A Study of Association between Dose Fraction and Occlusion Rate in Hypofractionated Stereotactic Radiotherapy for Intracranial Cerebral AVMs
- 1. Department of Radiation Oncology, Saitama Medical Center, Saitama Medical University, Japan
ABSTRACT
Introduction: Intracranial cerebral arteriovenous malformations (AVMs) are congenital malformations. For patients with Grade ? or higher on the Spetzler- Martin grade, radiotherapy or vascular embolization combined with surgery is considered. Stereotactic radiosurgery (SRS) has been adopted for intracranial AVM and reported its high rate of obliteration and cure. However, intracranial AVM with large nidus volume is impossible to administer a sufficient prescribed radiation dose once, which leads to decreasing the obliteration rate. Recently, the effectiveness of hypofractionated stereotactic radiotherapy (HSRT) for AVM has been reported. We examined the relationship between the prescribed dose and obliteration rate in patients with intracranial AVM patients treated with HSRT and evaluated the proper dose fraction.
Materials and Methods: We retrospectively reviewed 23 patients. We investigated the correlation between obliteration rates and a) nidus volume, b) per-fraction prescription dose, c) number of fractions, and d) the biological equivalent dose (BED) with an α/β ratio of 3.
Results: Overall complete obliteration rate was 69.6%. When comparing the two groups with thresholds set at 4 ml and 10 ml, there was no significant difference in occlusion rates. The case group with a prescribed dose per fraction of >=7.5 Gy had a significantly higher nidus obliteration rate than that with a dose of <7.5 Gy. The 4-fraction case group had a significantly higher obliteration rate than the 5-fraction or more case group. In comparison with BED (α/ β=3) based on the linear quadratic equations (LQ model), dose of >=100 Gy (EQD2) was associated with higher obliteration rate comparing with dose of
<100 Gy, although the difference did not reach the significant level.
Conclusion: HSRT for intracranial AVMs performed at our institution showed an obliteration rate comparable to SRS without severe adverse events, although many of the patients had relatively large nidus.
KEYWORDS
- Intracranial cerebral AVM
- Hypofractionated stereotactic radiotherapy
- Large nidus volume
- Dose fraction
- Obliteration rate
CITATION
Utsumi N, Yamano T, Hayakawa T, Mizuno N, Ueno S, et al. (2024) A Study of Association between Dose Fraction and Occlusion Rate in Hypofractionated Stereotactic Radiotherapy for Intracranial Cerebral AVMs. J Radiol Radiat Ther 12(1): 1104.
INTRODUCTION
Intracranial cerebral arteriovenous malformations (AVMs) are congenital malformations consisting of a supply artery, nidus (abnormal vascular network) and draining vein, and AV shunting of the nidus is the main feature. Abecassis et al., computed 1.12 – 1.42 per 100,000 population per year de novo diagnosed AVMs [1]. AVMs are primarily detected by mainly bleeding (70%), also by convulsive seizures or headaches [2]. The objective of intracranial AVM treatment is to block blood flow into the nidus, leading to prevent bleeding or to improve neurological symptoms. Treatment strategies for AVMs are often determined by the Spetzler-Martin grade [3,4]. The first treatment strategy for intracranial AVMs of Grade ? or ?? on the
Spetzler-Martin grade is surgery. For patients with Grade ??? or higher, radiotherapy or vascular embolization combined with surgery is considered. Radiotherapy is especially recommended for patients whose nidus is located in an eloquent area, or for patients with small lesions that are difficult to be treated by direct surgical removal due to inflow vascular conditions or the presence of complications [5,6]. Stereotactic radiosurgery (SRS) has been adopted for intracranial AVM and reported its high rate of obliteration and cure [7-9]. SRS is the technique of radiotherapy with high accuracy, enabling give tumor high dose at one time. However, intracranial AVM with large nidus volume is impossible to administer a sufficient prescribed radiation dose once, considering for increasing adverse events of normal brain tissue, which leads to decreasing the obliteration rate. In fact, SRS for intracranial AVM with large nidus volume is known to have a lower obliteration rate [10]. Recently, the effectiveness of hypofractionated stereotactic radiotherapy (HSRT) for AVM with large nidus volume has been reported [11-17]. We offer HSRT for patients with intracranial AVM who are not eligible for neurosurgery or SRS. We examined the relationship between the prescribed dose and obliteration rate in patients with intracranial AVM patients treated with HSRT in our hospital and evaluated the proper dose fraction.
