPR decrease (from 4120.5 to 2389.7 per 100,000) with an EAPC of -1.83 (95% CI: -1.96 to -1.70) from 1990 to 2021, while case numbers declined from 58.2 to 47.4 million. In contrast, the 70+ years group showed a milder 18.7% ASPR decrease (from 3856.2 to 3132.4 per 100,000; EAPC: -0.72, 95% CI: -0.85 to -0.59) but a 74.2% increase in case numbers (from 16.7 to 29.1 million), driven by global population aging. The 15–69 years group, as the largest demographic, exhibited a 39.3% ASPR decrease (EAPC: -1.57, 95% CI: -1.69 to -1.45) and a 20.7% reduction in case numbers (from 212.4 to 168.3 million).
Table 1: Prevalent Cases, Age-Standardized Rate (ASR) and EAPC of Asthma Globally and Across GBD Regions (1990–2021).
|
Region |
Prevalence (95% UI) – 1990 (millions) |
Prevalence (95% UI) – 2021 (millions) |
ASRs per 100,000 (95% UI) - 1990 |
ASRs per 100,000 (95% UI) - 2021 |
EAPC (95% CI) (1990– 2021) |
|
Global |
287.3 (250.4–331.1) |
260.5 (227.2–298.0) |
5568.3 (4899.6–6349.8) |
3340.1 (2905.2–3832.2) |
-1.59 (-1.74, -1.43) |
|
Low SDI |
29.0 (24.8–33.8) |
42.9 (36.9–49.5) |
5329.8 (4748.8–5987.9) |
3705.5 (3299.3–4128.1) |
-1.22 (-1.28, -1.15) |
|
Low-middle SDI |
52.3 (44.7–61.4) |
49.7 (43.2–57.5) |
4409.4 (3889.8–5063.1) |
2714.9 (2388.5–3105.8) |
-1.5 (-1.64, -1.36) |
|
Middle SDI |
72.0 (60.5–86.2) |
61.8 (53.2–72.3) |
4214.1 (3652.1–4939.3) |
2664.9 (2269.0–3168.6) |
-1.51 (-1.62, -1.4) |
|
High-middle SDI |
49.0 (42.5–56.4) |
34.4 (29.6–40.3) |
4723.5 (4098.1–5438.7) |
2796.6 (2325.2–3391.4) |
-1.83 (-1.99, -1.67) |
|
High SDI |
84.6 (74.7–96.0) |
71.2 (63.1–80.1) |
9339.4 (8156.1–10674.6) |
6755.3 (5831.8–7825.2) |
-0.75 (-0.98, -0.51) |
Note: ASRs=Age-Standardized Rates; UI=Uncertainty Interval; EAPC=Estimated Annual Percentage Change; CI=Confidence Interval. Data source: Global Burden of Disease Study 2021 database (https://vizhub.healthdata.org/gbd-results/, DOI: 10.31981/GBD.2021.0).
Figure 1 Asthma prevalence in globe and the five SDI regions from 1990 to 2021. A. The prevalence numbers of asthma. B. The ASPR of asthma. SDI = sociodemographic Index, ASPR = age-standardized prevalence rate.
Risk factors for asthma DALYs
Asthma, as a chronic respiratory condition, is characterized by persistent and recurrent symptoms, significantly impairing patients’ quality of life and imposing a substantial disease burden. According to GBD 2021 study, DALYs and mortality rates associated with asthma were linked to four primary risk factors: smoking, occupational asthmagens, nitrogen dioxide (NO?) pollution, and high body-mass index (BMI). The contribution of these risk factors to asthma-related DALYs varied significantly across GBD regions (Figure 2A). However, in global (15.4%) and most regions, high BMI had the highest contributions to DALYs due to asthma. Occupational asthmagens had the highest contributions (9.6%) only in Eastern Sub-Saharan Africa, slightly exceeding high BMI (9.5%). Additionally, the risk factors contributing to the asthma burden among children under 14 years of age were analyzed separately, focusing on nitrogen dioxide (NO?) pollution and high BMI (Figure 2B). In most regions, high BMI had the greater contributions in children, regardless of gender, than NO? pollution. Only in high-income Asia Pacific, did NO? pollution have the greater contributions among both male and female.
