Spontaneous Hamman-Macklin Pneumomediastinum in pediatric age. Two Unusual Forms
- 1. City Hospital Radiology Service, Italy
Abstract
Pneumomediastinum (PNM) is a pathological condition characterized by the penetration of air into the mediastinal space. The most frequent cause of pneumomediastinum is trauma that can cause burst rupture of the esophagus, trachea or bronchi (closed trauma) or passage of air from outside or from the respiratory spaces (penetrating trauma).
Rarer, non-traumatic causes may be mediastinal abscesses caused by airborne germs or pathological or traumatic perforation of a hollow abdominal viscus with consequent ascent of air through the diaphragmatic orifices.
Keywords
Pneumomediastinum; Trauma; Mediastinal abscesses
Citation
VISCONTI A, DIMONTE M (2022) Spontaneous Hamman-Macklin Pneumomediastinum in pediatric age. Two Unusual Forms. J Radiol Radiat Ther 10(1): 1094.
INTRODUCTION
Pneumomediastinum (PNM) is a pathological condition characterized by the penetration of air into the mediastinal space [1]. The most frequent cause of pneumomediastinum is trauma that can cause burst rupture of the esophagus, trachea or bronchi (closed trauma) or passage of air from outside or from the respiratory spaces (penetrating trauma).
Rarer, non-traumatic causes may be mediastinal abscesses caused by airborne germs or pathological or traumatic perforation of a hollow abdominal viscus with consequent ascent of air through the diaphragmatic orifices.
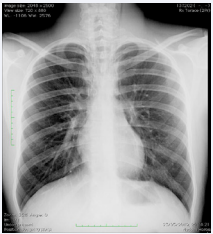
Figure 1: Case one. Standard chest X-ray AP view showing bilateral paramediastinal/paracardiac radioluncent bands.
Quite rarely we find cases of spontaneous pneumomediastinum (Hamman-Macklin syndrome), a condition characterized by the presence of free air in the mediastinum unrelated to trauma or invasive procedures, and which takes its name from the author who first described it in 1939 [2]. Commonly the term spontaneous indicates the absence of association with morbid events (predisposing causes can be recognized such as asthma, interstitial diseases, respiratory infections, tobacco, corticosteroids, the use of inhaled drugs or other irritating substances) and triggering causes such as episodes of coughing and all those conditions that reproduce the Valsalva manoeuvre
We report two unusual forms: one case about a 3-year-old boy and another one regarding a 15-year- old adolescent in whom spontaneous PNM is probably due respectively to a few coughs and during a concert sound check, both cases lacking of any predisposing pathology.
In particular we want to focus attention both on retrosternal pain in pediatric age, usually underestimated, as a relevant sign of spontaneous PNM and the role of CT scan in detecting the PNM allowing the differential diagnosis with other forms of PNM.
4. Description of cases
A 3-year-old boy and a 10-year-old adolescent came to our observation for retrosternal pain in the absence of dyspnoea. In both cases, there was no history of asthma or metabolic disease. The onset of symptoms in the first 3-year-old child was due to a coughing fit and in the second during singing tests at school.
The radiographic examination of the chest, performed in the two standard orthogonal projections, showed the presence of radiolucent bands in the paramediastinal and paracardiac areas bilaterally that extended between the cardiac base and the diaphragmatic dome (sign of the continuous diaphragm) (Figure 1).
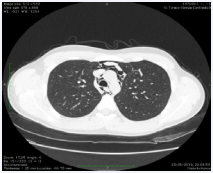
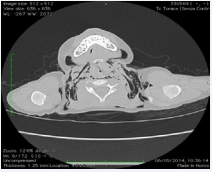
Spiral CT of the chest showed the presence of air in the context of the mediastinal connective tissue, between the vascular structures, around the heart and in the bronchial and esophageal sites. Furthermore, in the case of the 3-year-old boy, CT showed the presence of an area in the pulmonary interstitium arranged in a serpiginous manner, indicating the site of the alveolar lesion. The examination allowed to highlight in both patients the presence of subcutaneous emphysema with cervical and thoracic localization and allowed to exclude the presence of subpleural emphysema bubbles or associated mediastinal lung pathologies (Figure 2).
Figure 2: Case one. Chest CT showing air infiltrating mediastinal soft tissues.
The diagnosis of spontaneous pneumomediastinum was made in the absence of a positive history of a traumatic event or of diseases capable of determining a PNM.
The evolution of the picture was checked with standard radiograms and the two children were discharged 6 and 8 days after the first hospitalisation.
DISCUSSION
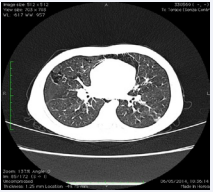
Spontaneous PNM is a rare condition in childhood with an incidence ranging from 1:7,000 to 1:42,000 cases with two peaks reported in the literature, one under 7 years of age and the other between 13 and 17 years of age. In a study by Yelin et al in which all children who came to the emergency room for dyspnoea and chest pain were screened, the reported incidence was 1:14,000 cases, therefore it is considered that sometimes it may occur in an unknown manner and therefore the its true incidence is underestimated [3] (Figure 3).
