Laparoscopy and Bilateral Inguinal Hernias
- 1. Department of Surgery, University of La Salle, USA
- 2. Department of Health Sciences, University Anáhuac North Mexico, USA
- 3. Department of Surgery, Hospital Angeles Lomas, USA
ABSTRACT
It is difficult to know the exact incidence of bilateral hernias in adults but, since the advent of laparoscopy, there have been several reports that show a significant increase. Currently we know that bilateral repair can be done simultaneously without increasing the recurrence rate, especially when mesh is used. Laparoscopic hernioplasty has shown to be effective in the early detection of contralateral defects, providing a less invasive approach without additional morbidity, with the advantages of less pain and early recovery. On the other hand, traditional open surgery requires two separate incisions either if the procedures are performed simultaneously or sequentially. It is important for surgeons to keep in mind that although the common presentation is a unilateral hernia, the frequency of bilateral hernias is high and that it is advisable to comment with the patients beforehand, that there could be a possibility to explore and repair both hernia sides if found necessary.
KEYWORDS
• Bilateral hernia
• Laparoscopy
• TAPP
• TEP
CITATION
Weber-Sánchez A, Weber-Alvarez P, Garteiz-Martínez D (2016) Laparoscopy and Bilateral Inguinal Hernias. J Surg Transplant Sci 4(1): 1019.
ABBREVIATIONS
TAPP: Transabdominal Preperitoneal; TEP: Totally Extra Peritoneal
INTRODUCTION
Bilateral hernia has been an underestimated subject in herniology and today it continues to generate controversy. Since antiquity there have been reports that patients may have multiple hernias. Hippocrates described that people who ate beans of the genus Lathyrus developed tissue laxity and multiple hernias [1].
One of the first reports about bilateral hernia was done by Cheatle, who performed the repair through a midline incision without entering the abdominal cavity, pushing aside the peritoneum to expose both inguinal regions. Later, he described doing a Pfannenstiel incision, in order to inspect both sides even in patients with unilateral hernia diagnosed and to repair both sides when detecting a contralateral defect. Few surgeons reproduced this technique, probably because they considered it aggressive compared to current approaches at that time.
The group of Rives in Reims and Stoppa in Amiens were conscious of the importance of strengthening the posterior wall of the inguinal region, as they felt that its weakness to resist the pressure was a major cause in the development of hernias. Therefore, in the sixties they began to use a wide dacron prosthesis between the transversalis fascia and the peritoneum, using both anterior inguinal and preperitoneals approaches. The mesh was placed so that it exceeded the internal inguinal orifice in all directions to distribute the pressure and prevent recurrence. In their paper they made special mention about patients with multiple hernia defects and the convenience to asses all possible hernia sites through their approach. It is to be noted their interest about the possibility of contralateral hernia. Even with an anterior inguinal approach they stated: “another patch can be placed without hesitation on the opposite side if there is pain or weakness in the inguinal structures”.
Years ago, some authors argued that repair of bilateral hernias should be sequential. Perhaps one of the motives of controversy was the Palumbo and Sharp´s paper in 1971. They reported that recurrence with the open approach were significantly greater in the group of patients operated bilaterally at the same time. However analyzing closely this report, of 3572 patients, only 37 recurrences were reported, two in the group of 78 with simultaneous bilateral hernia repair (2.5%) and four among 756 (0.5%) the group operated sequentially, finding that was apparently confirmed by others [2].
Because recurrence was attributed to tension in the suture line, and Palumbo´s report, many surgeons preferred to defer the repair of the second hernia for a later time [3]. The time between the two procedures could vary from days to months, depending on factors such as weight, age, size of the second hernia, and others [4]. However other reports, especially using Lichtenstein tension-free technique, showed no difference in recurrence or complications if bilateral hernia repair was done simultaneously, compared with two separate surgeries [2,3,5] suggesting to perform the repair at the same time because of the benefits of doing it in a single anesthetic time, avoiding the risk of strangulation or incarceration in the time spent between the two procedures, reducing the stress of the patient with another operation and avoiding the cost of another surgical procedure [3,5,6]. Under the concept of tension-free hernia repair, open or laparoscopic, there has been a revolution in hernia repair with the widespread use of prostheses and currently, repair of bilateral hernias in the same surgery is generally accepted. In the early nineties, inguinal hernia repair by laparoscopic surgery became possible and, since its very beginning, the bilateral aspect of the hernia was mentioned as one of the main advantages of laparoscopy due to the possibility to diagnose and treat contralateral defects at the same time [7]. Many reports suggest laparoscopic repair is ideal for patients with recurrent or bilateral hernias and those requiring some other simultaneous laparoscopic procedure to avoid the incision in the groin and on the other hand, to shorten the recovery time and diminish postoperative pain[1].
