Use of Semaglutide for Successful Weight Loss and Maintenance in a Non-Obese Population: An Observational, Retrospective Chart Review
- 1. NYC Plastic Surgeon, USA
Abstract
Objectives: This retrospective chart review aimed to assess the efficacy of compounded semaglutide, the active ingredient of an FDA-approved weight loss drug for patients with obesity, for weight loss in otherwise healthy, regular, and overweight people (BMI < 29.9). Additionally, a novel method to declare the ideal or target weight, which bridges the difference in body composition, bone structure a sex is proposed. Achieving a target weight is also proposed to measure the success of the elective weight loss (EWL™) program.
Methods: An internal, retrospective chart review was conducted to assess the efficacy and success of an Elective Weight Loss (EWL™) program. Weight was collected on 326 patients (male n=23, female n=303), with a mean age of 42.2 years, for 12 to 120 weeks. Weekly doses, dose adjustments, when semaglutide was stopped, when the target weight was attained, and weight maintenance were collected. No diet was prescribed.
Results: The results showed that 96% of the patients lost weight. Five patients gained weight, and seven lost no weight. In non-obese patients (n = 233), the mean start BMI was 25.44 ± 2.6 (20-28), and the end mean BMI was 22.99 ± 2.55, p-value <0.001. Obese patients (n = 93) mean BMI was 34.98 ± 4.6, a mean end BMI of 30.72 ± 4.98, p-value <0.001.
Conclusions: It was concluded that compounded semaglutide was found to be a safe and highly effective off-label option for elective weight loss in normal and overweight individuals. It promotes weight loss at lower doses and shows potential benefits comparable to moderate calorie restriction in improving cardiometabolic health and supporting anti-aging in non-obese people.
Keywords: Non-Obese; Semaglutide; Weight Loss; Successful Weight Loss
Introduction
Obese patients suffer from a high prevalence of serious obesity-related illnesses, including diabetes, hypertension, dyslipidemia, heart disease, stroke, sleep apnea, and cancer, and impose 147 billion in costs on the healthcare system annually in the US. Obesity in the United States was 40.3 % from 2017 to March 2O2O. It is predicted that by 2030, nearly 1 in 2 adults will have obesity [1]. Nationally, severe obesity is likely to become the most common BMI category among women, non-Hispanic black adults, and low-income adults [1]. In addition, cardiovascular disease (CVD) is the leading cause of worldwide morbidity, disability, and death [2]. An average of one American dies every 33 seconds from cardiovascular disease. Heart disease costs about 252.2 billion from 2019-2020 in the US [3].
The tragedies of delayed weight loss are obesity-induced illnesses such as type II diabetes and co-morbidities including coronary artery disease, hypertension, elevated blood lipids, fatty liver, and painful neuropathies. An extensive review and meta-analysis determined statistically significant associations between obesity and overweight (BMl> 25) with the incidence of type II diabetes, all cardiovascular diseases (hypertension, coronary artery disease, stroke, pulmonary embolus, except congestive heart failure), all cancers (except esophageal, pancreatic and prostate cancers), asthma, gallbladder disease, osteoarthritis, and chronic back pain [4]. The non-obese population that is overweight relative to themselves (approximately 10% over their normal, low adult weight) will likely also benefit from weight loss. This study addresses the potential physiologic, psychological, and preventative benefits of weight loss in a non-obese population. This observational study aims to show the high efficacy of compounded semaglutide for weight loss in normal to overweight patients and present anecdotal evidence of physiologic and psychological improvement in this lesser-studied population. Participants may benefit from potential weight loss, improved metabolic health, and enhanced overall well-being through structured medical supervision and available nutritional support. The study may also contribute to a better understanding of the effectiveness and safety of semaglutide in individuals who have struggled with weight loss through conventional methods. From a societal perspective, the findings could help refine elective weight management practices and provide insights into the off-label use of semaglutide. Additionally, the study may support more informed decision-making for healthcare providers and patients considering similar treatments. Overall, the research aims to advance knowledge in medical weight management while promoting safe and effective treatment approaches. Many Americans strive for weight loss and maintenance. The GLP-1 peptides have been proven to be very effective in weight loss for the obese population. Overweight, non-obese patients also strongly desire to return to their normal adult weight. I propose that modest weight gain (8-25 pounds), generally 5-15% of a person’s stable, low adult weight, should be viewed as a person being “overweight” relative to themselves. Gains above and returning to their “normal” lower weight likely correlate with elevation or decrease in cardiovascular disease risk factors (20-21). A method for determining a person’s target/goal weight is also proposed with an accompanying ‘success zone’.
The current state of research
Human studies observed that calorie restriction (CR) protects against multiple atherosclerotic risk factors [5]. Calorie restriction (CR) is defined as lessening caloric intake without depriving essential nutrients [6], and results in changes in molecular processes that have been associated with ageing, including DNA methylation (DNAm) (7-9). Moderate CR diet improved multiple cardiometabolic risk factors in healthy, young, and middle-aged non-obese men and women, as is similarly seen in weight loss studies on people with obesity [2]. A post hoc analysis of the blood samples from this same group found that the CR slowed the pace of ageing [7]. Moderate and other calorie-restricted diets may promote anti-ageing adaptations and are established to increase healthy lifespans in multiple species [5-9]. All the above considerations reinforce the importance of individuals maintaining their low normal weight.
Specific aims of the review
1. To evaluate the effectiveness of the compounded semaglutide for weight loss.
2. To study the effects of the use of compounded semaglutide in healthy people who are normal or overweight (BMI less than 29.9).
