Rate and Causes of Nondiagnostic Ultrasound Examinations of Appendicitis: An Observational Cohort Retrospective Study
- 1. Radiology and Nuclear Medicine Department, Security Forces Hospital, Riyadh, Saudi Arabia
- 2. Department of Radiology and Medical Imaging, King Saud University Medical City, King Saud University, Riyadh, Saudi Arabia
- 3. Radiology and Nuclear Medicine Department, Security Forces Hospital, Riyadh, Saudi Arabia
- 4. Qassim Cluster, King Fahd Specialist Hospital, Buraidh, Saudi Arabia
- 5. Radiology and Nuclear Medicine Department, Security Forces Hospital, Riyadh, Saudi Arabia
- 6. Ministry of Health, Riyadh, Saudi Arabia
Abstract
Objectives: An early and precise diagnosis is important to confirm acute appendicitis (AA) in children. Ultrasound imaging techniques have demonstrated higher value in the diagnosis of AA. This study was conducted to ascertain the nondiagnostic and diagnostic rates of U/S examinations for appendicitis in children and possibly examine the causes of these high failure rates.
Material and Methods: All abdominal and appendiceal U/S examinations for patients ≤16 years old that were performed at King Saud University Medical City (KSUMC), Riyadh, Saudi Arabia, between April 2019 and December 2021 (approximately 32 months) were retrospectively examined and evaluated after the local ethics committee gave its approval for the study. Final ultrasound reports were categorized as “positive,” “negative,” “borderline,” or “not visualized.”
Results: During the 32 months, 112 results of patients (62, 55.4% males and 50, 44.6% females), who underwent ultrasound (U/S) of the appendix were performed, reviewed, and analyzed (mean age, 10.59 ± 2.9 years). The rate of U/S non-diagnostic results was recorded in 77 (68.8%) cases, whereas 35 studies (31.2%) were classified as diagnostic. Of all the 35 diagnostic U/S studies, seven had follow-up CT scans, which showed five (35.7%) positive and two (14.3%) negative results. On the other hand, of the 77 non-diagnostic ultrasound (U/S) scans, seven had follow-up CT scans, which showed 3 (21.4%) borderline and 4 (28.6%) non-visualized appendices. There was no significant difference in the rate of US non-diagnostic results according to gender or the procedure performed. U/S sensitivity was 47.1%, specificity was 87.5%, positive predictive value was 87.5%, and negative predictive value was 47.5%.
Conclusion: We found a high rate of nondiagnostic tests for appendicitis. A comprehensive reassessment of the patient is required, and a second US may be necessary to confirm the diagnosis. It is recommended that implementing a standard US report template based on validated secondary appendicitis signs, assessment of appendiceal size, and improved techniques from a graded compression US to CT or MRI would improve diagnostic accuracy.
Keywords
• Ultrasound
• Computed Tomography
• Appendicitis
• Pediatrics
• Nondiagnostic
CITATION
Alshaibani MM, Abujamea AH, Alghamdi SB, Alomaireeni SA, Alroumi ZM, et al. (2025) Rate and Causes of Nondiagnostic Ultrasound Ex aminations of Appendicitis: An Observational Cohort Retrospective Study. J Radiol Radiat Ther 13(1): 1109.
INTRODUCTION
A prompt and accurate diagnosis is crucial to confirm or rule out perforation in acute appendicitis (AA), a condition with a high prevalence. With a lifetime frequency of about 7%, it is the most common abdominal emergency. Since the presentation is often typical, clinical diagnosis remains challenging in both juvenile and adult populations. Often, non-specific symptoms coexist with those of other disorders [1].