MATERIALS AND METHODS
We retrospectively reviewed 23 patients who underwent HSRT for intracranial AVMs at the Saitama Medical Center between 2004 and 2014. There were no exclusion criteria, and all 23 cases were included in the analysis.
Radiotherapy treatment planning
CT images for radiotherapy planning were acquired using a LightSpeed RT16 (GE Healthcare, Waukesha, WI, USA). BrainScan (Brainlab, AG, Heimstetten, Germany) was used for radiotherapy treatment planning. HSRT was performed with a Clinac 21EX (Varian Medical Systems, Inc., Palo Alto, CA, USA) with a tertiary m3 high-resolution mMLC (Brainlab, AG, Heimstetten, Germany). All patients were fitted with Frameless SRS Mask Set cranial (Brainlab, AG, Heimstetten, Germany) (Figure 1). Nidus was expanded by 1 mm to generate the planning target volume (PTV). Multi Leaf Collimator (MLC) margin was added appropriately to cover 90% of the PTV with the dose of 90% of the prescribed dose. We administered 100% of the prescribed dose to the center of PTV.
Figure 1 Frameless SRS Mask set cranial (Brainlab, AG, Heimstetten, Germany).
Treatment evaluation
Angiography was performed after HSRT to confirm whether nidus obliteration was achieved. In cases of the patients who were not suitable for angiography, contrast- enhanced Magnetic Resonance Imaging (MRI) or MR Angiography (MRA) was conducted. We investigated the correlation between obliteration rates and a) nidus
volume, b) per-fraction prescription dose, c) number of fractions, and d) the biological equivalent dose (BED) with an α/β ratio of 3. For analysis, we divided continuous variables into two groups as follownidus volume (>= 4ml and 10ml)
- prescription dose per fraction (>=7.5 Gy)
- a total number of fractions (>=5)
- BED (100 Gy (Equivalent Dose In 2 Gy fraction (EQD2)))
Statistical analysis
For analysis of the correlation between the two groups, the long-rank test was used for each index. All analyses were performed using R. Statistical significance was defined as p<0.05.
RESULTS
Patients
Patient characteristics are shown in Table 1. Mean age at treatment was 30.5 years (range, 4-68 years). The mean diameter of the nidus was 2.77 cm (1.0-4.3 cm), and the mean nidus volume was 7.76 ml (0.40-25.2 ml). As for AVM classification according Spetzler-Martin grade, 21 patients (91.3%; 21/23) were grade III or higher. The mean prescription dose was 33.8 Gy (28-40 Gy) and the mean number of fractions was 6.8 (4-13). The median follow-up period was 106 months (12-202 months). During the follow-up period, all 23 patients were alive. No adverse events of Grade 3 or higher were observed in all patients from the period of HSRT to the present.
Obliteration rate
Overall complete obliteration rate was 69.6% (16/23). We present a case for whom HSRT was performed on an AVM of grade IV (Spetzler-Martin grade) with a nidus volume of 12 ml and complete occlusion was confirmed on angiography (Figure 2).
Figure 2: A case for whom HSRT was performed on an AVM of grade IV (Spetzler-Martin grade) with a nidus volume of 12 ml and complete occlusion was confirmed on angiography. (A) – Pre-treatment angiography image (B) - Post-treatment angiography image (C) – Dose distribution. HSRT resulted in complete occlusion of AVM (indicated by circles in figure A and B). HSRT, hypofractionated stereotactic radiotherapy; AVM, arteriovenous malformation.
