CPAP Induced Manic Episode in a Patient with Bipolar Disorder: A Case Report of Central Sleep Apnea
- 1. Department of Physiology, Medical School, Atatürk University, Turkey.
- 2. Department of Psychiatry, Medical Park Y?ld?zl? Hospital, Turkey.
- 3. Department of Neurology, Medical School, Atatürk University, Turkey.
- 4. Department of Physiotherapy and Rehabilitation, Faculty of Health Sciences, I?d?r University, Turkey
- 5. Department of Biochemistry, Regional Training and Research Hospital, University of Health Sciences, Turkey
- 6. Department of Psychiatry, Private Alt?nkoza Hospital, Turkey.
- 7. Department of Endocrinology and Metabolism, Medical School, Zonguldak Bülent Ecevit University, Turkey
Abstract
Objective: In this case report we present our laboratory observations of one patient with bipolar disorder and central sleep apnea (CSA) who was treated with continuous positive airway pressure (CPAP) for their sleep apnea.
Background: Bipolar disorder is a psychiatric disorder characterized by episodes of mania, hypomania and major depression. This disorder affects approximately 0.8% of the adult population. Bipolar disorder frequently disrupts mood, energy, sleep, cognition, behavior and patients thus struggle to maintain employment and interpersonal relationships. Obstructive sleep apnea is a fully described and well-recognized entity. Central sleep apnea (CSA), however, has been poorly studied. The prevalence of obstructive sleep apnea (OSA) is expected to be high in bipolar disorder due to accompanying comorbid obesity. There is no evidence according to frequency of CSA in the patients with bipolar disorder. Coexistence of CSA and bipolar disorder has not been previously reported.
Results: The case of bipolar disorder, CPAP was started after a polysomnographic diagnosis of CSA and CPAP titration study indicating that most of the apneas/hypopneas were eliminated with a significant improvement in oxygen saturation. It was very remarkable that in this case initiation of CPAP resulted in manic symptoms and also symptoms of the REM behavior disorder.
Conclusions: Psychiatrists, especially laboratory physicians and other clinicians need to monitor patients with bipolar disorder closely for worsening of manic symptoms when they are started on CPAP for underlying mild OSA and especially severe CSA.
Keywords
• CSA
• CPAP therapy
• Manic symptoms
• Bipolar
• REM behavior disorders
Citation
Kayabekir M, Eren F, Ceylan M, Bayraktutan ÖF, Alt?nkaynak K, et al. (2021) CPAP Induced Manic Episode in a Patient with Bipolar Disorder: A Case Report of Central Sleep Apnea. J Sleep Med Disord 7(2): 1125.
ABBREVIATIONS
AHI: Apnea-Hypopnea Index, BD: Bipolar Disorder, CA: Central Apnea, CS: Cheyne Stokes breathing, CSA: Central Sleep Apnea, CSAS: Central Sleep Apnea Syndrome, CPAP: Continuous Positive Airway Pressure, OSA: Obstructive Sleep Apnea, PSG: Polysomnography, REM: Rapid Eye Movement, NREM: non-REM, SaO2: Arterial Oxyhemoglobin Saturation, W: Awake
INTRODUCTION
Bipolar disorder (BD) is a psychiatric disorder characterized by episodes of mania, hypomania and major depression. BD is still being understood, in which genetic and environmental factors play a role. It is thought to be associated with circadian dysregulation. Mood exacerbations may also be provoked by seasonal patterns and alterations in light intensity (1-2). This disorder affects approximately 0.8% of the adult population. BD frequently disrupts mood, energy, sleep, cognition, behavior and patients thus struggle to maintain employment and interpersonal relationships (3). First-line treatments for BD include lithium and valproic acid supplemented by use of atypical antipsychotics, all of which are associated with myriad multisystem side effects, especially weight gain, that predispose patients to obstructive sleep apnea (OSA) among other potential complications (4). Sleep apnea: it is the stopping of respiration for 10 seconds or longer during sleep. The patient’s partner or close ones describe it as an interruption of snoring, as patient holding his/her breath during sleep. There are two main types of apnea: In central sleep apnea (CSA) air flow stops together with the effort of respiration. In OSA, air flow stops because of a narrowing in the upper respiratory tract but the effort of respiration still continues (5). OSA is mainly accompanied by snoring and other complaints like night sweats, feeling of suffocation, nocturia, morning headaches, irritability, forgetfulness and depression and hypertension might follow. The patients are generally obese with short and thick necks; they also have narrow upper respiratory tracts. This body composition is not a rule though; people from all age groups including children might have obstructive apnea. CSA might be due to lesions of the brain stem and regions associated with the regulation of breathing. Furthermore, heart failure, metabolic and toxic encephalopathies might lead to central apnea (CA). CSA might happen both in sleep and during wakefulness (5-8). The clinical presentation of OSA may overlap substantially with that of major depression, including report of poor sleep quality, daytime fatigue, difficulty concentrating, cognitive deficits and somatic symptoms such as headaches. Since the depressive phase of BD is often chronic and difficult to treat, and undiagnosed underlying medical conditions may greatly contribute to its unfavorable outcome, it is reasonable to speculate that sleep-disordered breathing may play a role in this clinical picture (10-12). OSA is a fully described and well-recognized entity. CSA, however, has been poorly studied. The prevalence of OSA is expected to be high in BD due to accompanying comorbid obesity. There is no evidence according to frequency of CSA in the patients with BD. Coexistence of CSA and BD has not been previously reported.