Although the clinical diagnosis of this condition based on the patient’s medical history and physical examination (according to the Alvarado standard), some patients lack the AA-specific symptoms, and the outcomes of early diagnostic procedures like laboratory tests and white blood cell counting are ambiguous and on the verge of being inconclusive [2]. More specialized diagnostic techniques, such as laparoscopy, ultrasonography (U/S), barium enema, computed tomography (CT) scan, and magnetic resonance imaging (MRI), must be used in these individuals to differentiate appendicitis from other disorders with comparable clinical symptoms [3]. An increase in morbidity and death is linked to an appendicitis diagnosis that is made too late. Additionally, an inaccurate appendicitis diagnosis forces unneeded surgery, making the essential choice of whether to operate or not difficult [4]. There is widespread agreement that high rates of negative appendectomies (approximately 15 percent) must be accepted to lower the rate of perforation because AA with perforation is linked to severe morbidity and an increase in mortality [4,5].
A failed appendectomy could expose the patient to risks beyond those associated with the operation. Before the age of 20, tonsils and the appendix can be surgically removed, but there is an increased risk of suffering an acute myocardial infarction (AMI) as a result. Hence, one study found that before adulthood, when tonsillectomy and appendectomy were performed, that moderately more likely to cause a subsequent AMI, and Such operations have been linked to long-term health impacts. The authors note that more research is required, but small changes in immune function after these operations may change the cardiovascular risk and raise the risk for Hodgkin’s lymphoma [6].
Recent years have seen a significant increase in the importance of research focusing on various aspects of imaging techniques in the diagnosis of AA, including radiation protection. However, widespread accessibility and cost-effectiveness became increasingly important aspects of contemporary U/S imaging in the diagnosis of AA [7]. Radiologists and many other medical subspecialists already perform U/S imaging for suspected AA all over the world, with or without the assistance of sonographers [8].
More than 70% sensitivity and specificity have been observed in several studies on ultrasound that demonstrate its value in the diagnosis of appendicitis. Although U/S has a demonstrated function in the diagnosis of AA. Therefore, the operator’s expertise, skill, and understanding are crucial [9]. This study will concentrate on the challenges associated with diagnosing AA in patients seen in the U/S department, the prevalence of the condition, and strategies for increasing diagnostic precision. Determining the scope of the issue and the reasons behind non-diagnostic U/S exams in appendicitis cases may help us better understand the reasons behind delayed diagnosis, misdiagnosis, or high rates of unsuccessful appendectomies and reduce the likelihood that patients will need surgery. The current study was conducted to ascertain the nondiagnostic and diagnostic rates of U/S examinations for appendicitis in children and possibly examine the causes of these high failure rates.
MATERIALS AND METHODS
All abdominal and appendiceal U/S examinations for patients ≤16 years old that were performed at King Saud University Medical City (KSUMC), Riyadh, Saudi Arabia, between April 2019 and December 2021 (approximately 32 months), were retrospectively examined and evaluated after the local ethics committee gave its approval for the study. The study excluded all U/S studies performed outside of KSUMC, those performed on critically ill patients, patients with other pathologies identified that explain the patient’s symptoms, patients who underwent emergency surgeries without first undergoing a U/S, and U/S images with poor quality.
Data on the patients’ demographics, U/S results, and pathological analysis were all collected. Following that, final ultrasound reports were categorized as “positive,” “negative,” “borderline,” or “not visualized.” A report that identified appendicitis was deemed positive. A report that stated that the radiologist determined it to be either a normal appendix or that it was not appendicitis was considered negative. Borderline was a report that did not include the radiologist’s diagnosis but indicated any unusual or ambiguous findings that might be connected to appendicitis. When a report claimed that it was unable to locate the appendix, this was considered “not visualized”. Positive and negative reports were regarded as “diagnostic,” “borderline,” and “not visualized” as not diagnostic, respectively.
The data were analyzed using the Statistical Package for Social Sciences (SPSS software) version 25.0 (SPSS Inc., IBM, Armonk, New York, USA). Results are expressed as numbers and percentages for categorical variables and mean and standard deviation for continuous variables. The relationship between categorical variables (sonographic findings, operative data, pathological diagnosis) was done using the Chi-square test, and the Pearson correlation test (for continuous variables such as age). A p-value of ≤0.05 was considered statistically significant.