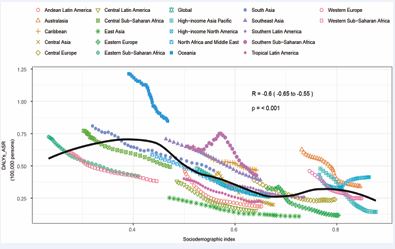
Association between SDI and asthma DALYs
At the regional level, an unbalanced M-shaped relationship was observed between SDI and the age- standardized DALY rate for asthma from 1990 to 2021 (P ≤ 0.001). The age-standardized DALY rate exhibited an exponential increase with rising SDI, peaking at an SDI of approximately 0.35, followed by a decline. However, it rose again until the SDI reached around 0.76, after which it decreased once more. Regions such as Oceania, Southern Sub-Saharan Africa, Southeast Asia, and the Caribbean demonstrated higher-than-expected DALY rates relative to their SDI values during this period. Conversely, East Asia, Central Latin America, Andean Latin America, and Tropical Latin America exhibited lower-than-expected asthma burdens from 1990 to 2021 (Figure 3).
Global asthma burden forecast (2022–2040)
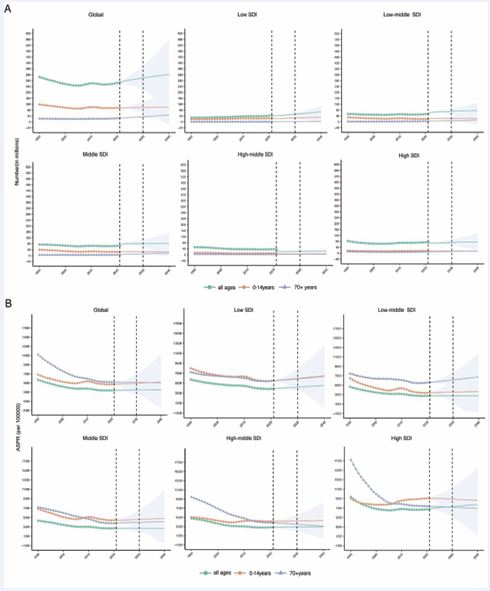
The Bayesian Age-Period-Cohort (BAPC) model was utilized to project future trends in the number of asthma cases and ASPR from 2022 to 2040, with 2030 designated as a primary benchmark year to align with the United Nations Sustainable Development Goals (SDGs) and enhance the statistical stability of near-term forecasts. By 2030, global asthma cases are projected to reach 292.3 million (95% UI: 201.7–384.9), with an age-standardized prevalence rate (ASPR) of 3,412.6 per 100,000 (95% UI: 2,356.8–4,468.4)—a 12.2% increase from the 2021 observed cases (260.5 million), reflecting a moderate but steady growth trajectory projected by the BAPC model. A further rise in the global total number of asthma cases is expected between 2030 and 2040, reaching 321.0 million (95% UI: 113.5 – 528.6) by 2040 (Figure 4A). This upward
trend is particularly pronounced in low SDI regions (Figure 4A). It is predicted that the number of female cases is more than that of male cases globally (Figure 4A). Age-stratified forecasts indicate the 70+ years group will drive future growth, with cases projected to reach 39.6 million by 2040 (95% UI: 13.8–65.4 million), a 36.1% increase from 2021. The 0–14 years group will remain stable (48.7 million by 2040, 95% UI: 17.2–80.2 million), while the 15–69 years group is expected to reach 232.7 million (95% UI: 82.5– 382.9 million). Meanwhile the ASPR is expected to follow a milder upward trend, culminating at 3,508.4 (95%UI 1,240.3 – 5,776.5) per 100,000 in 2040 globally; however, it will remain lower than the historical peak ASPR (Figure 4B). Notably, the 2040 projections are associated with wide 95% uncertainty intervals, reflecting inherent uncertainties in long-range ecological forecasting that arise from potential unforeseen events (e.g., large-scale public health interventions, climate anomalies) and model sensitivity over an 18-year horizon. Therefore, the 2040 estimates should be interpreted as a plausible scenario rather than a definitive projection. As the model cannot account for emerging environmental shifts or targeted interventions. The model projected a sustained increase in ASPR of asthma in high SDI regions, with this trend being more pronounced compared to other regions (2030 ASPR: 6,982.1 per 100,000; 2040 ASPR: 7,341.5 per 100,000).