3. To evaluate safety, efficacy, extent of weight loss with likely consequential health benefits.
4. To propose a novel method to declare the ideal or target weight which bridges the difference in body composition, bone structure and sex. Achieving a target weight is also proposed to measure the success of the weight loss program. The 'success zone' is defined as within 75% of the target weight.
The primary review question
What is the change in weight following a non-obese (BMl < 29.9) patient taking semaglutide over 3-24 months?
Materials and Methods/Study Design
Retrospective Cohort Study Design
This study employed an internal, retrospective chart review. It is a non-randomized, non-blinded, cohort design. It was conducted at Dr. Sharon Giese’s surgery medicine practice in New York City from May 2022 to October 2024. Ethical guidelines were adhered to throughout, and the primary aim was to evaluate the effectiveness and safety of compounded subcutaneous semaglutide in promoting weight loss and weight maintenance among a non-obese adult population (BMI < 29.9). the non-obese population will compared to an otherwise healthy obese population.
Intervention which was assessed
The single intervention assessed was the administration of compounded semaglutide via subcutaneous injection. Participants self-administered the drug at dosages aligned with FDA-approved guidelines. The intervention was part of the physician’s structured elective weight loss (EWL™) program that includes: Weekly weight tracking, adherence to regular coaching, continuous medical oversight for safety and adherence, weekly follow-ups (email and in-person or virtual), detailed education on semaglutide’s risks, side effects, and management strategies. Patients remained on semaglutide until they reached their target weight, after which the dose is tapered based on individual maintenance success. Participants could discontinue the medication at any time. The protocol for the compounded semaglutide medication with cyanocobalamin (B12) (5/ 0.5mg/1cc) was to generally inject 0.25mg or 5 units of medication subcutaneously into your thigh or abdomen, once weekly and check in with the office or nutritional coach to titrate the dose for appetite suppression, dosing and timing was adjusted as necessary to achieve appetite suppression and weight-loss. The weekly check in’s encouraged compliance. No refills were given without a current weight and dose. The medication was sourced from accredited 503 A and B pharmacies.
Success Zone and Weight Goals
A unique “Success Zone” was established for each participant. This range, defined as achieving 75% or more of the desired weight loss, allows a buffer for acceptable weight regain. It also establishes a threshold for reinitiating treatment if weight maintenance fails. For example, for a participant with a starting weight of 150 pounds and a target of 130 pounds, the success zone would be defined as 130–135 pounds. This goal-setting strategy emphasizes patient involvement and realistic, sustainable outcomes rather than rigid adherence to BMI charts.
Inclusion and Exclusion Criteria
Inclusion Criteria: Must be an adult aged 21 years or older, individuals unable to reach target weight via other methods, had consent to treatment, were taking semaglutide for at least 3 months, agreed to self-administered semaglutide off-label with full understanding of risks. All genders were offered treatment and there was no restrictions to social economic status. Exclusion Criteria: Pregnant or breastfeeding women, people with type 1 or type 2 diabetes, metformin use, or other chronic conditions. It was mandatory for participants to be classified as over their normal weight, overweight or obese based on BMI (>18.5 and < 40), or individuals with weight concerns relative to their personal health goals. People with a history of eating or severe gastrointestinal disorders were also not allowed. Additionally, people with adverse reactions to GLP-1 agonists.
Sample Size and Recruitment
There was no recruitment. All patients were treated electively and could not lose weight by any other means. The sample size was informed by a comparable 2-year randomized controlled trial on caloric restriction in non-obese adults (n=220)[2]. Both men and women aged 21–85 years were included.
Informed Consent
All patients had a written informed consent after receiving comprehensive information about semaglutide, the treatment procedures, possible benefits and risks, and their voluntary right to withdraw at any time. The consent process included written materials, verbal discussions, and video-based education. There was no financial inducement; all patients were self-funded, and no insurance claims were made. HIPAA compliance was strictly maintained, with signed consent forms stored securely.
Data Collection and Follow-Up
Data was collected using a mix of methods: weekly self-reporting of weight, including a photo of their weight on a digital scale and semaglutide dosage, structured intake and follow-up forms, visual verification by the physician for regular patients, review of medical records for treatment adherence and adverse events, and periodic surveys assessing satisfaction, well-being, and treatment experience. Patients also completed intake forms that assessed medical history, sleep, alcohol consumption, use of psychiatric or diabetic medications, and body weight history. A target weight was determined collaboratively between the patient and doctor, generally above the patient’s historical low weight to ensure attainability.
(a) How patients were identified
To protect patient confidentiality during the chart review I will use codes to allow re-identification. This will not be included in the same data sheet as the health information. I will use a “correlation tool” to remove identifiers from the data and place them in a separate file which only has identifiers. The correlation tool will be destroyed at final publication/presentation of the study.
The use of a correlation tool is being requested to allow re-identification of subjects. This request is being made for three main reasons. 1) In the case of data transcription error, I may need to go back to the medical record to correct the errors. 2) upon submission of the work for publication, a reviewer may request additional data to strengthen the study. 3) The medical charts are of active patients in my private practice.
(b) Who will collect data and from where
The office manager, staff, nutritional coach and the PI recorded weight and dose changes in the patient’s chart. All were trained and observed performing their task. The PI verified accuracy with periodic monitoring. The data abstraction or “correlation tool” was done on a Google doc to remove ALL identifiers. This separate Google doc was then given to the statistician, on a Google doc that could not be altered. The statistician only analyzed changes in weight over time.