RESULTS
During the 32 months, 112 results of patients (62, 55.4% males and 50, 44.6% females) who underwent U/S of the appendix were performed, reviewed, and analyzed. The mean age of all patients was 10.59 ± 2.9 years (range: 4.0 to 16.0 years). Sixty-two (55.4%) of the U/S procedures were U/S of the abdomen, whereas 22 (19.6%) were U/S of the abdomen and pelvis, 4 (3.6%) were U/S of the lower abdomen for appendicitis, and 24 (21.4%) were unspecified other areas. The rate of U/S non-diagnostic results was recorded in 77 (68.8%) cases, whereas 35 studies (31.2%) were classified as diagnostic. Follow-up CT scans were obtained in 49 (43.7%) patients, including 41 (83.7%) diagnostic and 8 (16.3%) non-diagnostic CT scans. Table 1 demonstrates the detailed characteristics of the patients.
Table 1: Detailed characteristics of 112 patients who had U/S of the appendix
|
Characteristics |
Mean (SD) |
n (%) |
|
Age in years |
10.59 (2.9) |
|
|
Age, min-max |
4.0 – 16.0 |
|
|
Gender |
|
|
|
Male |
62 (55.4%) |
|
|
Female |
50 (44.6%) |
|
|
Procedure type |
|
|
|
U/S abdomen |
62 (55.4%) |
|
|
U/S abdomen and pelvis |
22 (19.6%) |
|
|
U/S lower abdomen for appendicitis |
4 (3.6%) |
|
|
U/S Unspecified area |
24 (21.4%) |
|
|
U/S results |
|
|
|
U/S positive |
26 (23.2%) |
|
|
U/S negative |
9 (8.0%) |
|
|
U/S borderline |
22 (19.7%) |
|
|
U/S not visualized |
55 (49.1%) |
|
|
U/S categories |
|
|
|
Diagnostic |
35 (31.2%) |
|
|
Non-diagnostic |
77 (68.8%) |
|
|
CT scan results (n=14) |
|
|
|
Diagnostic |
7 (50.0%) |
|
|
Non-diagnostic |
7 (50.0%) |
Table 2 shows the appendix U/S results by impression, with the percentage of follow-up abdominal CT imaging. Of all the 35 diagnostic U/S studies, seven had follow-up CT scans, which showed five (35.7%) positive and 2 (14.3%) negative results. On the other hand, of the 77 non-diagnostic U/S, seven had follow-up CT scans, which showed 3 (21.4%) borderline and 4 (28.6%) not visualized appendices. There was no significant difference in the rate of US non-diagnostic results according to gender (male=42, 54.5% vs. female=35, 45.5%, p=0.840).
Table 2: Appendix U/S results by impression with percentage of follow-up abdominal CT imaging.
|
U/S impression |
Total |
Follow-up CT scan |
||||
|
n |
% |
95%CI |
n |
% |
95%CI |
|
|
Diagnostic Positive Negative Total |
26 9 35 |
23.2% 8.0% 31.2% |
21-26 5-13 28-35 |
5 2 7 |
35.7% 14.3% 50.0% |
30-38 10-16 48-53 |
|
Nondiagnostic Borderline Not visualized Total |
22 55 77 |
19.7% 49.1% 68.8% |
16-22 46-53 63-73 |
3 4 7 |
21.4% 28.6% 50.0% |
18-25 24-32 48-53 |
There was also no significant difference in the US non-diagnostic results according to the procedure performed (p=0.258). The mean age of the patient was not significantly different between those who had a US non-diagnostic result versus those with a US diagnostic result (p=0.465) (Table 3). We report a calculated U/S sensitivity of 47.1%, specificity of 87.5%, positive predictive value of 87.5%, and negative predictive value of 47.5% compared to the CT scan.