Figure 3: Case two. Chest CT: air infiltrating lung and parahilar interstice
The most accredited pathogenetic hypothesis is the one formulated by Hamman and confirmed by Macklin after studies carried out on animals, according to which in all cases of spontaneous PNM the primum movens would be represented by a rupture of the “marginal alveoli” placed in contact with the pulmonary vessels, of the interstitial tissue, small bronchi and bronchioles, and therefore subjected to greater pressure stress [4].
The rupture would be due to an alteration of the pressure gradient existing between the blood vessel and the alveolus, or to a sudden increase in intra-alveolar pressure (asthmatic crisis, Valsalva maneuver, vomiting, persistent cough, deep breathing, intense exercise, Heimlich maneuver, etc.) or for a sudden reduction in pulmonary arterial flow (pulmonary embolism, pulmonary stenosis, reduction of venous return to the heart).
Once the rupture of the alveolus has occurred, the air penetrates the interstitium causing interstitial emphysema and from the “escape route” it proceeds along the perivascular sheaths and the peribronchial fascial planes.
Due to the pressure gradient existing between the pulmonary periphery and the hilar region, the air reaches the hilum with a so-called “antegrade” path, dissects the mediastinal connective and is arranged around the heart, great vessels, trachea and oesophagus.
In some cases the increase in pressure can cause the rupture of the mediastinal pleura with consequent pneumothorax while in others the air can go up along the vascular sheaths of the neck (more frequent occurrence) causing the formation of subcutaneous emphysema of the supraclavicular, axillary, cervical regions and of the face with almost always symmetrical and bilateral distribution; or it may travel downward through the diaphragmatic orifices causing retropneumoperitoneum or penetrate the medullary canal resulting in pneumorachis.
The most feared complication is the development of a pneumopericardium which almost always requires urgent surgical treatment to avoid cardiac tamponade and be fatal.
Clinically, PNM manifests itself with more or less intense pain mostly localized in the retrosternal area or radiating to the back, dyspnoea of variable entity, more intense in the initial stages and tending to slowly attenuate, and subcutaneous crepitus, clearly noticeable in the cervical and supraclavicular.
In some cases main symptoms are dysphagia and odynophagia, asthenia, cough or alteration of voice tone (rhinolalia or nasal voice) due to penetration of air into the retropharyngeal space [5,6]. Pathognomonic is Hamman’s sign characterized on auscultation by “fine dry and superficial crepitations, synchronous with cardiac activity, audible in the inspiratory phase and during systole”, best perceived in the precordial region on the left parasternal, in ipsilateral lateral decubitus, detectable however according to the literature only in 18% of cases.
The diagnosis of pneumomediastinum is made with the chest radiogram in which it is highlighted in the anteroposterior projection in the form of a radiolucent streak that outlines the profile of the heart and mediastinal vessels and which in the most serious cases can include the soft tissues of the neck where presents as bubbles of subcutaneous emphysema. In the lateral view, a radiolucent triangle can be seen retrosternally.
Other important signs from a radiological point of view are the sign of the “double contour of the cardiac profile” evident in the anteroposterior projection as a radiopaque streak parallel to the left border of the heart separated from it by a radiolucent streak due to the interposition of air between the mediastinal pleura and pericardium or the “continuous diaphragm sign” in which in the anteroposterior projection a radiolucent streak is highlighted due to the interposition of air between the heart and the diaphragm.
The CT examination is always decisive for the diagnosis and for the evaluation of the extent of the PNM and for the identification of any complications.
It is also described in the literature and it is possible, as in our case, to identify the site of the alveolar rupture by highlighting the air located in the prevailing interstitium in correspondence with the lesion [7].
Furthermore, the CT examination is also important because it allows to exclude the concomitance of subpleural air bubbles or other predisposing pulmonary pathologies, the absence of which allows the diagnosis of spontaneous PNM to be made, the prognosis of which is completely favorable (Figure 4).
Figure 4: Case two. Chest CT: subcutaneous emphysema with paraclavicular and neck distribution.
Monitoring the evolution of the disease is necessary to rule out the onset of complications, even if rare, and can be performed with a simple double-projection chest radiogram.
In the rare cases in which they arise, the use of CT is fundamental and indispensable, which allows an accurate diagnosis of any pneumothorax, pneumorachis or pneumopericardium.
The therapeutic approach [8], in symptomatologically silent cases is based on rest, on the administration of painrelieving therapy with ventilators, on the administration of lowflow oxygen where necessary and on the elimination of those conditions that can reproduce the Valsalva manoeuvre, therefore with antitussives or possible anti-constipation therapy.
In the most serious cases we intervene according to the complications by limiting assisted mechanical ventilation only to cases of severe necessity as it could increase the PNM and evolve towards the PNX.
CONCLUSIONS
Spontaneous pneumomediastinum is a rare condition but it can also arise in the pediatric age, and it is therefore important not to underestimate the persistent retrosternal pain in healthy young patients.
Fundamental is the use of imaging diagnostics and in particular of CT test which allows detection, differential diagnosis with essential versus trauma-related forms, in order to orient therapeutical approach, and above all the identification of any complications.
REFERENCES
3. Stefania Formicola, Fabio Antonelli, Paolo Cavaliere, Luigi Masini, Enrico Melillo, Anna Naclerio, et al. Un caso di grave insufficienza respiratoria secondaria a pneumomediastino spontaneo. Pneumologia Pediatrica. Giugno. 2015.