EPIDEMIOLOGICAL CONSIDERATIONS
Hernioplasty is one of the most frequently elective surgeries performed, but it is difficult to know its precise incidence due to problems with data collection, misdetection and lack of accurate diagnosis. Most patients consult because the hernia is symptomatic or very noticeable, but many of them are not detected by the patient and they consult because of discomfort or groin pain [8]. The true frequency in which bilateral hernias are detected is even less known as shown by the clinical fact that operated patients return years later to be repaired on the contralateral side for hernia which was inexistent, underestimated or undetected at the time of the primary surgery. This is one of the explanations for the difference between series of bilateral hernias. This issue has been thoroughly reviewed in pediatric surgery for more than half a century, and although the pathophysiology seems to be different, it might be similar to what happens in adults. The percentage of bilaterality in newborns is around 15%, and may increase up to 40% in premature babies. The incidence of children who have undergone contralateral inguinal hernia repair in a second surgery may be up to 34% [9,10]. In his meta-analysis Miltenburg reported that the risk of developing a metachronous hernia in children under 18 years is 7%. Therefore, pediatric surgeons often perform contralateral inguinal exploration, especially in cases of left groin hernia, since the chances of finding hernia on the opposite side can be up to 40 to 60%. More recently, pediatric surgeons have relied on laparoscopic exploration through the processus vaginalis for contralateral exploration regardless presentation side of the primary hernia, as it helps to confirm or exclude the presence of a defect more accurately than with examination under anesthesia. They therefore recommend its routine practice and perform the repair if anomalies on the other side are observed [11].
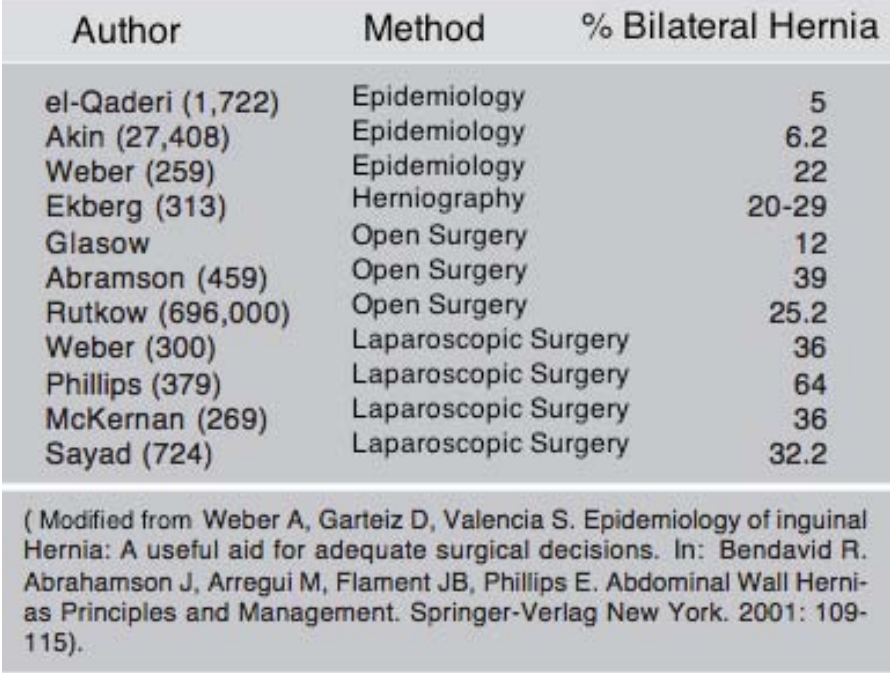
Reports of bilateral hernias in adults mainly among men are highly variable. Akin reported only 5% and el-Quaderi 6.2% of bilaterality among healthy population [12]. In the Hospital General de Mexico from 259 clinical files of open inguinal repair revised, 57 of them (22%) had bilateral hernia (because hey had undergone a contralateral hernia repair previously, because they had been already detected as such, or because bilateral hernia was detected during the hospital admission). Herniography detects between 20 and 30% of bilateral hernias, and open surgical series report bilateral hernias with frequency varying between 12 and 25% [3,13]. As shown in (Table 1), with laparoscopy bilateral hernia is reported much more frequently than with open surgery and can be up to 60%.