Table 3: Comparing different variables based on diagnostic and non-diagnostic US results
|
|
Diagnostic U/S n=35 |
Nondiagnostic U/S N=77 |
OR for Nondiagnostic U/S (95% CI) |
p values |
|
Age in years, mean (SD) |
10.89 (2.7) |
10.46 (2.9) |
t=-0.733 (-1.59-0.74) |
0.465 |
|
Gender Male Female |
20 (57.1%) 15 (42.9%) |
42 (54.5%) 35 (45.5%) |
0.930 (0.533-1.622) |
0.840 |
|
Procedure 1 2 3 4 |
15 (42.9%) 8 (22.9%) 2 (5.7%) 10 (28.6%) |
47 (61.0%) 14 (18.2%) 2 (2.6%) 14 (18.2%) |
0.791 (0.606-1.033) |
0.258 |
DISCUSSION
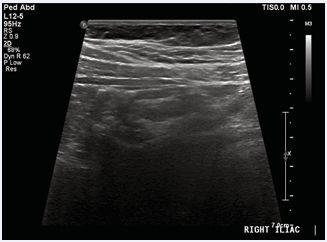
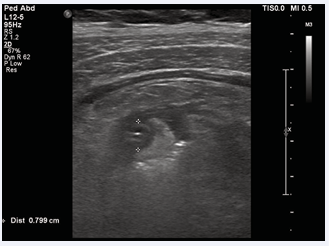
In the emergency room, pediatric patients with abdominal pain are a frequent occurrence, and imaging is frequently needed to establish whether surgical intervention is necessary. In our study, a significant percentage of appendix ultrasounds were not diagnostic (68.8%). Our results are almost identical to the Cohen et al study’s [10]. 63.34% nondiagnostic rate for diagnosis of AA in children. In their study, they noted that the risk of radiation exposure, in particular the elevated incidence of leukemia and brain tumors in children who have undergone CT scans, is still a major concern [10]. This is true even though a CT scan has a higher sensitivity than other imaging modalities like an ultrasound, despite the limitations of using an ultrasound to diagnose appendicitis. Although the absolute risk of tumors remains low, many have emphasized a careful approach to avoid unnecessary exposure [11,12]. The use of a CT scan has only been supported when a U/S is nondiagnostic. Another study done in a community setting revealed that a high percentage of pediatric appendix ultrasounds performed were nondiagnostic, and that follow-up CT imaging revealed that the likelihood of a CT scan was four times higher in the nondiagnostic group than the diagnostic group. Variability in radiologists’ interpretations is another potential cause of an increase in ambiguous readings. When compared to university radiologists who have had subspecialized training, community hospitals may have radiologists with less experience reading pediatric ultrasounds [13]. The adoption of standardized interpretative categories by the radiologist is one method of attempting to reduce interpretation variability. For instance, diagnostic accuracy is increased to 96.8% when considering the presence or absence of secondary symptoms when the appendix was not visible, compared to 94.1% for a binary interpretative scheme [14]. Some studies have developed protocols to restrict the use of CT scans. It has been discovered that protocols using CT solely after inconclusive appendix U/S had greater sensitivities and specificities than U/S alone, as well as a low rate of negative appendectomy [15]. One children’s hospital was able to minimize CT imaging by 41% while maintaining diagnostic accuracy by adhering to a clinical practice guideline [16]. Follow-up CT imaging is a logical next step in the diagnostic procedure in cases where U/S is nondiagnostic with persistent suspicion of appendicitis [15,16]. According to one study, individuals with incompletely visible appendices and the presence of sonographic secondary signals most often have appendicitis and do not require further imaging when using U/S alone [13]. In addition, whether or not the appendix is directly visible, MRI without secondary indications of appendicitis is successful in eliminating appendicitis, whereas otherwise negative right lower quadrant (RLQ) U/S that fail to identify the appendix are less beneficial. Regardless of the radiological modality, secondary signs of appendicitis without visibility of the appendix were not useful [17]. Here is an illustration of a non-diagnostic U/S of a 10-year-old child in which the appendix was not visible (Image 1) and a diagnostic U/S with signs of a significant wall thickening and an up to 0.8 cm-long inflamed appendix (Image 2).