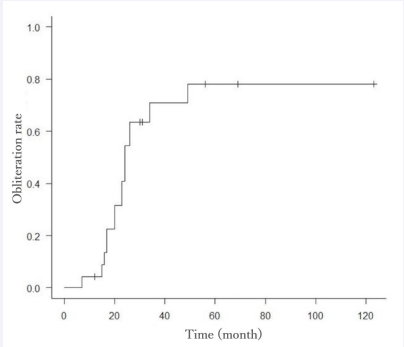
The obliteration rates at 36, 48, and 60 months after HSRT were 63%, 72%, and 78%, respectively (Figure 3).
Figure 3: Obliteration rate respect to nidus volume of 4 ml. No significant difference was seen between the obliteration rates respect to nidus volume with a threshold of 4 ml (p=0.275).
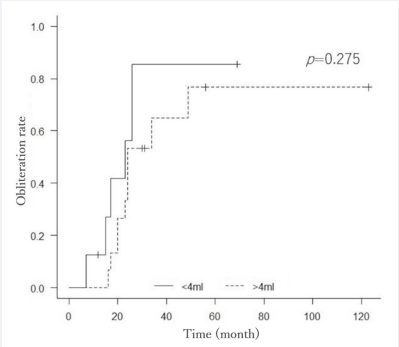
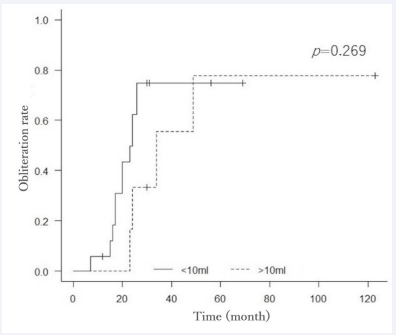
Rebleeding happened in four patients; two of the four underwent surgery, and the other two were followed-up conservatively. Surgery was performed in three of the six cases with partial obstruction, and SRS was added in the other three. When comparing the two groups with thresholds set at 4 ml and 10 ml, there was no significant difference in occlusion rates (p=0.27 and 0.26, respectively) (Figure 4,5).
Figure 4: Obliteration rate respect to nidus volume of 4 ml. No significant difference was seen between the obliteration rates respect to nidus volume with a threshold of 4 ml (p=0.275).
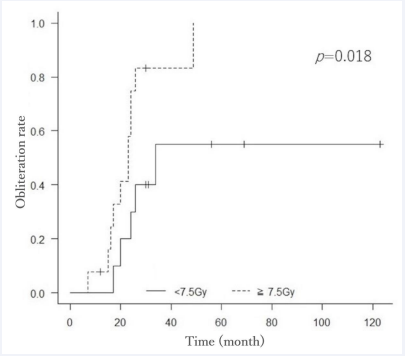
Figure 5: Obliteration rate respect to a prescription dose per fraction of 7.5 Gy. The case group with a prescription dose per fraction of >=7.5 Gy had a significantly higher nidus obliteration rate than that with a dose of <7.5 Gy (p=0.018).
The case group with a prescribed dose per fraction of >=7.5 Gy had a significantly higher nidus obliteration rate than that with a dose of <7.5 Gy (p=0.018) (Figure 6).
Figure 6: Obliteration rate respect to nidus volume of 10 ml. No significant difference was seen between the obliteration rates respect to nidus volume with a threshold of 10 ml (p=0.269).
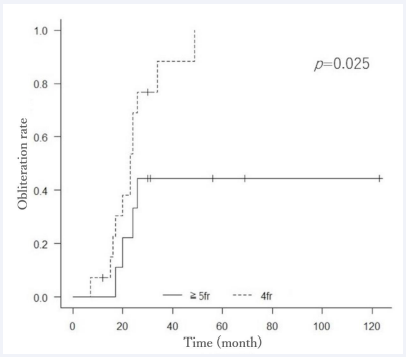
Regarding the number of fractions of HSRT, the 4-fraction case group had a significantly higher obliteration rate than the 5-fraction or more case group (p=0.025) (Figure 7).
Figure 7: Obliteration rate respect to the number of fractions. Regarding the number of fractions of hypofractionated stereotactic radiotherapy, the 4-fraction case group had a significantly higher obliteration rate than the 5-fraction or more case group (p=0.025).