Monitoring and Safety Measures
There was no monitoring for the chart review. When patients were treated the practice ensured 24/7 access to Dr. Giese for medical support. Commonly expected side effects such as nausea, gastrointestinal discomfort, or temporary appetite suppression were discussed thoroughly during intake and monitored through regular follow-ups. Patients were provided education on managing side effects, and dose adjustments were made in response to complications or slow weight loss progress.
Data Management and Confidentiality
All patient’s data was anonymized using unique ID codes. Each participant was assigned a unique number. The patient’s name and number are stored on the practice's private server which is backed up on a cloud with firewalls. Confidential information will be securely stored and back up on a private server in the building and is backed up with end-to-end encryption. The terminals are password-protected, with access restricted to the principal investigator and authorized research staff. Electronic data was stored in encrypted, password-protected systems with access limited to authorized research staff. Physical documents are kept in locked storage within secure offices. Data analysis was done in accordance with the current ethical and legal standard. Data will be retained and eventually destroyed by ethical and legal standards. HIPAA compliance protocols were strictly followed to ensure participant privacy and data integrity.
Risk and Benefit Analysis
The main risk is to data confidentiality, which has been addressed above. As this is a retrospective chart review, there are no privacy risks because there will be no interaction or intervention with subjects. The potential risks associated from taking semaglutide were minimal but included mild physical side effects such as nausea, vomiting, abdominal pain, diarrhea and constipation. Serious side effects can include pancreatitis, changes in vision, low blood sugar, allergic reactions, gallbladder problems and/or stomach paralysis. Risks were assessed differently based on participant characteristics. Psychological risks may involve feelings of frustration or disappointment if expected weight loss outcomes are not achieved. The PI assessed basic psychological competency before study enrollment, particularly regarding body dimorphic disorders. If excessive unanticipated psychological effect occurred following weight loss or failure to do so, they were addressed on an immediate, individual basis. Any suicidal ideation would be referred to the Emergency Department. Patients will benefit from potential weight loss, improved metabolic health, and enhanced overall well-being through structured medical supervision and nutritional support. The report may also contribute to a better understanding of the effectiveness and safety of semaglutide in individuals who have struggled with weight loss through conventional methods. The report will expand the use of semaglutide in non-obese people and explores the likely health benefits derived from its use. From a societal perspective, the findings could help refine elective weight management practices and provide insights into the off-label use of semaglutide. Additionally, the study may support more informed decision-making for healthcare providers and patients considering similar treatments.
Statistical Analysis
Unless otherwise indicated, continuous variables will be analyzed using Welch’s Two Sample t-tests and categorical variables were analyzed using Pearson’s Chi-squared test. A Shapiro-Wilke test of starting and current weight produced a p value of< 0.001, indicating the data is normally distributed (a prerequisite for paired t-testing). In this study the unit of analysis is the individual patient, which is also the unit of treatment assignment; therefore, no additional adjustment (e.g. design effect correction or multilevel modeling) was required. Additional analyses will be conducted using stratified subgroup comparisons—employing paired t-test for continuous outcomes and chi-square tests for categorical outcomes—with descriptive statistics presented via summary tables. No complex multivariable adjustment was required beyond this stratification. Subgroup analyses will be performed by stratifying the sample by key variables (e.g. obesity status, gender) and conducting paired t-tests and chi-square tests for group comparisons; any adjusted analysis was accomplished by comparing these stratified groups rather than fitting formal multivariable models. All analyses were performed using the statistical software R.
As previously described, all participants’ data was kept confidential, encrypted, password-protected, with very limited access. The statistics were performed remotely with anonymized copies of the raw data. The original data could not be altered by the statistician, as that type of access was not given to her.
Cost to Subjects
None
Results
Outcome
The total number of patients was 326. A summary of the study patient population can be seen in Table 1. 96% of the patients lost weight (314/326). 1.5% (5/326) gained weight, and 2.1% (7/326) did not lose weight. 0.6% (2/326) could not tolerate the medication, as shown in Table 2. There was no statistical difference in weight loss between the men and women in the group, as shown in table 2a, and no statistical difference between the obese and non-obese patients, as shown in Table 2b. The mean weight loss was 18.16 (13.61) in pounds, and the standard deviation (SD) was. The starting mean BMI was 28.16 (5.43). The current BMI is 25.19 (4.89) as shown in table 3. Additionally, the weight loss was divided into the percentage of starting body weight lost as per Table 3 and Figure 1-2. The change in the amount of weight, in pounds, and
the BMI change was statistically significant, with p-value <0.001, for both female and male patients as shown in table 3a and figure 2a, and non-obese and obese patients in Table 3b and Figure 2b. 25% of the patients achieved their target weight, and 47% entered or stayed in the success zone (Table 4). There was no statistical difference by gender for those who achieved target weight or were in the success zone, as shown in Table 4a. Just over half of the non-obese patients and about one-third of the obese patients have entered the success zone Table 4b. At the same time, 80% of study patients have achieved 5% or greater weight loss to date (Table 3). Most (93%) of patients in the success zone are still on medication. Most patients in the success zone (79%) have lost more than 10% of their starting weight (Table 4c). The amount of time spent on the medication is shown in Table 5. Since this is an ongoing, rolling study, a given time frame shows how long we have followed an individual or how long they have been on semaglutide and are still in the process of losing weight. The amount of time spent on medication is relatively similar for the obese and non-obese populations, Table 5a. 2/326 (0.6 %) stopped the semaglutide due to complications of nausea and stomach cramping.
