Epididymal Abscess Mimicking Testicular Torsion in a 30 Gestational Week Premature Infant
- 1. Division of Urology, West Virginia University, USA
- 2. Kathryn Moffett, Department of Pediatrics, West Virginia University, USA
ABSTRACT
Epididymal abscess, epididymo-orchitis, infected hydroceles, and testicular torsion are all rare in a neonate. The practice of exploring an acute scrotum in this patient population remains controversial. Here we describe a case of an unusual presentation of an epididymal abscess that mimics testicular torsion, in hopes of presenting the appropriate evaluation of torsion, and affirming the decision to surgically explore the acute scrotum of a neonate if suspicion remains present following appropriate work up.
KEYWORDS
• Neonate
• Epididymis
• Testicle
• Abscess
CITATION
Hubsher CP, Prudnick C, Point D, Morley C, Moffett K, et al. (2014) Epididymal Abscess Mimicking Testicular Torsion in a 30 Gestational Week Premature Infant. J Surg Transplant Sci 2(1): 1006.
INTRODUCTION
Epididymitis and testicular torsion are two vastly different causes of testicular pain and swelling with strikingly similar symptomatology and presentation [1]. These conditions can be incredibly difficult to distinguish clinically from one another, especially in the nonverbal neonate. This distinction must be made as quickly as possible to save the testicle in case of torsion, and avoid unnecessary surgical exploration of the scrotum at this age in case of epididymitis. Due to the low testicular salvage rates of <5%, the decision to surgically explore an acute scrotum in a neonate remains controversial [2-4]. Thus, we describe a case of a neonate presenting with an epididymal abscess mimicking testicular torsion to elucidate the importance of surgical intervention in suspected neonatal torsion. To our knowledge, this is the youngest, and smallest, neonate ever reported in the literature with such a diagnosis [5].
CASE PRESENTATION
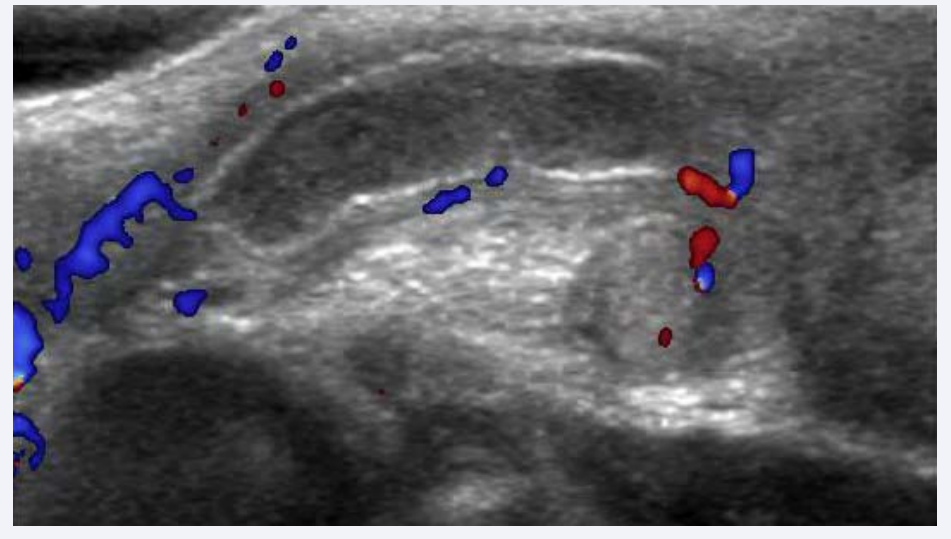
A 29 day-old male, weighing 0.97 kg (2 lb 2.2 oz), who was born premature at approximately 24 weeks to a healthy mother, was found to have a right testicular mass on exam. A scrotal ultrasound revealed normal caliber testes bilaterally with an increased vascularity on the right concerning for epididymitis. An increase in size of the right hemiscrotum prompted a follow up ultrasound approximately 2 weeks later. Findings demonstrated what appeared to be a hydrocele with hydrocord, a hypoechoic structure without any blood flow, and difficulty identifying the right testicle (Figure 1).
Figure 1: Ultrasound of right scrotum showing a hypoechoic structure without any central blood flow, a hydrocele with hydrocord, and significant inflammation.
These findings aroused a great concern for right testicular torsion. The patient was taken emergently to the operating room for scrotal exploration.
Upon incision into the scrotum, the presence of significant inflammatory tissue was noted. Exploration of the hemiscrotum did not demonstrate any signs of testicular cord torsion, however purulent material, which subsequently grew out Escherichia coli, was expressed from the right epididymis. Findings were consistent with a right epididymal abscess. Further examination of the right testicle revealed a viable testicle with appropriate blood flow. The patient was subsequently treated on antibiotics and follow up ultrasound 4 months after surgery demonstrated resolution of concerned right scrotal contents.
DISCUSSION
Here we present an unusual case of an epididymal abscess mimicking testicular torsion in a 30 gestational week premature infant. To our knowledge, this is the youngest, and smallest, patient ever reported with this diagnosis [5]. As the patient did not undergo any urethral manipulation or catheter insertion, we believe the abscess originated from a blood-borne etiology. In the neonatal period, epididymitis is a relatively rare condition but can be treated medically. For this reason, it is important to be able to distinguish this entity from testicular torsion to prevent an unnecessary surgical intervention at this critical age [6]. While physical exams may be similar in these two cases, the absence of the cremasteric reflex and the presence of a hardened testicle have emerged as two of the most sensitive findings for torsion [1,3,7]. Nonetheless, the presence of these findings are not unique to torsion, and should raise the clinician’s level of suspicion significantly.
Imaging is the recommended next step in management of a neonate with suspected acute scrotum. Testicular scintography, Color Doppler ultrasonography and high resolution ultrasonography are three methods commonly employed in the evaluation of testicular torsion [1,8]. High-resolution color Doppler ultrasonography is typically the method of choice for assessment of an acute scrotum in the neonate. It should be noted that the validity is highly dependent upon the skill of the ultrasound operator. Typical ultrasonographic findings can include a decrease in blood flow to the torsed testis compared to the contralateral testis via Doppler and/or visualization of the spermatic cord for evidence of twisting with high resolution ultrasound [8]. Imaging for epididymitis will typically show an increase in flow to the epididymis suggestive of inflammation [1].
The treatment of testicular torsion in the neonate is a controversial topic [1-4]. Numerous authors advocate continued immediate attempts at surgical salvage while many refute the practice citing the salvage rates in this population range from 0%-5% [2-4]. In our case, the decision to explore the testicle allowed for drainage of the epididymal abscess and resolution of the neonate’s scrotal issues.
We conclude that neonates found to have acute scrotal pain or swelling need to be evaluated as if they have a potential torsion requiring emergent surgery. Testicular torsion and epididymitis are two of the most common nontraumatic causes of an acute scrotum and early recognition, diagnosis and intervention is crucial to avoid tissue infarction [1]. Physical exam findings should be combined with imaging such as high-resolution ultrasonography or Doppler ultrasonography in order to make the most accurate diagnosis. Clinicians should keep in mind that ultrasonography alone cannot exclude testicular torsion, even in the sonographic presence of adequate testicular blood flow [1,2]. As evidenced by this case, if imaging and clinical exam are inconclusive in ruling out torsion, surgical intervention may be warranted. The decision to intervene surgically allowed for drainage of this epididymal abscess and salvage of this patient’s right testicle.