DISCUSSION
Unlike prior studies focusing on single-country or high- income region asthma burden [5-14], this study provides a global, 32-year temporal analysis and 2040 forecast, and is the first to identify an unbalanced-M shaped association between SDI and asthma DALY rates—a pattern that clarifies the dual burden of asthma in both low-SDI (high mortality) and high-SDI (high prevalence) regions. Asthma, an atopic disease, exerts lifelong impacts on patients due to its chronic nature and associated comorbidities, posing significant challenges to public health and the global economy. However, a growing body of research predominantly focuses on high-income countries, such as the United Kingdom (UK), European Union (EU) nations, and the United States (USA), reflecting both the higher prevalence of allergic diseases in affluent populations and the advanced diagnostic infrastructure in these regions [5-13]. Furthermore, asthma is frequently regarded as a pediatric condition, leading to a predominant focus on children in most studies. This article offers a unique and timely global perspective on the true public health impact of asthma. By analyzing the data from the GBD 2021 study, we describe the global burden of asthma, while exploring their associations with SDI, and risk factors.
Figure 2 The proportions of disability-adjusted life years (DALYs) attributable to asthma. A. Percentage of DALYs due to asthma attributable to each risk factor for the 21 Global Burden of Disease regions in 2021; B. Percentage of DALYs due to asthma attributable to each risk factor among children under 14 years for the 21 Global Burden of Disease regions in 2021.
The findings indicate that, compared to 1990, both the global number of asthma cases and the ASPR had decreased by 2021. High SDI regions demonstrated significantly higher ASPR compared to other SDI regions. Notably, age standardized asthma prevalence exhibited considerable heterogeneity across GBD regions and countries. By 2021, the global total number of asthma cases reached 260.5 million, with an age-standardized prevalence of 3,340.1 per 100,000 population, reflecting substantial improvements since 1990. This decline suggests advancements in healthcare systems and public health interventions. Although most SDI regions followed the global trend, significant variations were observed across the five SDI categories. Consistent with previous research, high SDI regions exhibited higher ASPR than other regions [14]. The number of asthma patients has declined in most SDI regions over the past three decades, with only low SDI areas showing an upward trend. This disparity can be attributed to multiple factors, including improved access to medical resources in high SDI regions, facilitating timely diagnosis and systematic documentation of symptomatic cases. Furthermore, high-income regions are characterized by longer indoor working hours, reduced outdoor activity, more processed diets, increased susceptibility to allergies, and potentially elevated levels of psychological stress [1 15]. In low SDI regions, the rising asthma prevalence could be related not only to population growth but also to the gradual Westernization of lifestyles [15,16].
Figure 3 Age-standardized disability-adjusted life year (DALY) rates for asthma across the 21 Global Burden of Disease (GBD) regions, stratified by sociodemographic index (SDI), from 1990 to 2021. For each region, 32 data points are plotted, representing the observed age-standardized DALY rates over this period. Expected values, derived from the sociodemographic index and disease rates across all regions, are depicted as a solid line. Regions above the solid line indicate a higher-than-expected burden (e.g., Oceania), while those below the line reflect a lower-than-expected burden (e.g., East Asia).
Regarding risk factors, high BMI is the leading contributor to DALYs attributable to asthma globally and in most regions. In the majority of regions, BMI exerts a greater influence on children under 14 years of age compared to nitrogen dioxide (NO?) pollution. However, in high-income Asia-Pacific regions, NO? pollution has a more pronounced impact on children within this age group. Previous studies have established that obesity represents a chronic state of low-grade systemic inflammation [17]. The elevated production of adipokines, coupled with inherent asthma susceptibility, can intensify airway inflammation, leading to more severe and treatment-resistant asthma phenotypes. The co-occurrence of obesity and asthma poses distinct risks and complications, underscoring the need for personalized interventions to enhance health outcomes. The Global Initiative for Asthma (GINA) guidelines recommend physical activity as a strategy to mitigate asthma severity and lower the risk of recurrence (2). A 2024 study published in MEDICINE compared the impact of continuous-load aerobic exercise versus graded aerobic exercise on cardiopulmonary health and functional capacity in obese children with asthma, demonstrating that graded aerobic exercise was more effective in enhancing cardiopulmonary function [18]. Nevertheless, we recommend that all asthma patients, including adults, participate in moderate aerobic activities during stable phases of the disease under medical supervision, with graded aerobic exercise being especially recommended.