Side effects
Side effects were transient (1-4 weeks at onset) or when medication dosing was increased to attain appetite suppression and weight loss. 13% nausea, 3% vomiting, and 2% diarrhea and abdominal cramping. 18.5% (60/326) of patients requested Zofran. Anecdotally, more patients who requested Zofran were under 30 years old and seemed to want it ‘on hand’ when they were out drinking alcohol. The average weekly dose of semaglutide was 0.83mg (0.25-2.4mg). No incidence of infection was observed with the use of multi-dose vials. No person reported ‘cloudy’ medication before using the vial. There was no evidence of patients overdosing. One thousand one hundred twenty-nine vials were ordered from May 2022 to October 2024.
Table 1
Table 1: Summary of the Patient Population
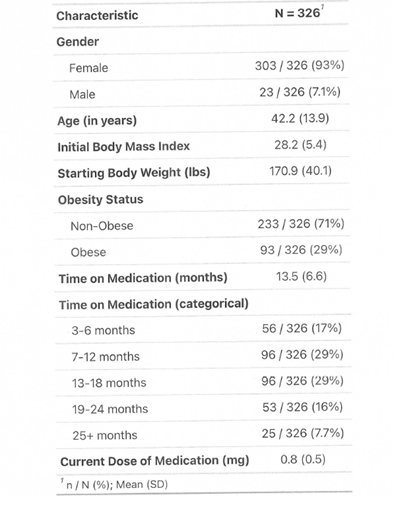
Table 2
Table 2: Population Weight Loss Characterization
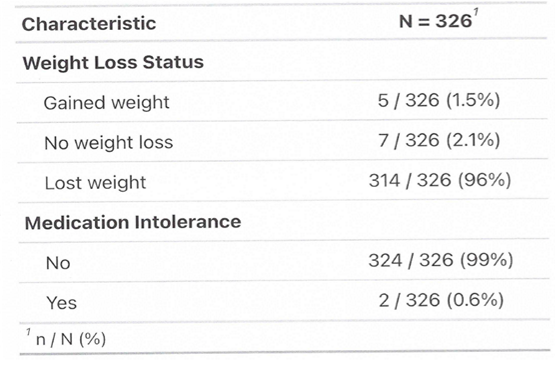
Table 2a
Table 2a: Weight Loss Characterization by Gender
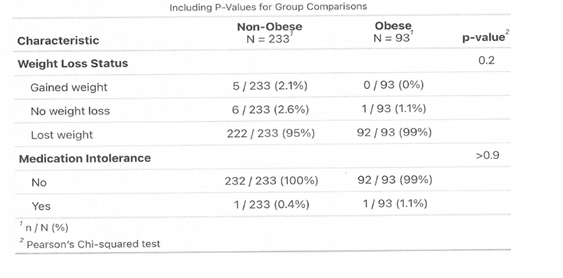
Table 2b
Table 2b: Weight Loss Characterization of Obese and Non-Obese Populations
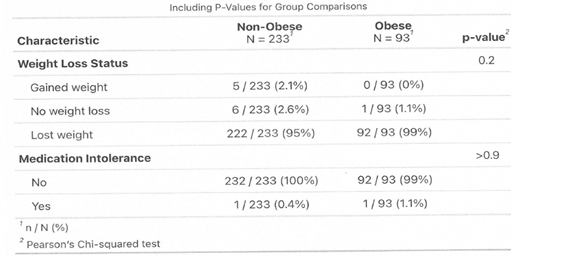
Table 3:
Table 3: Amounts of Weight Loss
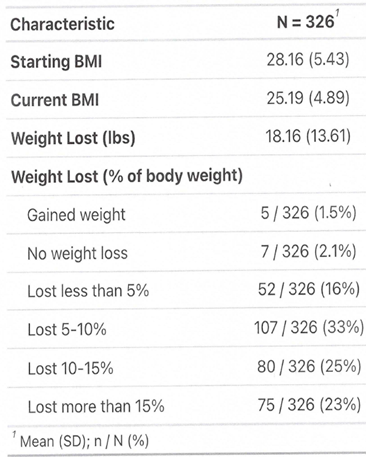
Table 3a: Amounts of Weight Loss by Gender
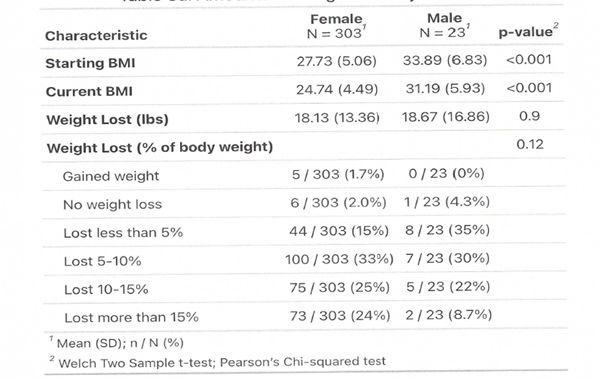
Table 3b
Table 3b: Amounts of Weight Loss for Obese and Non-Obese Populations
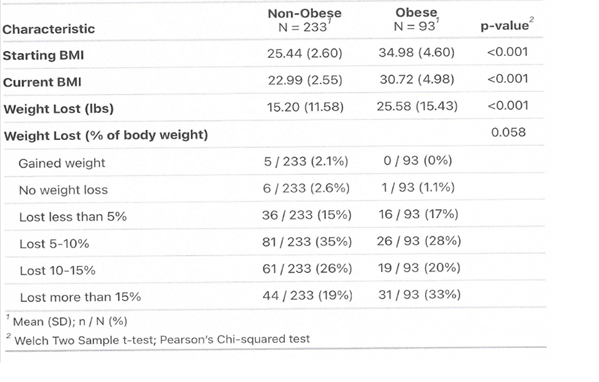
Table 4
Table 4: Defining the Success of the Elective Weight Loss Program
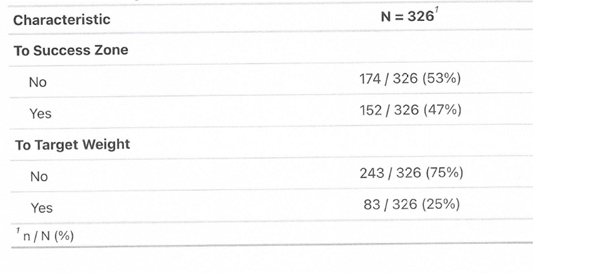
Table 4a
Table 4a: Defining the Success of the Elective Weight Loss Program, by Gender
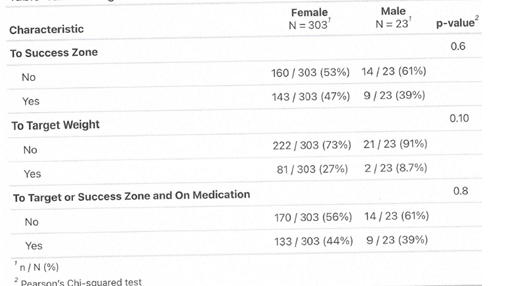
Table 4b
Table 4b: Defining the Success of the Elective Weight Loss Program for Obese and Non-Obese Populations
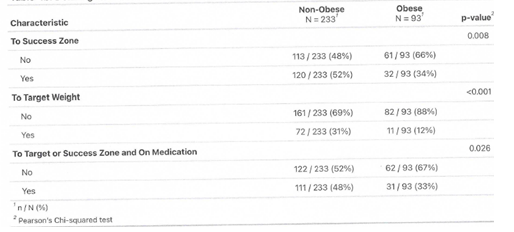
Table 4c
Table 4c: Percentage of Weight Loss in the Success Zone.
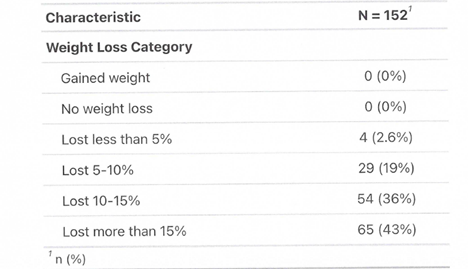
Table 5:
Table 5: Amount of Time on Medication
Table 5a
Table 5a: Amount of Time on Medication for Obese and Non-Obese Populations
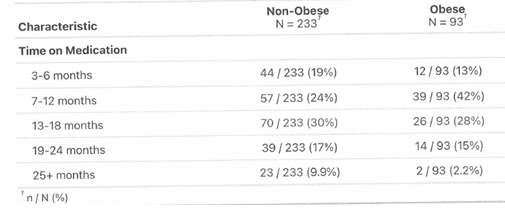
Figure 1
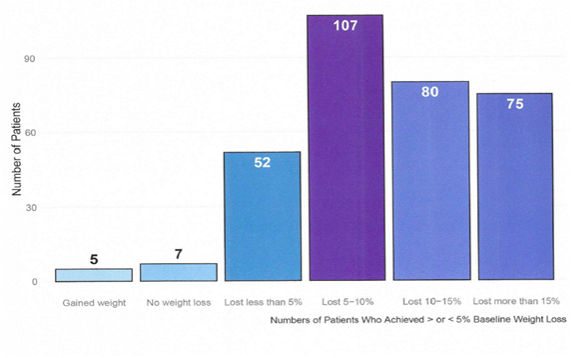
Figure 1: Percentage Weight Loss from Baseline in Elective Weight Loss Program
Figure 2
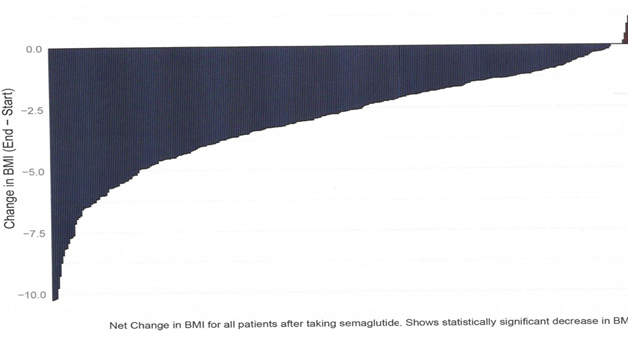
Figure 2: Net Change in BMI for each Patient
Figure 2a and 2b
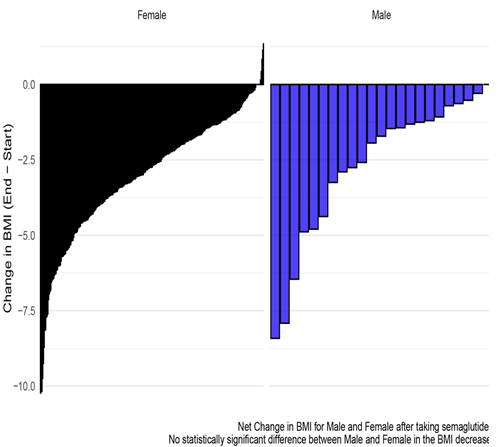
Figure 2a: Net Change in BMI by Gender
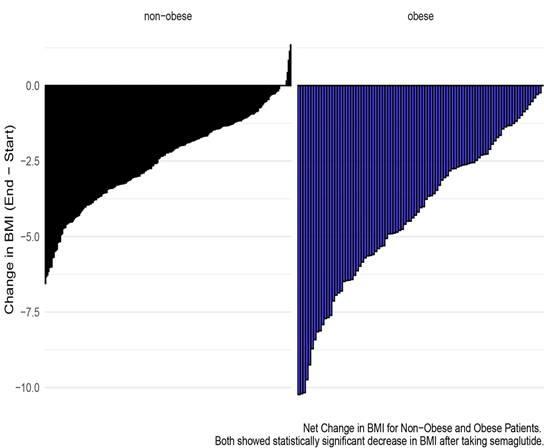
Figure 2b: Net Change in BMI by starting Obesity Status
Discussion