Table 1: Bilateral Hernia Reports.
DISCUSSION
With laparoscopy the difference in the percentages of bilateral hernias in the literature may be due to the fact that a posterior view and the effect of pneumoperitoneum facilitates detection of contralateral defects. Large defects with well-defined hernia sacs present no problem and can be perfectly appreciated. The difference may be related with small defects, the assessment of weakness of the inguinal floor and failure in the obliteration of processus vaginalis. The relatively high incidence of an occult contralateral patent processus vaginalis has led to the practice among pediatric surgeons to perform laparoscopic contralateral exploration [24].
In direct hernias, pneumoperitoneum allows to appreciate a weakness of the wall much better than with the open approach. Nyhus in 1991 mentioned that palpation was necessary during surgery to detect small hernias, but laparoscopy can diagnose small and undetected defects at earlier stages. It is also true that some surgeons do not consider these defects as true hernias, it is possible that they may never be clinically detected or symptomatic, but what is certain is that there is a defect on the posterior view of the inguinal wall, whose clinical course is unpredictable and potentially can develop into large and symptomatic defect like any other hernia that started that way. Even at the contralateral “healthy” side, hernias can develop later in a small percentage of cases as it was demonstrated by Saggar.
History of complex hernias may provide a warning about the possibility to develop another defect [14]. Felix [15] proposed the term complex hernias which was later extended and modified by our group to include patients who have one or more of the following facts: family history of hernia, known recurrent or bilateral hernia in the patient or his family, or patient with multiple hernia defects. In all these cases, special attention must be paid to explore both sides and all possible sites of herniation to treat them and prevent recurrences.
Harrison nearly a century ago and later Read and others, showed that inguinal hernia is a much more complex pathology than the simple defect explained by the saccular theory and that other factors such as collagen alterations and hereditary factors may be involved [16].
Another possibility to consider is herniation of preperitoneal fat that sometimes is not detected clinically, and is also difficult to detect by laparoscopy, as they aren’t seen as the typical hole but cause symptoms and need to be repaired. When they are suspected or diagnosed by physical exam or ultrasound, dissection of the groin can often reduce large masses of herniated preperitoneal fat and once reduced, the defect must be repaired. These true hernias are not the typical lipoma of the cord and should be detected by a good physical examination, by ultrasound or laparoscopy.
In reviewing the practice in our group with laparoscopic hernioplasty, of 143 patients we repaired 245 defects, 99 bilaterally (69%). Of these, 73 were detected as bilateral by physical examination, and in 25 the decision to repair bilaterally was due to the mentioned factors. There are countries like Scotland which in compliance with British Hernia Society Guidelines (2013), which recommend that bilateral inguinal hernias should be repaired laparoscopically, form a cost-utility patient perspective, perform elective primary bilateral hernia repairs by laparoscopy in 97 % of the cases [14-17,25].
Some patients with a negative contralateral exploration subsequently develop a symptomatic hernia on that side. A cohort study of metachronous contralateral hernia by Zendejas and others, revealed that from 409 patients with unilateral repair and negative contralateral exploration without previous hernia repair (n = 11) with a median follow-up of 5.9 years, 33 (8.1%), developed hernia on the previously “healthy” side, yielding incidence rates at 1, 5 and 10 years of 1.6, 5.9 and 11.8%, respectively. The median time to hernia development was 3.7 years (range 0.1-12.4) [18].
Taking into consideration all these factors, our group performs bilateral repairs often, as our actual view is that inguinal hernias should be operated when diagnosed in order to prevent complications [19]. We also do what we consider “prophylactic” repair in the high risk patients who have been thoroughly informed about the risks and benefits of the bilateral procedure [20,21].
Transabdominal preperitoneal (TAPP) or totally extra peritoneal (TEP) approach may be different in the detection of bilateral defects. Experience with both techniques is an important factor, because as has been mentioned, in TEP it is difficult to notice if there is an indirect component until lateral dissection has been completed. Some groups that prefer TEP to repair hernias use TAPP for the diagnosis of bilateral hernias. Initially they make an intra-abdominal approach to examine the abdomen and then perform the extraperitoneal approach [22,23].
Our group always performs TAPP repair, since one of its most obvious advantages is the ability to explore both inguinal regions. During the early years of our experience with laparoscopy more than twenty years ago, we used to place one large piece of mesh as described by Stoppa, but later we decided to do the repair placing mesh on each side which overlaps in the midline, because it is simpler to handle two, instead of one large piece of mesh.