In fact, asthma burden is also influenced by host genetics, prematurity or low birth weight, anxiety, and environmental exposures, including fine particulate matter (PM2.5), microplastics, extreme weather events, and climate change [16-22]. While the GBD database includes relatively limited factors, it is evident that high BMI significantly impacts asthma outcomes. We strongly advocate that all asthma patients participate in aerobic exercise during stable disease phases to enhance disease management and mitigate the negative impacts on daily life, under the supervision of a healthcare professional.
The age-standardized DALY rate for asthma showed an M-shaped correlation with SDI. As SDI increased, the age-standardized DALY rate exhibited an exponential rise, reaching its first peak at an SDI of approximately 0.35, followed by a decline. However, it rose again, achieving a second peak at an SDI of around 0.76, before subsequently decreasing. SDI is a composite index assessing a country or region’s development status, based on data, such as fertility rate for women under 25, average education level for women aged 15 and above, and per capita income. Research based on 1990~2019 GBD data indicated that asthma incidence in high-SDI regions (365.9 [245.7, 642.9]) is much higher than that in low-SDI regions (430.2 [279.2, 675.2]) [23]. Another study has analyzed SDI in relation to asthma prevalence, incidence, mortality, and DALYs, revealing that higher SDI corresponds to lower mortality, whereas DALYs are the lowest in high SDI regions and the highest in low SDI regions [14]. Our study, through statistical principles, clarified the correlation between SDI and asthma DALYs, indicating a clear relationship. This observation is rooted in reality, as elevated asthma risk and healthcare disparities across different SDI regions contribute to this imbalance. With the progressive adoption of Westernized lifestyles, low SDI regions face increased asthma risk but lack adequate healthcare infrastructure to mitigate the burden. Furthermore, regions such as Oceania, Southern Sub-Saharan Africa, Southeast Asia, and the Caribbean exhibited higher-than-expected DALY rates relative to their SDI values, underscoring the need for targeted interventions by policymakers and healthcare providers to address the high asthma burden in these areas.
Figure 4 Projected case numbers (A) and ASPR (B) of asthma for global and different regions from 2022 to 2040. ASPR = age-standardized prevalence rate. Projected case numbers for the 15–69 years group are 232.7 million (95% UI: 82.5–382.9 million) by 2040, driving the global growth alongside the 70+ years group.
This statistically significant unbalanced M-shaped association (P ≤ 0.001) is characterized by two distinct peaks at SDI≈0.35 and SDI≈0.76, reflecting the epidemiological transition of asthma drivers across different socioeconomic development stages. This unbalanced M-shaped association, characterized by two distinct peaks at SDI≈0.35 and SDI≈0.76, reflects the epidemiological transition of asthma drivers across different socioeconomic development stages. At SDI≈0.35 (low-to-lower-middle income stage), the first peak is predominantly driven by traditional environmental exposures and improved diagnostic capacity. Representative countries in this SDI range include Nigeria (SDI=0.34) and Bangladesh (SDI=0.33), where biomass fuel use accounts for over 70% of household energy consumption [14], leading to high levels of household air pollution (HAP) with an exposure rate exceeding 60%. HAP, combined with high childhood respiratory infection rates and undernutrition affecting 25%-30% of children under 5 [15], synergistically exacerbates airway inflammation and asthma susceptibility. Meanwhile, the gradual expansion of basic medical resources in these regions has improved the identification of previously undiagnosed cases, creating a “diagnostic paradox” that further elevates reported DALY rates [15].