Most of the studies on weight loss and the risks of obesity are understandably conducted on the obese population. Those individuals are likely already in a diseased, inflammatory state and not a comparable population to those at a normal weight (BMI <25) or even otherwise healthy, overweight, or non-diabetic people (BMI < 29.9). Notable weight loss in the obese population has conferred improved health benefits and risk factors for coronary artery disease, hypertension, and lipid profiles [2,10,46-48]. An extensive review and meta-analysis determined statistically significant associations between obesity and overweight (BMI> 25) with the incidence of type II diabetes, all cardiovascular diseases (hypertension, coronary artery disease, stroke, pulmonary embolus, except congestive heart failure), all cancers (except esophageal, pancreatic and prostate cancers), asthma, gallbladder disease, osteoarthritis, and chronic back pain [11]. Maintaining a healthy weight could be important in preventing the large disease burden and significantly impacting health expenditures. Obese patients suffer from a high prevalence of serious obesity-related illnesses, including diabetes, hypertension, dyslipidemia, heart disease, stroke, sleep apnea, and cancer, and impose $147 billion in costs on the healthcare system annually in the US [2]. More recently, several STEP studies [12], have demonstrated that the magnitude of weight loss reported in STEP trials offers the potential for clinically relevant improvement for individuals with obesity-related diseases [12-20]. A recent, very controlled study implementing moderate calorie restriction in non-obese men and women with a clinically normal baseline showed improvements in six cardiometabolic risk factors—reduction in LDL-C, increase in HDL-cholesterol concentration, reduced serum TG, lower systolic blood pressure, reduction in BMI, reduction in Met syndrome Z-score and AUC insulin [2]. Normal risk factors were already improved at the 2-year post-implementation of the CR diet. The improvement in long-term cardiovascular risk was implied [2]. The calorie restriction compliance was aided by intensive, weekly behavioral therapy and food and calorie calculation support. Without such support, compounded semaglutide may be a good alternative and adjunct to achieving calorie restriction and weight reduction. CR has been shown to reduce inflammatory markers TNF-α and CRP in non-obese humans [1]. Sustained CR was feasible in humans and sufficient to affect some potential modulation of longevity that CR has also induced in laboratory animal studies or adults [37-40]. This, in turn, likely diminishes risk factors for age-related cardiovascular and metabolic diseases and enhances human life span [5,21]. A recent report of two years of sustained CR in humans positively affected skeletal muscle quality, and gene expression changes induced by CR partially mediate preserving muscle strength [11].