For many years, bilateral inguinal hernia in adults was not considered as important as in children. Parents almost always accept the advice to explore both sides on their children, but most likely they would not accept bilateral open exploration for themselves if not clinically evident. But as the emphasis is on detection by physical exam and during the surgical procedure, contralateral hernia is more likely to be found by laparoscopy and it offers also as an attractive possibility to solve them in the same surgery. In Western countries, repaired bilateral inguinal hernias represent 10-15% of all repaired hernias, although this percentage is higher because with laparoscopy, small asymptomatic contralateral hernias that were undetected preoperatively are found during surgery between 22 to 50% of the times [21].
Postoperative complications such as surgical site infection with laparoscopy to explore contralateral processus vaginalis have been shown to be minimal [24]. As a matter of fact, some authors recommend performing routinely transinguinal laparoscopic exploration for identification of contralateral inguinal hernias and patent processus vaginalis because of the high prevalence of contralateral hernia for its safety and effectiveness [26].
Currently, some surgeons refuse to treat bilateral defects, especially when detected by the surgeon and not by the patient, or when patient is young, perhaps due to the fear of treating a disease that causes no symptoms, with the possibility of having a complication, adding cost and other considerations. Laparoscopic hernioplasty is a technique which can present specific complications, related to the access to the abdominal cavity, pneumoperitoneum, trocar site hernia, vascular, neural and visceral injuries which must not be neglected, but they can be avoided with adequate knowledge, proper technique and strategies directed to prevent them [27,28].
Inguinodinia is always a concern because the possibility to cause significant chronic pain independent of the method of repair either open or laparoscopic, affecting physical activity, social interactions and productivity, occurring in as much as 6 to 8% of patients. Common sources of pain include hernia recurrence, nociceptive problems (tissue inflammation, foreign material, meshoma), and neuropathic causes. Therefore, specific efforts to prevent injuries at the time of the repair through identification and careful handling of the nerves are the best measures to prevent this problem [29]. After Shin´s report in 2005 about patients with obstructive azoospermia after hernia repair with implantation of polypropylene meshes, some concern was raised about male patients undergoing bilateral mesh repair for inguinal hernias. However, literature reveals that most studies on obstructive azoospermia are based on animal experiments and incidental case reports [2]. Also it has been reported that bilateral repair does not affect the femoral vessel flow. At present simultaneous correction is recommended [4] as it does not increase morbidity or hospital stay. It does not modify the need for analgesia or recurrence rates, but reduces cost. Laparoscopic bilateral repair does not significantly increase operative time; Duluc reported his experience of more than 3,000 TEP repairs, with a mean operative time of 17 minutes for unilateral hernia and 24 for bilateral.
We think that once a surgeon takes into consideration the high frequency of contralateral defects he should discuss it with the patient in an effort to diagnose and repair a problem that is already present, although it may be asymptomatic, as with other pathological surgical conditions, because it can be done with minimal risk to the patient in the same operative time. Timing is also important to consider, as patient future medical conditions may not be optimal to expose him to other surgical or anesthetic risk.
The authors are aware that most surgeons do not perform laparoscopic inguinal hernia repair regularly and that this may be an important factor. Nonetheless, as minimally invasive techniques are taught more often and young surgeons become familiar with these procedures, the future will probably change this controversial issue. Trevisonno´s recent survey shows that most of the surgeons (59%) who do not see a benefit with laparoscopic approach also admit lack of training with this procedure. On the other hand, McCoy´s paper titled “Are open abdominal procedures a thing of the past?” shows an undisputable increase of 265% in laparoscopic inguinal and femoral hernia repairs with a concomitant decrease in open inguinal procedures performed by US general surgery residents [30].
CONCLUSION
One of the main advantages of laparoscopic approach is to treat through the same mini-incisions bilateral hernias simultaneously as was described since its beginning, with minimal risk, low recurrence rate, less pain, earlier recovery, without significantly increasing operative time, reducing costs; so why not treat them? Surgeons should discuss with their patients these facts and offer them the best option on individualized basis.
REFERENCES
1. Bernal GR. Manejo actual de la hernia inguinal por vía laparoscópica. Cir Gen. 2006; 28: 110-112.
7. Wantz GE. Complications of inguinal hernial repair. Surg Clin North Am. 1984; 64: 287-298.
8. Postlethwait RW. Recurrent inguinal hernia. Ann Surg. 1985; 202: 777-779.