Sleep Hygiene, Sleep Quality and Excessive Daytime Sleepiness among Indian College Students
- 1. Akal School of Public Health and Hospital Administration, Eternal University, India
- 2. Post Graduate Institute of Medical Sciences and Research, India
Abstract
Poor sleep hygiene is linked with sleep problems such as poor sleep quality and excessive daytime sleepiness (EDTS). Objective of this research was to assess the sleep hygiene practices of the Indian college students and study the relationship of sleep hygiene with sleep quality and EDTS.
A cross sectional study was conducted among 1215 college students using Sleep Hygiene Index (SHI), Pittsburg Sleep Quality Index (PSQI) and Epworth Sleepiness Scale (ESS). Mean SHI score of study population was 31.27 ± 6.09 and majority of the study population (77.7%) had poor sleep hygiene (SHI>26). Problem of poor sleep hygiene was found to be significantly more in professional courses (χ2 test p=0.000). Subjects with poor sleep hygiene had two times higher odds of poor sleep quality (OR 2.194, 95% CI: .595-3.017, p = 0.000) and more than two and half times higher odds of EDTS (OR 2.843, 95% CI: 2.016-4.009, p = 0.000). Results indicate the probable relationship of poor sleep hygiene with EDTS and poor sleep quality.
Keywords
• Sleep hygiene
• Sleep quality
• Excessive daytime sleepiness
• College students
• India
Citation
Kaur G, Singh A (2017) Sleep Hygiene, Sleep Quality and Excessive Daytime Sleepiness among Indian College Students. J Sleep Med Disord 4(1): 1076.
ABBREVIATIONS
EDTS: Excessive Daytime Sleepiness; ESS: Epworth Sleepiness Scale; SHI: Sleep Hygiene Index; PSQI: Pittsburg Sleep Quality Index; BA: Bachelor of Arts; BCom: Bachelor of Commerce; BSc: Bachelor of Science; BTech: Bachelor of Technology; BDS: Bachelor of Dental Surgery; MBBS: Bachelor of Medicine and Surgery
INTRODUCTION
Sleep plays very important role in health of an individual. Evidences have shown the linkage of poor sleep with cardiovascular disease [1], stroke [2], diabetes [3], metabolic dysfunctions [4]. The sleep hygiene is one of the determinant of sleep. Sleep hygiene encompasses simple behavioral practices, environmental factors that intend to promote healthy sleep. Mild to moderate insomnia is treated with the help of good sleep hygiene practices [5]. Poor sleep hygiene is associated with problems such as bad sleep quality [6], [7] and excessive daytime sleepiness (EDTS) [8]. Activities such as maintaining a regular sleep schedule [9], managing stress [10], avoidance of caffeine [11], regular physical exercise [12] and noise free bedroom [13] are good for sleep [14]. All these behavioral practices help in regulating circadian clock and maintaining natural sleep pattern [5,15].
As homeostatic drive and body internal clock or circadian rhythm influences the process of sleep therefore, melatonin suppression due to over illuminated nights [16] and overriding stress hormones [17] has thrown circadian clock of body out of gear. The natural sleep pattern is changing due to demands of service based economy and modern lifestyle [18]. Artificially lit cities buzz with commercial, industrial and other activities throughout the night to achieve and produce more. 24X7 entertainment industry, internet, mobile phones, smart phones and many other IT technologies have artificially extended the daytime. It has changed the sleep behavior of humans [19,20].