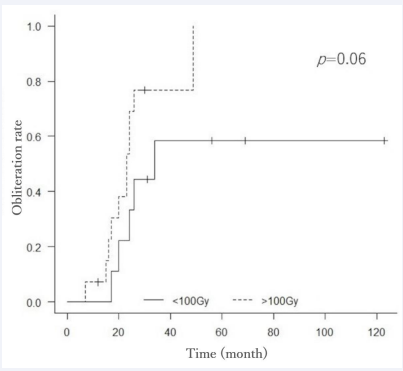
In comparison with BED (α/ β=3) based on the linear quadratic equations (LQ model), dose of >=100 Gy (EQD2) was associated with higher obliteration rate comparing with dose of <100 Gy, although the difference did not reach the significant level (p=0.060) (Figure 8).
Figure 8: Obliteration rate respect BED. In comparison with BED (α/β=3) based on the linear quadratic equations, dose of >=100 Gy (Equivalent Dose in 2 Gy fraction) was associated with higher obliteration rate comparing with dose of <100 Gy, although the difference did not reach the significant level (p=0.06).
DISCUSSION
SRS is expected the high obliteration rates for intracranial AVMs. Radiotherapy is commonly used in treatment for malignant tumor. Since AVM is benign tumor, the mechanism of therapeutic effect caused by radiation in AVM differs from that in malignant tumor. Nidus is obliterated by granulation of endothelial cells, inflammatory changes, fibrinoid degeneration, hyalinosis (vitrification), and other inflammatory changes in the vessel wall [11]. These changes are due to late reaction of radiation, whereas anti-malignant tumor effects are mainly caused by acute response. α/β ratio of late reaction is generally smaller than that of acute reaction. In fact, from the study using the LQ model, it can be inferred that the α/β ratio that would be expected for nidus occlusion in AVM would be small. Kocher et al., computed α/β ratios for obliteration of AVMs and revealed an α/β ratio value of 3.54 Gy, and they also calculated an α/β ratio value of 4.6 and
6.4 Gy for small (<3 cm) AVMs [18]. When an α/β ratio is small, the impact of high dose per fraction on the therapeutic effect becomes significant. SRS is a special radiotherapy technique that administers high dose at one time, and AVM is a good treatment adaptation of SRS. For intracranial AVMs with small nidus volume, SRS is expected to provide sufficient obliteration and one of the standard treatments. Shilienger et al., reported that the overall obliteration rate was 64% with a 48–96 months follow-up from analysis of 169 AVM cases [8]. In a review by Yamamoto et al., 65% of 40 patients achieved AVM obliteration with a follow- up period of 54 to 205 months [9]. Flickinger et al., revealed that the obliteration rate increased as the prescribed dose of SRS raised and reached a plateau above 20 Gy and they stated that irradiation beyond 25 Gy might not be significant [19]. In SRS for intracranial AVMs, it is estimated that a prescribed marginal dose of about 20 Gy might be optimal.
Since AVMs are benign lesions, it is important to treat them with few adverse events. Although SRS is a treatment with a steep dose gradient and this special characteristic reduces the irradiated dose to surrounding normal tissue, the impact on surrounding normal brain tissue could be problematic in cases of intracranial AVM with large nidus volume. Miyawaki et al., reported a 22% frequency of severe radiation induced brain necrosis when a dose of 16 Gy or more at the marginal dose was administered for patients with a nidus volume of 14 ml or more [20]. As for late adverse event of SRS, cyst formation has been reported [9,21].