In contrast, the second peak at SDI≈0.76 (upper-middle income stage) is shaped by the transition from environmental pollution-driven to lifestyle-driven risk factors—consistent with the GBD-defined high BMI as the leading global risk factor for asthma DALYs. Typical nations include Brazil (SDI=0.75) and Poland (SDI=0.77), which have reduced HAP exposure through industrialization and energy transition but face a surge in “Westernized” risk factors: adult obesity rates exceeding 30% (the primary contributor to local asthma DALYs), pet ownership rates of 45%-50% (increasing indoor allergen exposure), and increased antibiotic use leading to gut microbiota dysbiosis [16]. Obesity induces low-grade systemic inflammation via adipokine overproduction, which synergizes with asthma susceptibility to intensify airway hyperresponsiveness [17]. Additionally, the mature diagnostic systems in these regions ensure high detection rates of mild cases, contributing to the second DALY peak [18]. This transition aligns with global epidemiological trends of allergic diseases shifting from pollution-driven to lifestyle-driven [4]. Notably, regions like Oceania (average SDI=0.85) and the Caribbean (average SDI=0.72) fall near the second peak, where lifestyle risk factors overlap with residual environmental pollution, leading to higher-than-expected DALY rates relative to their SDI values. Regions with higher-than-expected DALYs (e.g., Oceania, Southern Sub Saharan Africa) either overlap with the second M-shaped peak (SDI≈0.76) or face residual traditional risk factors combined with limited healthcare access, exacerbating their burden beyond SDI-predicted levels.
UNOBSERVED RISK FACTORS MODULATING FUTURE ASTHMA BURDEN
Beyond the four GBD-defined risk factors (smoking, occupational asthmagens, NO? pollution, high BMI) three unobserved factors merit attention for interpreting future burden trajectories as they are not incorporated into the current BAPC model yet may significantly modulate asthma prevalence.
Elevated temperatures from climate change prolong atmospheric residence of ozone (O?) and fine particulate matter (PM?.?) whose co-exposure exacerbates airway inflammation and acute asthma episodes while warming extends growing seasons of allergenic plants in high latitude regions increasing pollen concentrations by 30% 50% and advancing allergy seasons to disproportionately affect patients with allergic asthma [4-21]. Per the Intergovernmental Panel on Climate Change (IPCC) Sixth Assessment Report such climatic shifts will intensify over the next two decades potentially raising asthma prevalence in low- and middle-latitude regions (e.g., South Asia, Central and South America) by 5%-8% by 2040 [20].
Floods from extreme weather events trigger indoor mold growth with mold spore exposure associated with a 40%-60% increase in asthma-related emergency department visits within 1-2 weeks while droughts exacerbate sand and dust storms whose mineral particles bind allergens to prolong airway inflammation [19-23]. Thunderstorm asthma a phenomenon linked to sudden pollen fragmentation and high humidity has emerged as a severe acute risk in regions like Australia and Europe with climate change projected to increase its frequency these events disrupt medication access and worsen treatment adherence in low SDI regions with fragile healthcare infrastructure while high SDI regions with a higher proportion of allergic asthma patients face greater susceptibility to allergen concentration fluctuations [19,20].
Climate change and urbanization drive prolonged pollen seasons and increased allergen diversity expanding at-risk populations the global average pollen season has lengthened by 20-30 days over the past three decades with 2%-3% annual growth in pollen concentrations in temperate regions [4]. Urbanization-induced introduction of exotic plants (e.g., Ambrosia artemisiifolia in North America, Reynoutria japonica in Asia) adds novel allergens whose cross-reactivity with native allergens particularly affects children and adolescents [4-22]. By 2040 pollen exposure duration in major global cities is expected to increase by 15%-20% potentially raising the proportion of allergic asthma to 65%-70% of all cases suggesting the current model may underestimate burden in high SDI regions [4].
These unobserved factors confirm the BAPC model projections represent a baseline scenario future asthma burden will be shaped by the interplay of socioeconomic development lifestyle transitions and environmental changes. Integrating climate models environmental monitoring data and epidemiological surveys in future studies will enhance the precision of burden forecasts and support region-specific risk mitigation. These factors may lead to underestimation of 2040 burden in high SDI regions due to allergic asthma expansion and low SDI regions due to climate-induced pollution indicating the projected 321.0 million cases are a conservative estimate.