Image 1: Nondiagnostic U/S in which the appendix was not visible
Image 2: Diagnostic U/S showing signs of a significant wall thickening and an up to 0.8 cm-long inflamed appendix
Without the need for additional imaging, patients with a negative or inconclusive U/S of the appendix and less than two predictors of pain migration to the RLQ, vomiting, male gender, and a white blood cell count higher than 12.0 x 10? /L can be discharged home with next-day follow-up [18,19]. Another study revealed that patients with a nondiagnostic U/S without leukocytosis do not need any additional diagnostic imaging. Unfortunately, because our investigation concentrated on the radiological and not the clinical aspects of appendicitis, we were unable to evaluate these associations with likely predictors. Numerous more observations on the more probable causes of a nondiagnostic U/S for appendicitis have been made, including young adults and children who are overweight [19]. According to another study, a second U/S scan or clinical reassessment may provide a higher level of diagnostic accuracy for pediatric appendicitis, particularly in obese children with a low likelihood of appendicitis who should not routinely undergo U/S scanning [20]. Regarding age, we found no statistically significant difference between the diagnostic and nondiagnostic U/S results in this investigation.
In this study, we report a sensitivity of 47.1%, specificity of 87.5%, positive predictive value of 87.5%, and negative predictive value of 47.5% compared to the CT scan. At a community hospital that regularly performs U/S for the evaluation of appendicitis, previous research of children and adults found a sensitivity of 83% and a specificity of 95% [21]. This study did not take into consideration the use of ultrasound to rule out appendicitis when it was not specifically noted in radiology reports, which could have reduced the number of negative/normal or nondiagnostic appendices. This could be the cause of the low negative predictive values and artificially high positive predictive values. Because of this, even though U/S has a high diagnostic positive predictive value, it demonstrates that it is better at identifying positive than negative findings, which is consistent with the findings of Johansson et al., [22]. Many academics have suggested employing a strategy in which CT is only used if the initial US evaluation is nondiagnostic [23]. Our analysis, unfortunately, shows that a large majority of appendix U/S values are nondiagnostic. This may be due to a variety of reasons, including the test’s operator dependence and adequate imaging. Apart from patient-related characteristics such as greater body mass index, normal appendix, retrocecal placement, distal tip inflammation, and perforation, several sonographers may not be recognized or may only be partially seen when doing pediatric ultrasounds [13].
Accordingly, suggestions to increase appendix visualization and decrease nondiagnostic findings in kids with suspected AA, sonographers performing appendiceal U/S undergo training in the scanning technique, and awareness of secondary signs significantly improved the visualization rate and provided more useful findings to referrers [24]. Another is the adoption of a standardized ultrasound report form based on approved secondary appendicitis symptoms, which may eliminate unnecessary tests, increase diagnostic precision, and reduce the need for CT scans [25]. To avoid differences between ultrasounds, a comprehensive reassessment of the patient is required, followed by supplementary imaging if indicated. This may necessitate a second US test [1]. As stated by one study, implementing a standard US report template based on validated secondary appendicitis signs and a stepwise imaging approach that begins with graded compression US and progresses to CT or MRI may nearly eliminate non-diagnostic examinations and improve diagnostic accuracy [25,26]. Another recommendation for improving the appendicitis diagnostic US was measuring the size of the appendix and the presence of secondary symptoms if the appendix was not visible [27]. Partain et al., proposed that a variety of appendiceal diameters might be utilized as a positive criterion for appendicitis. The sensitivity of the US dropped while the specificity rose with a 7mm typical assessment of an atypical appendicitis size [27]. In another study, using forced upward sweepings of the high-frequency linear transducer moving upward on the low-lying cecum and false or true pelvic location of the vermiform appendix will improve US diagnostic accuracy [28]. An upgraded grasshopper optimization algorithm-based support vector machine may distinguish uncomplicated from complicated appendicitis and increase accuracy, sensitivity, and specificity to more than 80% [29].