Rapid lifestyle and behavioral changes leading to poor sleep hygiene in college students have been noticed [21]. The college students are early adopters of technology and spend significant amount of time on internet, IT technologies, social media and late night partying. College students also sacrifice sleep for studies, completing assignments and other academic activities. Thus variance in sleep schedule is common in college students. Irregular bed time is associated with poor sleep quality and decreased sleep time. Even single night change in sleep schedule can induce difficulties in sleep initiation and maintenance [9]. College students are more prone to risk taking behaviors such as experimenting with addictions, smoking and consumption of liquor. Alcohol and nicotine interacts with sleep physiology and causes sleep problems such as EDTS, insomnia and snoring [22,23]. College students are often ignorant about good sleep hygiene practices and their implications [6]. However, there is dearth of literature on sleep hygiene and its impact on sleep health [5]. The sleep hygiene of Indian college students is not studied so far. Very few studies have been carried out that asses the implications of sleep hygiene on sleep health [8] showed that the poor sleep hygiene is associated with EDTS in junior resident doctor in India. Study tried to explore the effects of sleep hygiene on sleep health. The sleep hygiene practices of Indian college students were assessed through this study. No other study is available on the implications of sleep hygiene on the sleep health of Indian students.
Objective of the research was to study the sleep hygiene practices of the college students and to find the relationship of sleep hygiene with sleep quality and EDTS.
MATERIAL AND METHODOLOGY
It was a cross sectional study conducted among 1215 college students pursuing graduation in Bachelor of Arts (B.A.), Bachelor of Commerce (BCom), Bachelor of Science (BSc), Bachelor of Technology (BTech), Bachelor of Dental Surgery (BDS), and Bachelor of Medicine and Surgery (MBBS). These students belonged to various colleges in Chandigarh a north Indian city. Different behavioral practices associated with sleep were assessed with Sleep Hygiene Index (SHI), a self-administered questionnaire. To study the sleep health, Epworth sleepiness scale (ESS) and Pittsburg sleep quality index (PSQI) were used. ESS is used to assess EDTS and PSQI asses sleep quality. Ethical clearance was taken from ethical committee of Panjab University, Chandigarh, India. Data were collected during the time when students were free from their classes after taking permission from college authorities. To invite participants, the pamphlets were distributed in the colleges. Posters inviting students to participate were displayed on notice boards at prominent places such as canteens and common rooms of colleges. The announcements to invite participants into the study were made in classrooms. Before participation informed consent was obtained from all participants for this cross-sectional interview based non-interventional study. 30 students refused to participate in the study. Those who were ill at any time during the last month (n=15) were excluded from study as illness disturbs the natural sleep pattern.
Study tools
Sleep Hygiene Index Scale (SHI) - It is a 13-item self administered Likert scale index in which responses to each item are based on the frequency with which the person engges in the behaviour from 1(never) to 5 (always). The global assessment score of SHI range from 13–65. Scores more than 26 were taken as unhygienic sleep and 26 or less than that were considered as hygienic sleep. The test-retest reliability is good (r=0.71) and internal consistency Cronbach’s α is moderate (.66) for SHI [24].
Pittsburg Sleep Quality Index (PSQI) - It is a self-administered questionnaire used to asses sleep quality in last 1 month. It give a combined PSQI score that ranges from 0 to 21, and a higher score is indicative of poorer sleep quality. Scores less than or equal to 5 were associated with good sleep quality and score more than 5 were considered as poor sleep quality. It has high internal consistency Cronbach’s α = .83 and high test retest reliability of .85 (p<.001).It produces single factor on factor analysis [25]. Two factor solution [26,27] and three factor [28,29] produces better fit to data in other studies. Epworth Sleep Scale (ESS) -The ESS is an 8-item self-administered questionnaire producing scores that range from 0 to 24 with score exceeding 10 indicating abnormal levels of sleepiness. ESS has high internal consistency of Cronbach’s α =.88 and produces single factor on factor analysis [30]. Sociodemographic information pertaining to age, sex, education stream, and year of course was also collected.
Statistical Analysis; Normality of data was checked by Shapiro-Wilk test. Percentage, mean, SD, χ2 test, t-test, test of homogeneity of odds ratio and conditional independence and regression analysis were used for statistical analysis. SPSS statistical package 16.00 was used for statistical analysis.
RESULTS AND DISCUSSION
Sociodemographic profile of study participants is given in Table 1.