Age-specific differences in asthma trajectories may stem from distinct underlying mechanisms. Pediatric asthma (0–14 years) is more sensitive to early-life environmental exposures and developmental factors, such as NO? pollution, childhood obesity, and immature immune systems (Figure 2B). This explains the steeper ASPR decline in this group, as global efforts to reduce childhood environmental risk factors and improve early diagnosis have yielded tangible results. In contrast, adult onset asthma in the 70+ years group is often comorbid with chronic obstructive pulmonary disease (COPD), cardiovascular conditions, and age-related immune dysfunction, leading to slower ASPR declines. The growing case numbers in the elderly population primarily reflect global demographic aging, as longer lifespans increase the likelihood of developing asthma or experiencing disease progression. The 15–69 years group, as the largest demographic, exhibits intermediate trends, with burden driven by a mix of occupational exposures, lifestyle factors (e.g., obesity, sedentary behavior), and persistent environmental triggers. These age-specific patterns underscore the need for lifecycle-tailored prevention and management strategies. Notably, the 70+ years old group’s projected 36.1% case growth by 2040 contrasts with the stable pediatric burden, reflecting demographic aging and age-specific comorbidities that are not observed in children, highlighting the need for geriatric-focused asthma management.
The BAPC model projections, with 2030 as a primary benchmark year, present critical insights into the evolving epidemiology of asthma through 2040, revealing distinct patterns across demographic and socioeconomic strata. The anticipated 12.2% increase in global asthma prevalence from 2021 to 2030 (reaching 292.3 million cases) provides a statistically stable near-term reference aligned with the United Nations Sustainable Development Goal (SDG) 3.4 (reducing non-communicable disease burden), while the further 9.8% growth from 2030 to 2040 (to 321.0 million cases) underscores the persistent burden of this chronic respiratory condition. Given the wide 95% uncertainty intervals for 2040 estimates (e.g., global cases ranging from 113.5 to 528.6 million), the projections should be interpreted as a baseline scenario rather than definitive outcomes, with inherent limitations related to long-term ecological forecasting fully acknowledged. These uncertainties stem from multiple factors, including potential shifts in environmental risk factors, changes in healthcare access, and unforeseen public health crises that may alter disease trajectories. Notably, the disproportionate case accumulation in low SDI regions aligns with existing evidence of environmental triggers and healthcare access disparities in these areas. These findings emphasize the urgent need for targeted interventions in low-resource settings to address modifiable risk factors and improve asthma management. The gender disparity, with female cases consistently outnumbering male cases, may reflect both biological susceptibility differences and diagnostic patterns, warranting further investigation into sex-specific risk factors. These findings call for gender sensitive approaches in asthma prevention and treatment strategies.
The ASPR projections reveal a nuanced epidemiological pattern. While the global ASPR is expected to increase to 3,508.4 per 100,000 by 2040, it remains below historical peaks, suggesting that current interventions, such as improved access to inhaled corticosteroids and public health campaigns, have had some success in mitigating the burden. However, the sustained increase in ASPR in high SDI regions is particularly concerning and contrasts with traditional epidemiological transitions. This trend indicates that there may exist emerging risk factors in high SDI regions, and efforts should address emerging risk factors, including urban air pollution and lifestyle changes, while maintaining robust diagnostic and management frameworks.
These projections highlight the need for region-specific public health strategies. In low SDI regions, interventions should prioritize reducing environmental triggers, such as indoor air pollution, and expanding access to affordable asthma medications. In high SDI regions, efforts should address emerging risk factors, including urban air pollution and lifestyle changes, while maintaining robust diagnostic and management frameworks. Furthermore, the gender disparity in asthma prevalence warrants further research to elucidate the underlying mechanisms and inform gender-specific interventions.
STUDY LIMITATIONS
Several limitations of this study should be acknowledged when interpreting the findings. First, data scarcity in the Global Burden of Disease (GBD) 2021 database for certain low-sociodemographic index (SDI) regions (e.g., select areas of Southern Sub-Saharan Africa) may introduce minor biases into regional burden estimates. Second, only four primary risk factors were evaluated due to data availability constraints within the GBD framework, excluding potential etiological contributors such as genetic predisposition, indoor allergen exposure, and psychosocial stressors. Third, the Bayesian Age-Period-Cohort (BAPC) model projections are predicated on historical epidemiological trends and cannot accommodate unforeseen events (e.g., large-scale public health interventions, novel pandemics, or policy overhauls) that could reshape future asthma burden trajectories. Fourth, the ecological study design prohibits the establishment of causal associations between SDI/risk factors and asthma outcomes, as individual level confounding variables (e.g., socioeconomic status at the personal level, medication adherence) cannot be adjusted for in aggregate analyses. Despite these inherent limitations, the findings provide critical population-level insights to inform global asthma prevention strategies and evidence-based resource allocation.