I propose that people in the traditionally normal weight population (BMI <25) and non-diabetic, overweight adults (BMI< 29.9) will equally benefit from weight loss to a target weight, around their low weight as an adult, with the aid of semaglutide. Multiple cardiometabolic risk factors are reduced in the obese and non-obese populations with weight loss by calorie restriction [11,28]. Semaglutide has also been used as an adjunct to increase the magnitude and efficacy of weight loss with attendant medical benefits [11]. I propose the successful, efficacious weight loss in the non-obese population of this study, with the aid of semaglutide, improved cardiometabolic risk profiles as in the CALERIE study [2].
As a body contour expert, I have used this target weight benchmark for over 20 years to establish an individual's "normal weight." When assessing all my body contour patients, I always ask about a person's adult high, low, and ideal body weight. In general, those values are quickly answered. It seems that most people intuitively know their "healthier" Weight and set their ideal at a little higher than their lowest Weight. Therefore, attaining a "target weight" is not a benchmark for a program's weight loss success or effectiveness. Success or effectiveness has been expressed as a per cent decrease from the start weight, a reduction in BMI, a decrease in waist circumference, improvements in health outcomes (blood pressure, cholesterol levels, and insulin sensitivity), and participants' satisfaction. The results in this study are analyzed in three ways: 1) statistically significant weight loss, relative to themselves, 2) the percent decrease in body weight loss at <5%, 5-10%, 10-15%, and >15%, and 3) statistical decrease in the BMI. Patients who achieved and maintained 75% progress toward the target weight or, following attaining the target weight, do not regain more than 25% of the weight loss, are designated in the "Success Zone." This target weight is patient-centric and patient-motivated. It does not rely on the BMI chart. Achieving 10% of body weight loss generally correlates with improved health profiles. However, obese and non-obese patients may have weight goals that are beyond that. In this case, the target weight is essential, as I recommend that patients stay on the medication until they reach the target. Just losing Weight is not necessarily viewed as "success." To further justify using the target weight and 'success zone,' we compared the patients who achieved that status to typical milestones of success with weight loss medications and per cent body weight loss. 79% of patients in the "Success Zone" have lost 10% or more of their start weight, and people with more minor total losses, < 10%, had smaller weight-loss targets (Table 4c). Medical benefits have been noted with as little as 5 per cent weight loss [12]. 81% of the study patients have achieved 5% or greater weight loss (Table 3).