Table 1: Sociodemographic profile of study participants.
| Variable | Categories | Frequency | % | |
| Gender | Male | 625 | 51.40% | |
| Female | 590 | 48.60% | ||
| Study course | Arts + commerce | BA | 185 | 15.20 |
| BCom | 159 | 13.10 | ||
| Science | BSc ( Nonmedical + Medical) | 576 | 47.40 | |
| Professional courses | BTech | 148 | 12.20 | |
| BDS | 77 | 6.30 | ||
| MBBS | 70 | 5.80 | ||
| Bachelor of Arts (B.A.), Bachelor of Commerce (BCom), Bachelor of Science (BSc), Bachelor of Technology (BTech), Bachelor of Dental Surgery (BDS), and Bachelor of Medicine and Surgery (MBBS) | ||||
Male participants were 51.40% and rest was female. 28.30% students belonged to arts and commerce streams (BA and BCom), 47.70% belonged to science stream (BSc medical and non-medical) and 20.30% belonged to professional courses (BTech, BDS and MBBS).
Sleep Hygiene of study population
Majority of the study population (77.70%) had poor sleep hygiene (Table 2).
Table 2: Sleep Hygiene index among study participants (N=1215).
| Categories | Frequency (%) |
| Hygienic ≤26 | 271(22.30) |
| Unhygienic >26 | 944(77.70) |
Sociodemographic variables and sleep hygiene
Prevalence of poor sleep hygiene was highest in professional courses, significant difference was observed in prevalence of poor sleep hygiene of different streams (χ2 test p=.000).
Sleep hygiene practices of study participants
The item wise score is high for item 2 (I go to bed at different times from day to day), 8 (I use my bed for things other than sleeping), 12 (I do important work before bedtime) and 13 (I think, plan, or worry when I am in bed).
Sleep hygiene and excessive daytime sleepiness
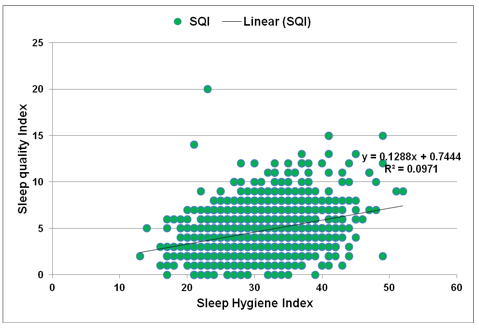
Simple linear regression was calculated to predict ESS score based on SHI score. Regression equation was found to be F (1, 1213) = 144.530, P<.01, With R2 of .106. Participants ESS score is equal to .1953X +2.8645 (Figure 1).
Figure 1: Linear regression curve of SHI scores with ESS scores
Table 5: Association of Sleep Hygiene with EDTS.
| SHI scale | OR | p | 95% CI for OR(p for OR) | |||
| Hygienic | Unhygienic | |||||
| EDTS | No EDTS | 225(27.37) | 597(72.63) | 2.843 | 0.000*** | 2.016-4.009(.000) |
| EDTS | 46 (11.70) | 347(88.30) | ||||
| Excessive Daytime Sleepiness (EDTS) & Sleep Hygiene Index (SHI) | ||||||
Table 5 shows the odds ratio for association between sleep hygiene and EDTS. The Mantel-Haenszel common odds ratio was estimated to be 2.843, with Breslow-Day and Tarone tests of homogeneity of odds ratio and Mantel-Haenszel test for conditional independence being highly significant (p<.001). The role of chance factor for odds ratio was ruled out with p<.001. The 95% confidence interval ranged from the observed lower bound limit (2.016) and upper bound limit (4.009).