Case (History)
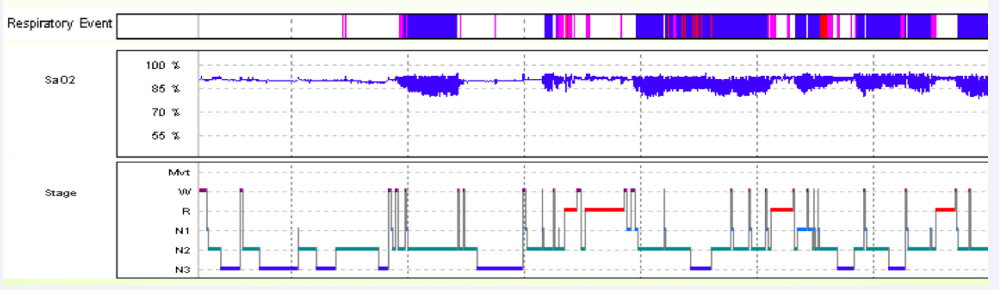
31 years old, Body Mass Index: 30.5 (obesity), male patient with BD was admitted to the sleep disorders center, electrophysiology laboratory with complaints of daytime sleepiness. Fragmented sleep was also detected in the patient who underwent a one-night sleep test (Polysomnography (PSG)). Respiratory findings in PSG (shown in the Figure): Apnea-Hipopnea Index (AHI): 75.5; supine AHI: 150; total number of the CA: 377/ one night; number of CA in the supine position: 280/ one night were particularly striking. 8 cmH2O automatic Continuous Positive Airway Pressure (CPAP); with a diagnosis of Central Sleep Apnea Syndrome (CSAS) therapy was started. Daytime sleepiness disappeared within 1 week, but on the 8th day, her husband told her that she strangled her mother in her sleep, the patient began to wake up very early (in the morning: 3), her mood and energy increased during the day, and her concentration deteriorated. Only the quetiapine dose of the patient who used 1200mg/day lithium (therapeutic index) was increased. The patient voluntarily discontinued CPAP. (Figure 1)
Figure 1: It shows the sleep histogram taken from the PSG recording of the patient with BD. Stage, Stages of sleep (N1: NREM1, N2: NREM2, N3 NREM3, R: REM, W: Awake); SaO2, Arterial Oxyhemoglobin Saturation (%)
Respiratory Event (pink lines indicate CA occurring during the night). Note the relationship between Stage and Respiratory Event for the cause of fragmented sleep: Sleep deprivations are seen due to CA. Also note the relationship between Respiratory Event and SaO2: Blood oxygen levels of case with BD cause serious decreases (blue areas) between CA events (pink lines) (NREM: Non Rapid Eye Movement, REM: Rapid Eye Movement).
DISCUSSION
CSA is prevalent in patients with heart failure, healthy individuals at high altitudes, and chronic opiate users and in the initiation of “mixed” (that is, central plus obstructive apneas). CA is their predominance in NREM sleep and especially in lighter sleep stages as well as their relative scarcity in phasic REM sleep (13-15). Physiologically, control of breathing during sleep is critical. It is important to understand the basic respiratory mechanisms in the pathophysiology of CA. In particular, metabolic control (chemoreceptors in the medulla sensitive to CO2), as well as intrapulmonary receptors directed by vagal nerves, regulate respiration via the brain stem (of course with the help of O2 and CO2 sensitive carotid body receptors). If the CO2 level is low at sleep onset, respiration cannot be stimulated (sleep onset CA). The chemosensitivity of patients with central alveolar hypoventilation and obesity hypoventilation syndrome decreases during the day; CA is rare, these patients experience hypoventilation especially during REM (hypercapnic respiratory failure). Increased CO2 chemosensitivity (idiopathic CA) too little CO2 increase during sleep causes disruption of respiratory rhythm. Periodic central apneas (Cheyne Stokes breathing (CS)) are seen in heart failures with low left ventricular ejection fraction and atrial fibrillation. The frequency of CS and CSA in the REM period is low. CSA occasionally emerge with CPAP titration of sleep-disordered breathing (complex sleep apnea), also can occur in patients on opiates (16-19). Our case was on regular BD treatment and had no substance abuse (opiate). CAs revealed in PSG disappeared during CPAP titration. Could CAS have a relationship with BD and the drugs it uses? Quetiapine mechanism of action might involve rapid dissociation from D2 receptors. Atypical antipsychotics treat manic symptoms associated with BD by blocking dopamine D2 receptors; Side effect is weight gain. Patients with a high baseline body weight are more likely to gain weight while taking lithium. Our case was obese; hypoventilation, heart failure was not detected. Maybe the CAs that emerged were related to high altitude (Our city, Erzurum, is 1900m above sea level). Or idiopathic CA may have been seen together with BD. So far, no case of coexistence of CSAS and BD has been reported. Our case, in which we could not see CA in REM processes in PSG, got up at night and strangled her mother. Does CPAP therapy also cause REM behavior disorder in BD patients?
As a result, CPAP application in a patient with BD, regardless of etiology, caused a new manic episode to occur.
CONCLUSION
Psychiatrists, clinicians, especially laboratory physicians who record electrophysiological signals; It should be kept in mind that CPAP therapy, which is initiated in patients with BD, will worsen manic symptoms, shorten sleep duration, and cause REM behavior disorder while treating sleep apnea.