Mediastinal evaluation of Silicosis according to Lung Transplantation
- 1. Thoracic Surgery Department, Adnan Menderes University, Turkey
SUMMARY
Silicosis is one of the oldest occupational diseases and causes the death of thousands of people worldwide every year. It is irreversible and progresses even after the exposure is over. Moreover, the lung transplantation may be the only change of the patients for treatment. But, is the intrathoracic ekstra pericardial lung transplantation suitable for all of these patients? We had an occasion to evaluate hilar and mediastinal structures in a case undertaken to lung volume reduction surgery. We observed multiple mediastinal calcified lymph nodes from superior paratracheal to inferior ligament and each were bounded by a fibrous tissue. In particular, lymph nodes of aortico-pulmonary window were conglomerated and adhered firmly so that we hardly performed mediastinal dissection. Mediastinal and visceral pleura were sclerotic and had lost their elasticity. Considering these findings; our opinion is that the extra pericardial mediastinal dissection of the vessels could not be carried out safely and surgeons should make provision against an intrapericardial vessel anastomosis.
KEYWORDS
• Silicosis
• Lung transplantation
• Mediastinal
• Calcification
CITATION
Kuman NK, Çokp?nar S (2015) Mediastinal evaluation of Silicosis according to Lung Transplantation. J Surg Transplant Sci 3(1): 1010.
DEAR EDITOR,
Silicosis is an incurable lung disease caused by the inhalation of dust containing free crystalline silica. Progressive Massive Fibrosis has a prevalence of 75% in chronic silicosis [1], and presents with accelerated silicosis. Emphysematous changes may exist in patients with chronic silicosis [2]. Pulmonary nodules in the lung parenchyma are usually detected - typically located in the upper lobes [2].
A 48 year old man was admitted to our clinic with a severe dyspnea. In his medical history, there was an occupational silica exposure while working in a quartz mine for 7.5 years. He was diagnosed with tuberculosis 10 year ago; had experienced left pneumothorax twice in the recent four years and he has COPD since then. As we had learned; he had applied to the emergency services with dyspnea once every two days, lately.
In his physical examination, the expiration was found to be elongated and the breath sounds were decreased on both upper zones. Bilateral supraclavicular lymphadenomegaly were detected.
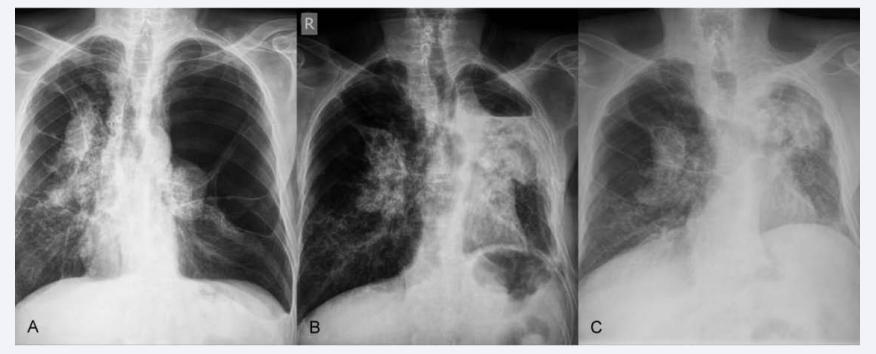
On his chest radiogram, a giant bulla compressing the mediastinum to the right (in left upper and middle zones) and also a bullous parenchyma in the right upper zone were observed. Bilateral irregular hilar zone and micro nodular lower zone densities were observed (Figure 1).
Figure 1: Chest graphics showed mediastinal shift to the right hemithorax before the operation because of a giant bulla (1a), Residual space on upper left hemithorax following operation (1b), Mediastinal shift to the left and bulla formation following disappearing residual space (1c).
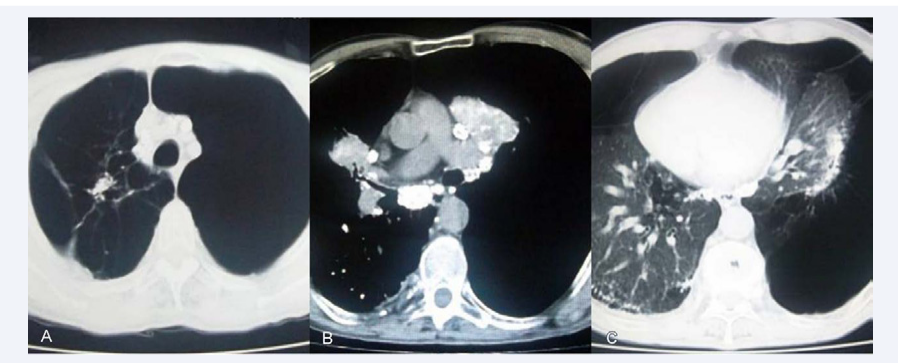
Thorax computed tomography demonstrated paratracheal, carinal and hilar multiple calcified lymph nodes. Bulla formation in various sizes in the right and a giant bulla in the left hemithorax with parenchymal interstisial fibrosis were observed (Figure 2).