Multiple studies have questioned the BMI stratification. While there are likely gross triage benefits today, the BMI scale was not intended for individualized clinical use but rather to define the average Weight of a population [21]. I use it simply as a benchmark and quantify the weight change within each individual in the study group. The fact that the BMI scale lacks overall clinical relevance supports my question about the ideal body weight for any given person. Determining the target weight was used as another benchmark of the success of any individual's weight loss and is intended to supplant the traditional standard BMI definitions of normal Weight (BMI 18.5-24.9) or overweight (BMI 25-29.9).
I have a unique window into an ageing, very disciplined, accomplished, and generally healthy female population. Over the years, I have seen many patients struggle to maintain Weight and/or achieve weight loss. They have many resources at their disposal and a multibillion-dollar weight loss industry. Their failure to achieve their weight goal motivated me to explore why. If it were so easy to stay near a lower weight, more people would be there and not be trying to lose.
A prescription for weight loss is hardly one size fits all. Western medicine generally prescribes "calorie restriction and exercise." Anyone who has tried to lose Weight and failed knows this is easier said than done. Longitudinal/population studies have shown that weight loss and maintenance in the obese population fail miserably over time [22]. There is also high recidivism and minimal success for commercial and community-based weight loss programs [23,41]. A study evaluating only the most successful and overweight Weight Watchers® members found that 50% maintained at least 5% of their weight loss over 5 years [24]. Weight loss interventions are generally multifaceted, costly, aggressive, and dramatic changes forced onto a person, all of which may contribute to failure. Given high failure rates or simply the lack of transparency with the results or success, it begs for higher, more reproducible standards to evaluate weight loss.
The simple answer to high failure rates is that it is challenging to stay on a restricted calorie diet for a sustained period [25-31]. Weight loss generally takes longer than one thinks to achieve. Then, there is weight maintenance, which is usually considered to be equally as hard [32-36]. Incredibly, weight gain is often ignored by primary care physicians until a person reaches an obese level. Even then, in the face of a diseased state, perhaps pre-diabetic, in many cases, no recommendation for treatment is made [42-46]. Gradually, weight gain is generally accepted as people age. While many factors contribute to weight changes, one known one is that muscle mass decreases (in most cases) with advancing age, particularly in women over 60. This would then lead to a weight reduction as we age, not a weight gain. All the patients studied failed to achieve their ideal body weight by other means and opted to try compounded semaglutide to lose Weight. An additional anecdotal comment repeated by patients that I believe contributes to its effectiveness is the reduction of 'food noise.' Some patients opted to stay on a low dose (0.25-0.5mg semaglutide weekly) as a maintenance dose to keep the 'food noise' away. Recently, this has been described as "microdosing". The food cue reactivity conceptual model is gaining credible scientific substantiation [42]. Evidence supports that weight loss increases appetite sensations, particularly to upregulate appetite in women [25]. This chart review indicated that the success of weight loss, aided by compounded semaglutide in non-obese individuals, was resounding. 96% of the 326 subjects lost Weight, with only one regaining Weight after stopping the medication. 81% of the total population achieved over 5 per cent of body weight, with nearly half of the patients still working towards their target weight. 18.5 % were lost to follow-up. I categorized my results for weight loss by per cent of weight loss, similar to the graded improvement of 5%, 10%, 15%, and over, lost in obese populations, which results in escalating health benefits [10]. The target is health improvement, including quality of life or health-span. It is likely then that a CR diet, with resultant weight loss of 5 to more than 15 %, will confer similar, positive health benefits by reducing obesity-induced risk factors. The addition of the 'Success Zone' offers a measure of the success and effectiveness of the program. Patients enter the 'success zone' when they achieve and maintain at least 75% of their weight loss goal to a target weight. This will hopefully encourage patients to reach their goals and keep them aware of any weight regain. If they fall out of the zone, they should be vigilant before losing more ground and yo-yoing their weight loss. The weight loss success occurred without infection or overdosing. I found patients very competent to manage using a multi-dose vial, where injections were self-administered. They were empowered by that and motivated not to have side effects. Hence, no overdosing, which would not only be costly but also uncomfortable. I believe the patients were very motivated to succeed in the most expeditious way to save money. This also motivated patients to be able to go off the medication or maintain a very low dose of 0.25mg every 7-14 days.
In the future, we may have patients utilize Bluetooth scales to capture the data in real time instead of having patients photograph the digital Weight and send it. I expect that will result in more data points, as this would aid in strengthening the data, which is partly self-reported. However, since all were current patients in my practice, we had the visual advantage of checking on patients. It was more likely that we updated weights that they had not reported on patient visits, which were generally lower than the previous number. Having a placebo group of two is not ideal; however, we could not identify anyone to chance not getting medication. We did not study whether the dose of semaglutide correlates with the patients appetite suppression and overall satisfaction with the program. We are in the process of obtaining this feedback through a post-participation survey. It is difficult to discern if adherence to the program's guidelines (weekly follow-ups, dose recommendations) influences weight loss outcomes. The post-participation survey may also address this in the future.