Table 6: Comparison of Mean EDTS Scores of participants in Hygienic and Unhygienic groups.
| SHI | EDTS score | ||||
| N | mean | SD | t | p(2-tailed) | |
| Hygienic | 271 | 7.29 | 3.69 | -8.906 | 0.000*** |
| Unhygienic | 944 | 9.46 | 3.49 | ||
| Excessive Daytime Sleepiness (EDTS) | |||||
Table 6 shows comparisons of mean EDTS scores in hygienic and unhygienic groups. The mean EDTS score for 271 respondents with hygienic was 7.29 with SD of 3.69 and that for 944 respondents with unhygienic were 9.46 with SD 3.49.The difference in means was highly significant at p<.001. Further Cohen’s effect size (d=2.27) suggest high practical significance.
Sleep quality and sleep hygiene
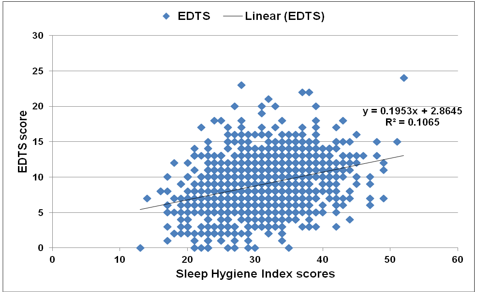
Simple linear regression was calculated to predict PSQI score based on SHI score. Regression equation was found to be F (1, 1213) = 133.09, P<.01, with R2 of .0971. Participants ESS score is equal to .1288X +.7444 (Figure 2).
Figure 2: Linear regression curve of PSQI scores with SHI scores
Table 7: Association between Sleep Quality and Sleep Hygiene.
| SHI | OR | p | 95% CI for OR(p for OR) | |||
| Hygienic | Unhygienic | |||||
| PSQI scale | Good | 213(26.49) | 591(73.51) | 2.194 | 0.000*** | 1.595-3.017(.000***) |
| Poor | 58(14.11) | 353(85.89) | ||||
| Sleep Hygiene Index (SHI) & Pittsburg Sleep Quality Index PSQI | ||||||
Table 7 shows that the odds ratio for association between sleep hygiene and sleep quality. The Mantel-Haenszel common odds ratio was estimated to be 2.194, with Breslow-Day and Tarone tests of homogeneity of odds ratio and Mantel-Haenszel test for conditional independence being highly significant (p<.00 1). The role of chance for odds ratio was ruled out with p<.001. The 95% confidence interval ranged from lower bound limit (1.595) and upper limit bound (3.017).
Table 8: Comparison of Mean PSQI Scores of participants in Hygienic and Unhygienic groups.
| SHI | PSQI score | ||||
| N | mean | SD | t | p(2-tailed) | |
| Hygienic | 271 | 3.77 | 2.33 | -7.605 | 0.000*** |
| Unhygienic | 944 | 5.06 | 2.50 | ||
| Sleep Hygiene Index (SHI) & Pittsburg Sleep Quality Index PSQI | |||||
Table 8 shows comparisons of mean PSQI scores in hygienic and unhygienic groups. The mean PSQI score for 271 respondents with hygienic was 3.77 with SD of 2.33 and that for 944 respondents with unhygienic were 5.06 with SD 2.50.The difference in means was highly significant at p<.001. Further Cohen’s effect size (d=1.66) suggest high practical significance.
DISCUSSION
Poor sleep hygiene is associated with sleep problems such as poor sleep quality. 77% of the college students under study had poor sleep hygiene. It may be due to ignorance or inability to practice the good sleep hygiene.
High variance in sleep schedules was noticed in studied participants. As per study, they were extensively doing cognitive/ stress inducing activities before sleep and used bed for activities other than sleeping. Using bed to study [31], worrying/ thinking about important matters at bed time were also frequent in American students [32]. In Chinese mainland students taking a nap during daytime [33] and stress near bedtime were common behaviors in Australian university students. [34]. Thus poor sleep hygiene practices observed Indian college students is almost similar to American and Australian students. Stress, anxiety and worrying before sleep significantly affect sleep health [35]. Various sleep problems such as poor sleep quality and EDTS are associated with academic and emotional stress among college students [36-38]. Research has indicated that variable sleep schedule is linked with poor sleep quality [9]. Regularization of sleep wake schedule is also linked with reduced daytime sleepiness [39]. Therefore, it has been established that regulating the timing to go to bed and wake up are good sleep hygiene practice. Poor sleep hygiene was also more common in professional and science stream students (Table 3).