CONCLUSIONS
The burden of asthma varies with gender, age, BMI, geographical location, SDI level, period and birth cohort. This study revealed a complex epidemiological landscape of asthma, with a declining ASPR globally but distinct age specific trajectories—particularly the growing burden in the 70+ years population. Our analysis reveals a distinctive bimodal (unbalanced-M shaped) correlation between the SDI and asthma-related DALYs across the study period (1990-2021), driven by different risk factors at SDI≈0.35 (traditional environmental pollution) and SDI≈0.76 (Westernized lifestyles) with clear regional manifestations. Projective modeling indicates a sustained upward trajectory in both global asthma case numbers and ASPR through 2040, with 2030 serving as a statistically stable benchmark aligned with UN SDGs. These epidemiological patterns necessitate a paradigm shift in public health strategy, emphasizing precision-based interventions for high-risk demographics (e.g., elderly populations in low SDI regions, children in high-income Asia Pacific) and geographic hotspots (e.g., Oceania, Southern Sub Saharan Africa). Such targeted approaches should prioritize optimization of disease management protocols, mitigation of population health burden, and enhancement of pulmonary health outcomes through evidence-based resource allocation and policy implementation.
DECLARATIONS
Ethics approval and consent to participate
Ethics approval is not required as this study uses de identified aggregate public data from the Global Burden of Disease Study 2021, with no access to individual-level medical or demographic records, and the research involves no human subjects, interventions, or privacy data collection. This exemption was confirmed by the Institutional Review Board of Wenzhou Medical University (reference no. WMU-IRB-2025-012). The study is fully compliant with the Declaration of Helsinki and international epidemiological research ethical norms. Informed consent is not applicable due to the nature of the publicly available aggregated data, which contains no identifiable personal information.
Availability of data and materials
The datasets analyzed during the current study are from the Global Burden of Disease Study 2021 (GBD 2021, https://doi.org/10.31981/GBD.2021.0), publicly accessible via https://vizhub.healthdata.org/gbd-results/ with no access restrictions. The R code used for BAPC modeling and statistical visualization is available from the corresponding author (Min Wu, E-mail: minwoo2022@126. com) upon reasonable request.
Funding
This work was supported by funds of the Key Research and Development Grant of MOST (2023YFA095000), the Affiliated Xiangshan Hospital of Wenzhou Medical University, the National Science Foundation of China (82470005) and Wenzhou Institute University of Chinese Academy of Sciences.
Authors’ contributions
Min Wu (MW) provided funding support, critical revision of the manuscript, and study supervision. Zhenwei Xia (ZX) and Qun Wu (QW) served as corresponding authors and reviewed the manuscript. Yujiao Wu (YWu) revised the manuscript. Huabin Zhu (HZ) and Yajin Wen (YW) contributed equally to this work and are co-first authors. Huabin Zhu (HZ) drafted the initial manuscript. Yajin Wen (YW) analyzed the data and performed statistical analyses. All authors (HZ, YW, MW, ZX, QW, YWu) read and approved the final version for publication.
Acknowledgments
The authors thank the support of Skill Learning from Kaixin Doctor and MASCU (Medical Association with Science, Creativity, and Unity), Inc, Shenzhen, China (mascu_forever@163.com). We also thank members in our laboratory for helpful discussion.
REFERENCES
- Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018; 391: 783-800.
- Global Initiative for Asthma (GINA). Summary Guide for Asthma Management and Prevention 2024. Geneva: Global Initiative for Asthma, 2024.
- Martinez A, de la Rosa R, Mujahid M, Thakur N. Structural racism and its pathways to asthma and atopic dermatitis. J Allergy Clin Immunol. 2021; 148: 1112-1120.
- Shin YH, Hwang J, Kwon R, Lee SW, Kim MS, GBD 2019 Allergic Disorders Collaborators, et al. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Allergy. 2023; 78: 2232-2254.