Dosing was significantly lower than dosing regimens recommended by Ozempic® and Wegovy® in the obese population, which routinely ramp up to 2.4 mg weekly. The average dose for patients was 0.84 mg weekly semaglutide (0.15 to 2.4 mg). At those doses, patients were losing Weight at a rate of ½ to 2 pounds a week. This was a predictive tool to estimate how long patients would be on the medication. I then estimated patients would stay on the medication for another 6-8 weeks to ensure a stable weight at the target. Then, we would start to wean patients off the drug by decreasing 2-5 units or 0.1-0.25 mg a week. Decreasing dosing would proceed as long as the Weight stayed stable. Some patients opted to stop once their target was achieved. Given the long half-life of semaglutide (1 week), simply stopping yields a taper-off over 5-6 weeks, with no intervention.
Some patients lost 30 pounds of Weight with 0.25-0.5 mg of semaglutide weekly. In those cases, just being smaller cannot explain the lower doses. In general, I found dosing needed to be customized. Some larger patients were successful on low doses, and smaller ones needed 1.25 to 1.5 mg weekly. A smaller percentage of the patients advanced to 2.4 mg/week to achieve the target weight. If weight loss stalled at high doses of semaglutide, the patient was changed to tirzepatide, 29/326 patients. I believe this type of lower, customized dosing conferred a lower complication rate, particularly the worst one being vomiting.
Anecdotal health benefits include one patient being able to go off one of two hypertensive medications, and another having a significant reduction in the appearance of spider veins, indicating ease of venous return to the heart and possibly improved venous insufficiency. In contrast, patients reported increased energy and decreased joint pain. Another patient's sleep apnea completely resolved with a 35-pound weight loss. Previous studies show positive and negative psychological results [26]. Psychological effects may not be reliant on absolute weight loss. Viable study design for psychological benefits, subjects chosen, interventions, and the outcome is under investigation for obese and non-obese populations [26].
Additionally, many patients expressed appetite suppression after taking semaglutide, which helped control their portion. Once they learned the portion adjustments, they chose more nutritionally dense foods. Some scientists believe obesity rates have exploded in the past decades, at least in part due to the manipulation, ultra-processing, and quality of the food supply. Semaglutide appears to help get around food quality with portion control until we can solve this larger societal issue. Overwhelmingly, in the current study, all patients had improved body image and felt more satisfied with themselves. We will attempt to quantify these perceived psychological benefits in the future. One- and two-year results on a larger group will provide information on weight maintenance following the discontinuation of semaglutide and the possible return to semaglutide if some weight is regained. Since over 40% of the US adult population is obese, I believe adults should not gain more than 10% above their low weight as an adult unless an untoward medical condition is involved with that change.
The body is not static, meaning it changes over time. I liken this to the brain not being “hard-wired;” it is plastic and ever-changing. It appears that semaglutide aided a reduction and a reset in non-obese people’s weight without a feeling of deprivation. All patients ate and drank what they wished; by all reports, they just had less of it. By systematically documenting patient outcomes, this study contributes to the existing body of knowledge on semaglutide's efficacy in weight management and informs best practices for its use in clinical settings.
More than ever, an old medical adage of “anything in moderation” may hold here. Overconsumption in many aspects of life has become more commonplace in the advancing, industrious, seemingly abundant world. “Less is more” may never have been more relevant in our current divergent world. Is seeing and living the success of attaining the ideal weight goal an independent psychological benefit? Will that improvement motivate weight maintenance to adapt behavioral changes in the future? We will answer this in the future as we continue to follow this expanding pilot study group at 1, 2, 3, and 4 years.
Conclusions
The active ingredient of Wegovy®, an FDA-approved weight loss drug for obese patients, semaglutide, can safely be used off-label for highly effective elective weight loss in normal and overweight patients. It aids calorie restriction at significantly lower doses. A simple method to establish an individual’s ideal body weight is presented with a corresponding ‘success zone.’ Elective weight loss with compounded semaglutide in non-diabetic, non-obese individuals also likely improves cardiometabolic risk factors, promotes anti-ageing adaptations, and may be equally effective in achieving significant weight loss in non-obese people.
Patents
Funding: This research received no external funding.
Institutional Review Board Statement: The chart review was declared exempt by the Institutional Review Board (or Ethics Committee) of Beyond Bound IRB Approval Number: BB2503SG-083 (date of approval).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The author declares that the data supporting the findings of this study are available within the article.
Acknowledgments
Thank you to all the participating patients who provided follow-up data, Brenda Gloria and Kandice Watson for organizing and collecting the data, and Misty Knight-Finley, PhD, for statistics and graphics.
References
6. Speakman JR, Mitchell SE. Caloric restriction. Mol Aspects Med. 2011; 32: 159-221.
36. Sochovsky N, Miles H. Global Equity Observer GLP-1: The Weight of Speculation. Invest Insight. Morgan Stanley Investment Management. 2023.








































































































