LIMITATIONS
We did have certain limitations because this was a retrospective study. First, the clinical or pathologic result of each patient’s medical course was not included in our study. Despite this study’s limitations, we concentrated on how initial U/S test findings affected future CT scan testing. Second, our ability to extend our assessment of the diagnostic sensitivity, specificity, and accuracy of appendiceal U/S may have been constrained by the small sample size.
CONCLUSION
At our facility, a very high rate of nondiagnostic tests appears to be limiting the usefulness of ultrasound to diagnose appendicitis. The significant negative predictive value indicates that not all patients who underwent follow-up CT imaging after receiving a diagnostic U/S agreed with the results of the original ultrasound. If an appendix ultrasound is nondiagnostic, a comprehensive reassessment of the patient is required, and a second US may be necessary to verify the diagnosis. Implementing a standard US report template based on validated secondary appendicitis signs, assessment of appendiceal size, improved techniques such as forced upward sweepings for low-lying cecum and vermiform appendix, an algorithm-based support vector machine, and a stepwise imaging approach from a graded compression US to CT or MRI improves diagnostic accuracy. However, it would be wise to establish a systematic approach, including other diagnostic tests, for the work-up of juvenile abdominal discomfort, until U/S displays improved and consistent test features.
REFERENCES
- Mostbeck G, Adam EJ, Nielsen MB, Claudon M, Clevert DA, Nicolau C, et al. How to diagnose acute appendicitis: ultrasound first. Insights Imaging. 2016; 7: 255-263.
- Javaherzadeh M, Sabet B, Malekpour-Alamdari N, Kazeminejad B, Noraee N, Mokhber-Dezfolly M. The predictive value of modified Alvarado score in diagnosis of acute appendicitis. J Isfahan Med Sch. 2016; 34: 745-750.
- Farrokh D, Feyzi A, Rastegar YF. Ultrasound in the differential diagnosis of acute appendicitis. J North Khorasan Univ Med Sci. 2016; 8: 321-330.
- Shogilev DJ, Duus N, Odom SR, Shapiro NI. Diagnosing appendicitis: evidence-based review of the diagnostic approach in 2014. West J Emerg Med. 2014; 15: 859-871.
- Humes DJ, Simpson J. Acute appendicitis. BMJ. 2006; 333: 530-534.
- Janszky I, Mukamal KJ, Dalman C, Hammar N, Ahnve S. Childhood appendectomy, tonsillectomy, and risk for premature acute myocardial infarction—a nationwide population-based cohort study. Eur Heart J. 2011; 32: 2290-2296.
- Brenner DJ, Hall EJ. Computed tomography-an increasing source of radiation exposure. N Engl J Med. 2007; 357: 2277-2284.
- Hosseini MM, Safdari R, Shahmoradi L, Javaherzadeh M. Better diagnosis of acute appendicitis by using artificial intelligence. ISMJ. 2017; 20: 339-348.
- Russo A, Cappabianca S, Iaselli F, Vallone G, Reginelli A, Grassi R. Acute abdominal pain in childhood and adolescence: assessing the impact of sonography on diagnosis and treatment. J Ultrasound. 2013; 16: 201-207.
- Cohen B, Bowling J, Midulla P, Shlasko E, Rosenberg H, Schechter S, et al. The non-diagnostic ultrasound in appendicitis: is a non-visualized appendix the same as a negative study? J Pediatr Surg. 2015; 50: 923- 927.
- Krishnamoorthi R, Ramarajan N, Wang NE, Huang D, Mueller CM, Chen C, et al. Effectiveness of a staged US and CT protocol for the diagnosis of pediatric appendicitis: reducing radiation exposure in the age of ALARA. Radiology. 2011; 259: 231-239.
- Pena BM, Mandl KD, Kraus SJ, Goodman DC, Perrin JM, Homer CJ. Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis in children. JAMA. 1999; 282: 1041- 1046.