- Gorham TJ, Tumin D, Groner J, Allen E, Retzke J, Hersey S, et al. Predicting emergency department visits among children with asthma in two academic medical systems. J Asthma. 2023; 60: 2137-2144.
- Hurst JH, Zhao C, Hostetler HP, Ghiasi Gorveh M, Lang JE, Goldstein BA. Environmental and clinical data utility in pediatric asthma exacerbation risk prediction models. BMC Med Inform Decis Mak. 2022; 22: 108.
- Hogan AH, Brimacombe M, Mosha M, Flores G. Comparing Artificial Intelligence and Traditional Methods to Identify Factors Associated With Pediatric Asthma Readmission. Acad Pediatr. 2022; 22: 55-61.
- Patel SJ, Chamberlain DB, Chamberlain JM. A Machine Learning Approach to Predicting Need for Hospitalization for Pediatric Asthma Exacerbation at the Time of Emergency Department Triage. Acad Emerg Med. 2018; 25: 1463-1470.
- Gaillard EA, Kuehni CE, Turner S, Goutaki M, Holden KA, de Jong CCM, et al. European Respiratory Society clinical practice guidelines for the diagnosis of asthma in children aged 5-16 years. Eur Respir J. 2021; 58: 2004173.
- Votto M, De Silvestri A, Postiglione L, De Filippo M, Manti S, La Grutta S, et al. Predicting paediatric asthma exacerbations with machine learning: a systematic review with meta-analysis. Eur Respir Rev. 2024; 33: 240118.
- Nanda A, Baptist AP, Divekar R, Parikh N, Seggev JS, Yusin JS, et al. Asthma in the older adult. J Asthma. 2020; 57: 241-252.
- Taherian MR, Fatemian F, Halimi A, Soleimani Y, Jorjani G, Nozari P, et al. Prevalence of asthma among children and adolescents in WHO’s Eastern Mediterranean Region: a meta-analysis of over 0.5 million participants. BMC Public Health. 2024; 24: 2148.
- Adal O, Mamo ST, Belay AE, Tsehay YT, Netsere HB, Mulatu S, et al. The prevalence of asthma and its predictor among patients presetting in Ethiopian public hospitals: systematic review and meta-analysis, 2024. Ther Adv Respir Dis. 2024; 18: 17534666241275336.
- Mattiuzzi C, Lippi G. Worldwide asthma epidemiology: insights from the Global Health Data Exchange database. Int Forum Allergy Rhinol. 2020; 10: 75-80.
- Serebrisky D, Wiznia A. Pediatric Asthma: A Global Epidemic. Ann Glob Health. 2019; 85: 6.
- Stern J, Pier J, Litonjua AA. Asthma epidemiology and risk factors. Semin Immunopathol. 2020; 42: 5-15.
- Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. J Clin Invest. 2011; 121: 2111-2117.
- Elnaggar RK, Osailan AM, Alghadier M, Elnegamy TE, Morsy WE, Abdrabo MS, et al. Exercise strategies for reversing cardiopulmonary deconditioning in obese children with bronchial asthma: A randomized comparative effectiveness study of constant-load and graded aerobic training. Medicine (Baltimore). 2024; 103: e40667.
- Makrufardi F, Manullang A, Rusmawatiningtyas D, Chung KF, Lin SC, Chuang HC. Extreme weather and asthma: a systematic review and meta-analysis. Eur Respir Rev. 2023; 32: 230019.
- Beggs PJ. Thunderstorm Asthma and Climate Change. JAMA. 2024; 331: 878-879.
- Liu K, Hua S, Song L. PM2.5 Exposure and Asthma Development: The Key Role of Oxidative Stress. Oxid Med Cell Longev. 2022; 2022: 3618806.
- Han Q, Gao X, Wang S, Wei Z, Wang Y, Xu K, et al. Co-exposure to polystyrene microplastics and di-(2-ethylhexyl) phthalate aggravates allergic asthma through the TRPA1-p38 MAPK pathway. Toxicol Lett. 2023; 384: 73-85.
- Xu Q, Zhou Q, Chen J, Li T, Ma J, Du R, et al. The incidence of asthma attributable to temperature variability: An ecological study based on 1990-2019 GBD data. Sci Total Environ. 2023; 904: 166726.