For intracranial AVM with a large nidus volume or when the nidus is located in an eloquent area, we have to administer a lower prescribed dose in consideration of adverse events, leading to a lower obliteration rate. The use of combined endovascular embolization, repeated SRS, and HSRT have been reported in order to improve obliteration rate [11- 16,22]. Aoyama et al., evaluated the correlation between that obliteration rate and fraction number and revealed that there was no statistically significant difference in obliteration rate between the SRS and HSRT (p=0.44) [12]. In the present study, overall complete obliteration rate of HSRT was 69.6 %, which might be comparable to SRS. Analysis of nidus size showed no statistically significant differences in occlusion rates between groups of >4 ml and <4 ml or between groups of >10 ml and <10 ml. The appropriate prescribed dose and number of fractions of HSRT has not currently been established. Veznedaroglu et al., compared 42 Gy/6 fraction and 30 Gy/6 fraction groups for large AVM patients and reported a significantly higher obliteration rate in the 7 Gy per fraction group (83% versus 22%) [17]. Shah et al., performed HSRT designed to deliver a BED of approximately 150 Gy and achieved 100 % of obliteration rate in 37 patients, but radiation necrosis occurred in four [11]. Sparks et al., reported that obliteration rate was 15.2% in 33 patients treated by
HSRT of 30 Gy/5 fractions providing a BED of 90 Gy [15]. Chen et al., reviewed 38 patients with the median dose regimen of 35 Gy in five fractions (a BED of 116.67 Gy) and reported that obliteration rate was 74% [16]. From results of the present study, the prescription doses of 7.5 Gy or more per fraction in four fractions could be one of the optimal regimens to get sufficient obliteration rates without sever adverse events. A BED with an α/β ratio of 3 for 30 Gy/4 fractions is 105, and it might say a BED (α/β=3) >=100 Gy is needed to get high obliteration rates, which is consistent with previous reports.
There are some limitations to this study. First, the prescribed dose used in our institution cannot be simply compared with that in past reports. In this study, we set the central dose of the PTV to be 100% of the prescribed dose, but if the peripheral dose is set to be 100% of the prescribed dose, the central dose is expected to be higher than the prescribed dose. In addition, we acknowledge that this study is an analysis of a small number of cases. To begin with, the number of intracranial AVMs for which radiotherapy is considered is limited, because surgery is selected for cases in which surgery is possible. Radiotherapy is indicated for patients with Grade III or higher on the Spetzler-Martin, especially for patients whose nidus is located in an eloquent area or patients who are ineligible for surgery for any reason. We assume that it is difficult to draw strong conclusions based on reports from a single institution. It is expected that the accumulation of a small number of reports such as this study will lead to the optimal dose, and we believe that the results of our study provide a clue to the appropriate regimen of HSRT for AVMs.
CONCLUSION
We retrospectively reviewed the relationship between the prescribed dose and obliteration rate in patients with intracranial AVM patients treated with HSRT. HSRT performed at our institution showed an obliteration rate comparable to SRS without severe adverse events, although many of the patients had relatively large nidus. The prescription doses of 7.5 Gy or more per fraction in four fractions could be one of the optimal regimens to get sufficient obliteration rates. Also, it might say BED with an α/β ratio of 3 >=100 Gy is needed to get high obliteration rates. Improvement of treatment results with optimal dose regimen is expected with the accumulation of future cases.
REFERENCES
- Abecassis IJ, Xu DS, Batjer HH, Bendok BR. Natural history of brain arteriovenous malformations: a systematic review. Neurosurg Focus. 2014; 37: E7.
- Hillman J. Population-based analysis of arteriovenous malformation treatment. J Neurosurg. 2001; 95: 633-637.
- Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. 1986. J Neurosurg. 2008; 108: 186-193.
- Naranbhai N, Pérez R. Management of Brain Arteriovenous Malformations: A Review. Cureus. 2023; 15: e34053.
- Arteriovenous Malformation Study Group. Arteriovenous malformations of the brain in adults. N Engl J Med. 1999; 10: 1812- 1818.
- Lee CC, Chen CJ, Ball B, Schlesinger D, Xu Z, Yen CP, et al. Stereotactic radiosurgery for arteriovenous malformations after Onyx embolization. A case-control study. J Neurosurg. 2015; 123: 126-135.
- Ellis TL, Friedman WA, Bova FJ, Kubilis PS, Buatti JM. Analysis of treatment failure after radiosurgery for arteriovenous malformations. J Neurosurg. 1998; 89: 104-110.
- Schlienger M, Atlan D, Lefkopoulos D, Merienne L, Touboul E, Missir O, et al. Linac radiosurgery for cerebral arteriovenous malformations: results in 169 patients. Int J Radiat Oncol Biol Phys. 2000; 15: 1135-1142.