Table 3: Summary of comparison between Hygienic and Unhygienic categories.
| Socio demographic variable | Category | Hygienic | Unhygienic | χ2 test p | OR | 95% CI OR |
| Sex | Male | 134(21.47) | 490(78.53) | 0.475 | 0.906 | 0.692- 1.187 |
| Female | 137(23.18) | 454(76.82) | ||||
| Year | First | 92(21.85) | 329(78.15) | χ2 test p=0.038* | ||
| Second | 73(18.72) | 317(81.28) | ||||
| Third | 106(26.24) | 298(73.76) | ||||
| Stream | Arts/Commerce | 87(25.29) | 257(74.71) | χ2 test p=0.000*** | ||
| Science | 145(25.17) | 431(74.83) | ||||
| Professional | 39(13.22) | 256(86.78) | ||||
Table 4: Item wise responses to Sleepiness Hygiene Index by study participants (N=1215).
| Ratings by Study Participants | Item Wise Score | |||||
| 1 Never |
2 Rarely |
3 Sometimes |
4 Frequently |
5 Always |
Mean ± SD ( 95%CI ) |
|
| 1. I take daytime naps lasting two or more hours. |
368 (30.3) | 383(31.5) | 314(25.8) | 103 (8.5) | 47 (3.9) | 2.24± 1.09 (2.18- 2.30) |
| 2. I go to bed at different times from day to day. | 146(12.0) | 243(20.0) | 351(28.9) | 305(25.1) | 170(14.0) | 3.09±1.22 (3.02-3.16) |
| 3. I get out of bed at different times from day to day. | 147(12.1) | 316(26.0) | 378(31.1) | 254(20.9) | 120(9.9) | 2.90±1.16 (2.84-2.97) |
| 4. I exercise to the point of sweating within one hour of going to bed. | 855(70.4) | 196(16.1) | 98(8.1) | 30(3.2) | 27(2.2) | 1.51±.93 (1.46-1.56) |
| 5. I stay in bed longer than I should two or three times a week. | 291(24.0) | 343(28.2) | 366(30.1) | 143(11.8) | 72(5.9) | 2.47±1.15 (2.41-2.54) |
| 6. I use alcohol, tobacco, or caffeine within four hours of going to bed or after going to bed. | 824(67.8) | 145(11.9) | 148(12.2) | 64(5.3) | 34(2.8) | 1.63±1.06 (1.57-1.69) |
| 7. I do something that may wake me up before bedtime (for example: play video games, use the internet, or clean). | 458(37.7) | 241(19.8) | 344(28.3) | 125(10.3) | 47(3.9) | 2.23±1.17 (2.16-2.29) |
| 8. I go to bed feeling stressed, angry, upset, or nervous. | 345(28.4) | 314(25.8) | 391(32.2) | 121(10.0) | 44(3.6) | 2.35±1.10 (2.28-2.41) |
| 9. I use my bed for things other than sleeping (for example: watch television, read, eat, or study). | 124(10.2) | 129(10.6) | 274(22.6) | 458(37.7) | 230(18.9) | 3.45±1.21 (3.38-3.51) |
| 10. I sleep on an uncomfortable bed (for example: poor mattress or pillow, too much or not enough blankets). | 779(64.1) | 236(19.4) | 135(11.1) | 42(3.5) | 23(1.9) | 1.60±.95 (1.54-1.65) |
| 11. I sleep in an uncomfortable bedroom (for example: too bright, too stuffy, too hot, too cold, or too noisy). | 748(61.6) | 254(20.9) | 150(12.3) | 43(3.5) | 20(1.6) | 1.63±.94 (1.57-1.68) |
| 12. I do important work before bedtime (for example: pay bills, schedule, or study). | 166(13.7) | 166(13.7) | 355(29.2) | 358(29.5) | 170(14.0) | 3.16±1.23 (3.10-3.23) |
| 13. I think, plan, or worry when I am in bed. | 99(8.1) | 132(10.9) | 364(30.0) | 343(28.2) | 277(22.8) | 3.47±1.19 (3.40-3.53) |
| Total Mean ± SD( 95%CI ) | 31.27± 6.09 (30.93-31.61 ) | |||||
Long lectures, practical classes, hectic schedule contribute to high academic stress in professional courses and that may leads to poor sleep hygiene. This finding need further need exploration and research.