Figure 2: CT showed bulla bilaterally upper lobes (2a), Mediastinal, hiler and intraparenchymal nodes calcification (2b), Calcification of compressed left lower zone at preoperative period (2c).
Left thoracotomy was performed for lung volume reduction surgery. During the operation, it was observed that the upper lobe was almost comprised of a 18 cm sized bulla; and no parenchyma was left beside numerous peribronchial and hilar calcified lymph nodes that surrounded and narrowed the superior lobe bronchus. Bulla formation was observed in posterior segment of lower lobe and the same calcified enlarged lymph nodes surrounded its segmental bronchi, at the same time. Multiple micro nodular calcifications were palpated in the rest of parenchymal area.
Lung transplantation is the only chance for the definitive treatment of these cases. However, mediastinal dissection might be difficult due to the mediastinal fibrosis and calcifications. In the literatüre it has been reported that undergoing lung transplantation for other severe occupational lung diseases might carry high- risk of death in the following first year [3]. But we didn’t encounter any issue on the silicosis cases studying the mediastinal operative evaluations. This case made us think that silicosis allocates these cases from the other lung transplantation candidates by its destruction of the structure of mediastinum. Frankly, the same findings such like pleural thickening, mediastinal and pleural adhesions, fibrosis (etc.) might be seen in some other conditions necessitating transplantation adhesion. Yet, in a study on radiological appearances in silicosis cases; the presence of calcified lymph nodes were reported as 85% and were located predominantly in the hilar zone which showed diffuse nodal calcification [4]. Even this high rate seems lower to us; when we compare the mediastinal calcifications reported in thorax CT images with our intraoperative macropathological findings which might be pronounced as petrification. We found CT examination insufficient to evaluate the mediastinum in this case because the total perceivable/palpable calcified area was twice as much. Unfortunately, there is no way to transfer the intraoperative date exactly.
In our case, it was observed that hilar nodular calcification was centered around the bronchus; and caused the upper lobe and lower lobe superior parts to become just like a giant bulla. The fact that intraparanchimal calcifications were palpated among all basal segments to the contrary of non- calcified nodules around its bronchus has given rise to the thought that the main reason of severe paranchimal damage is due to the progressive air trapping beyond the obstructed part up to the check valve mechanism created by rather than fibrosis.
Pulmonary hilus was just like a 8- 10 cm rock lying through carina. In particular, lymph nodes of aortico-pulmonary window were conglomerated and adhered firmly so that we hardly performed mediastinal dissection. Furthermore; sclerotic fibrosis, calcification and loss of elasticity was detected in the mediastinal and parietal pleura. Multiple mediastinal calcified lymph nodes were observed from superior paratracheal to inferior ligament and each were bounded by a fibrous tissue
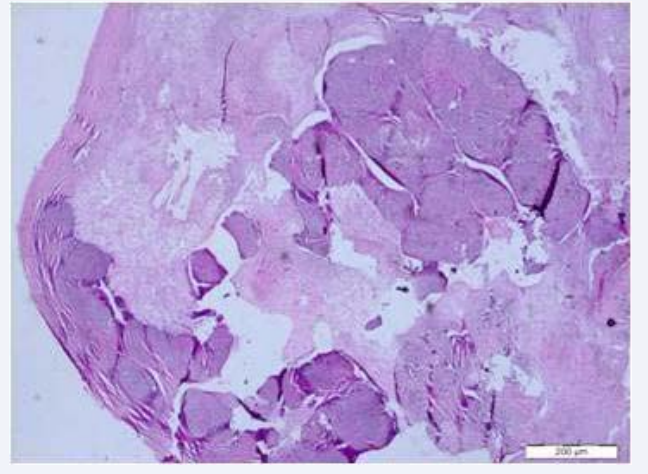
We decided to carry out a lymph node biopsy through the parathymic area far from the vessels and a partly soft one. Obviously, the sounds were just like a scissors scraping over the stone while dissecting mediastinal pleura and lymph nodes were like a rock (Figure 3).
Figure 3: Inflamed fibrous cyst wall and calcified fibrotic node was revealed in pathologic examination (HE X50).
Bulla excisions were performed during operation.
Considering this case in terms of lung transplantation, we may say that it was impossible to carry out mediastinal dissection. In our opinion, intrapericardial dissection of the vessels seems to be more reliable in cases with similar peculiarities. In silicosis cases, surgeons should make provision against an intrapericardial dissection and vessel anastomosis. Bronchus dissection might be a serious problem during operation. It might be necessary to go deeper in order to find a healthy bronchus suitable for anastomosis. An operation by transsternal cardiopulmonary bypass may be an option in such cases. Additionally, surgeons should approach to tomography images with suspicion and consider that fibrosis and calcification might have influenced a broader area. Of course, all cases will present with different features. On the other hand, we believe that adequate preoperative arrangements will provide a safer surgery.
ACKNOWLEDGEMENT
We thank to Özge Karakaya MD, for her English editing.
Presented in part at the 16th Annual Congress of the Thoracic Society of Turkey in Antalya on April 2013