- Yamamoto M, Jimbo H, Hara M, Saito I, Mori K. Gamma knife radiosurgery for arteriovenous malformations: long-term follow-up results focusing on complications occurring more than 5 years after irradiation. J Neurosurg. 1996, 38: 906-914.
- Chen Y, Li R, Ma L, Zhao Y, Yu T, Wang H, et al. Single-Stage Combined Embolization and Resection for Spetzler-Martin Grade III/IV/V Arteriovenous Malformations: A Single-Center Experience and Literature Review. Front Neurol. 2020; 11: 570198.
- Shah SN, Shah SS, Kaki P, Satti SR, Shah SA. Efficacy of Dose-Escalated Hypofractionated Radiosurgery for Arteriovenous Malformations. Cureus. 2024, 16; e52514.
- Aoyama H, Shirato H, Nishioka T, Kagei K, Onimaru R, Suzuki K, et al. Treatment outcome of single or hypofractionated single- isocentric stereotactic irradiation (STI) using a linear accelerator for intracranial arteriovenous malformation. Radiother Oncol. 2001; 59: 323-328.
- Tripathi M, Kumar N, Sreenivasan SA, Ahuja CK, Jani P, Bhatta R, et al. Hypo fractionated Gamma Knife Radiosurgery for Intra cranial Pathologies: A Single Center Prospective Analysis of Feasibility, Safety, Efficacy, and Complication Profile. Neurol India. 2023; 71: S189-S197.
- Murray AL, Dally M, Jeffreys A, Hwang P, Anderson JFI. Neuropsychological outcomes of stereotactic radiotherapy for cerebral arteriovenous malformations. J Clin Neurosci. 2014; 21: 601-606.
- Sparks H, Hovsepian A, Wilson B, De Salles A, Selch M, Kaprealian T, et al. Dose Hypofractionated Stereotactic Radiotherapy for Intracranial Arteriovenous Malformations: A Case Series and Review of the Literature. World Neurosurg. 2019; 126: e1456-1467.
- Chen JCT, Mariscal L, Girvigian MR, Vanefsky MA, Glousman BN, Miller MJ, et al. Hypofractionated stereotactic radiosurgery for treatment of cerebral arteriovenous malformations: Outcome analysis with use of the modified arteriovenous malformation scoring system. J Clin Neurosci. 2016, 29: 155-161.
- Veznedaroglu E, Andrews DW, Benitez RP, Downes MB, Werner- Wasik M, Rosenstock J, et al. Fractionated stereotactic radiotherapy for the treatment of large arteriovenous malformations with or without previous partial embolization. Neurosurgery. 2004; 55: 519-530.
- Kocher M, Wilms M, Makoski HB, Hassler W, Maarouf M, Treuer H, et al. α/β Ratio for arteriovenous malformations estimated from obliteration rates after fractionated and single-dose irradiation. Radiother Oncol. 2004; 71: 109-114.
- Flickinger JC, Kondziolka D, Maitz AH, Lunsford LD. An analysis of the dose-response for arteriovenous malformation radiosurgery and other factors affecting obliteration. Radiother Oncol. 2002; 63: 347-354.
- Miyawaki L, Dowd C, Wara W, Goldsmith B, Albright N, Gutin P, et al. Five year results of LINAC radiosurgery for arteriovenous malformations: outcome for large AVMS. Int J Radiat Oncol Biol Phys. 1999; 44: 1089-1106.
- Kihlström L, Guo WY, Karlsson B, Lindquist C, Lindqvist M. Magnetic resonance imaging of obliterated arteriovenous malformations up to 23 years after radiosurgery. J Neurosurg. 1997; 86: 589-593.
- Blackburn SL, Ashley WW, Rich KM, Simpson JR, Drzymala RE, Ray WZ, et al. Combined endovascular embolization and stereotactic radiosurgery in the treatment of large arteriovenous malformations: Clinical article. J Neurosurg. 2011; 114: 1758-1767.