High ESS score is associated with high SHI scores in study participants as depicted in regression line (Figure 1). Above result were also depicted when significant association is observed between unhygienic/ maladaptive sleep and EDTS (χ2 test p=.000) (Table 5). It mean that participants in maladaptive sleep hygiene category had two and half time higher odds of EDTS. Mean EDTS scores were also significantly higher in participants having maladaptive sleep. Sleep hygiene is a predictors of EDTS has relationship with EDTS. Similar relationship was observed between EDTS and sleep hygiene of Indian medical residents. A positive correlation was found between sleepiness and sleep hygiene. Physicians with more maladaptive sleep behaviors as indicated by SHI had three times chance of experiencing EDTS [8]. Linear regression showed a positive association between PSQI and SHI scores in study participants (Figure 2). Similar relationship was also observed as we see significant association between sleep hygiene and sleep quality (χ2 test p =.000) (Table 6). It mean that participants in maladaptive sleep hygiene category had two time higher odds of poor sleep quality. Similarly mean PSQI scores were also significantly higher in participants having maladaptive sleep hygiene. Poor sleep hygiene was significantly associated both with poor sleep quality and EDTS. Studies shows that poor sleep hygiene is associated with sleep problems such as EDTS [8,40] and poor sleep quality in students [41, 33,42,]. It means that good sleep hygiene promote sleep quality and protects from EDTS. Keeping in view the detrimental effects poor sleep health, it needs attention in public health. The sleep health problem has far reaching effects on health, academic, cognitive and future career performance of college students. Thus it is important to prevent sleep problems and promote healthy sleep practices in college students. College students are young and the poor sleep hygiene will have detrimental effect on their health for long time in future. Thus, there is a need to educate the students about sleep hygiene practices through educational sessions and workshops conducted by experts. College students should be screened for sleep problems and maladaptive sleep hygiene practices. Those requiring advice should be referred to a sleep clinics for expert advice.
In creating sleep health promoting environment the support of collages is also required. The optimization of academic pressure especially in professional courses also needs the active support of college authorities via different supports measures.
LIMITATIONS OF THE STUDY
Tool used in the study self-administered questionnaire, so respondent’s bias can’t be ruled out. Participants were recruited by open invitation and so study is not immune to selection bias.
CONCLUSIONS
Sleep hygiene is a significant factor that affects the sleep health of college students. Poor sleep hygiene may be associated with poor sleep quality and excessive daytime sleepiness.
ACKNOWLEDGEMENT
Sincere thanks to all the college students who participated in this study, without their cooperation this work would not have been possible.
REFERENCES
17. Lack LC, Wright HR. Chronobiology of sleep in humans. Cell Mol Life Sci. 2007; 64: 1205-1215.
18. Shochat T. Impact of lifestyle and technology developments on sleep. Nat Sci Sleep. 2012; 4: 19-31.
22. Roehrs T, Roth T. Sleep, Sleepiness, and Alcohol Use. Alcohol Research & Health.1998; 25:101-109.
30. Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep.1992; 15: 376-381.