- Alter SM, Walsh B, Lenehan PJ, Shih RD. Ultrasound for diagnosis of appendicitis in a community hospital emergency department has a high rate of nondiagnostic studies. J Emerg Med. 2017; 52: 833-838.
- Larson DB, Trout AT, Fierke SR, Towbin AJ. Improvement in diagnostic accuracy of ultrasound of the pediatric appendix through the use of equivocal interpretive categories. AJR Am J Roentgenol. 2015; 204: 849-856.
- Kaiser S, Frenckner B, Jorulf HK. Suspected appendicitis in children: US and CT—a prospective randomized study. Radiology. 2002; 223: 633-638.
- Russell WS, Schuh AM, Hill JG, Strout TD, O’Connor SC, Mannix MM, et al. Clinical practice guidelines for pediatric appendicitis evaluation can decrease computed tomography utilization while maintaining diagnostic accuracy. Pediatr Emerg Care. 2013; 29: 568-573.
- Kearl YL, Claudius I, Behar S, Macias CG, Monroe D, Dudley NC, et al. Accuracy of magnetic resonance imaging and ultrasound for appendicitis in diagnostic and nondiagnostic studies. Acad Emerg Med. 2016; 23: 179-185.
- Leeuwenburgh MM, Stockmann HB, Bouma WH, Houdijk AP, Verhagen MF, Vrouenraets B; OPTIMAP Study Group. A simple clinical decision rule to rule out appendicitis in patients with nondiagnostic ultrasound results. Acad Emerg Med. 2014; 21: 487-496.
- Keller C, Wang NE, Imler DL, Vasanawala SS, Bruzoni M, Quinn JV. Predictors of nondiagnostic ultrasound for appendicitis. J Emerg Med. 2017; 52: 318-323.
- Schuh S, Man C, Cheng A, Newton AS, Lam T, Stimec J, et al. Predictors of non-diagnostic ultrasound scanning in children with suspected appendicitis. J Pediatr. 2011; 158: 112-118.
- Chan I, Bicknell SG, Graham M. Utility and diagnostic accuracy of sonography in detecting appendicitis in a community hospital. AJR Am J Roentgenol. 2005; 184: 1809-1812.
- Johansson EP, Rydh A, Riklund ÅK. Ultrasound, computed tomography, and laboratory findings in the diagnosis of appendicitis. Acta Radiol. 2007; 48: 267-273.
- Teo EL, Tan KP, Lam SL, Ong CL, Wong CS. Ultrasonography and computed tomography in a clinical algorithm for the evaluation of suspected acute appendicitis in children. Singapore Med J. 2000; 41: 387-392.
- Reddan T, Corness J, Harden F, Mengersen K. Improving the value of ultrasound in children with suspected appendicitis: a prospective study integrating secondary sonographic signs. Ultrasonography. 2019; 38: 67-73.
- Nielsen JW, Boomer L, Kurtovic K, Ziembicki S, King S, Gross T, et al. Reducing computed tomography scans for appendicitis by introduction of a standardized and validated ultrasonography report template. J Pediatr Surg. 2015; 50: 144-148.
- Swenson DW, Ayyala RS, Sams C, Lee EY. Practical imaging strategies for acute appendicitis in children. AJR Am J Roentgenol. 2018; 211: 901-909.
- Partain KN, Patel AU, Travers C, Mitchell E, Travers CP. Improving ultrasound for appendicitis through standardized reporting of secondary signs. J Pediatr Surg. 2017; 52: 1273-1279.
- Lee JH, Jeong YK, Park KB, Park JK, Jeong AK, Hwang JC. Operator- dependent techniques for graded compression sonography to detect the appendix and diagnose acute appendicitis. AJR Am J Roentgenol. 2005; 184: 91-97.
- Xia J, Wang Z, Yang D, Shi H, Wang J, Li B. Performance optimization of support vector machine with oppositional grasshopper optimization for acute appendicitis diagnosis. Comput Biol Med. 2022;143:105206.