The Effects of Preoperative Imaging on Negative Appendicectomy Rates: A Retrospective Cohort Study
- 1. Department of General Surgery, Queen Elizabeth Hospital, UK
- 2. South Thames Foundation Deanery, England, UK
ABSTRACT
Background: Acute appendicitis is the most common abdominal surgical emergency, yet its diagnosis remains difficult with high negative appendicectomy rates (NAR) reported throughout the United Kingdom (UK). High NARs are associated with increased risk of morbidity. Recently guidelines have suggested the use of preoperative imaging modalities to reduce this; however these are not routinely followed in the UK. Our aim was to assess the effects of preoperative imaging on the NAR.
Methods: Retrospective cohort study of all appendicectomies at a London District General Hospital over a one-year period. Examining histological data taken from tissue intraoperatively and examining reports of imaging conducted prior to operation.
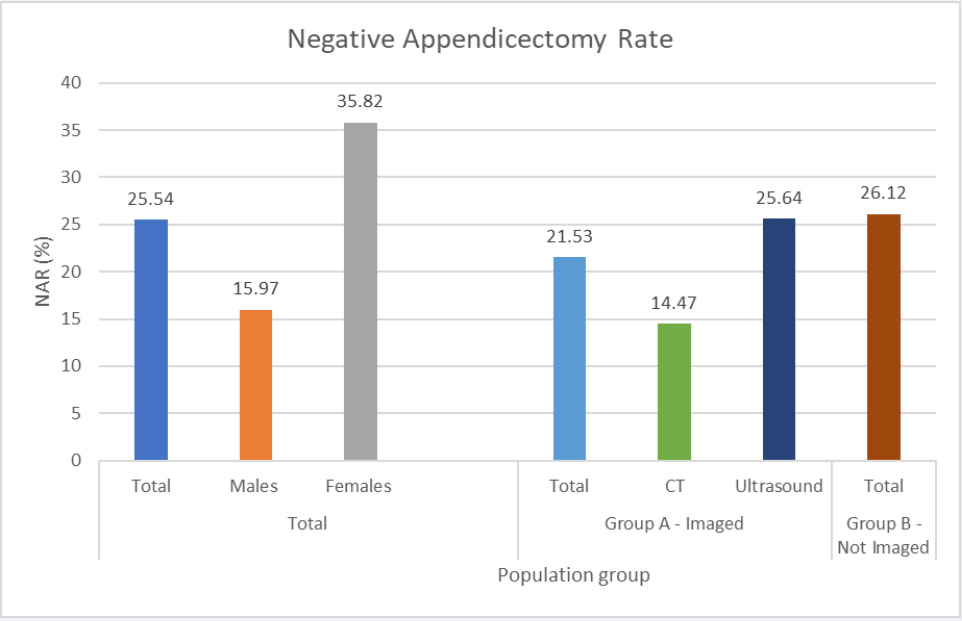
Results: The total NAR was calculated at 25.54%. Females had a higher NAR. (35.82% Vs 15.97%) (p<0.05). No significant difference in the NAR was seen between patients who underwent preoperative imaging and those who did not (21.53% Vs 26.12% (p=0.8908)).
Conclusion: The use of preoperative imaging in our centre does not alter the NAR. The high rate of inconclusive ultrasound reports could contribute to this. UK guidelines for the secondary care management of suspected appendicitis are needed to reduce the NAR; careful consideration for the use of preoperative imaging should be used whilst conducting these guidelines.
KEYWORDS
• Appendicitis; Preoperative imaging; Negative
appendicectomy rates
CITATION
George R, Lyon RJ, Cheng Hin PN (2020) The Effects of Preoperative Imaging on Negative Appendicectomy Rates: A Retrospective Cohort Study. J Surg Transplant Sci 7(1): 1074.
INTRODUCTION
Acute appendicitis is the most common abdominal surgical emergency with a prevalence of 6-8% [1,2]. Despite this, the diagnosis remains difficult, with high negative appendectomy rates (NAR) reported in the United Kingdom (UK), between 19-33% [3-7]. These high NARs are associated with increased postoperative morbidity, significant cost implications and rarely mortality [4,8]. A nationally accepted NAR has not been agreed, however, a NAR of around 15% has been suggested as the appropriate figure to sufficiently reduce the rate of severe complications whilst also treating all cases of appendicitis [4].
Methods of reducing the NAR are debated; one such method used increasingly, and included in multiple guidelines, is the use preoperative diagnostic imaging for suspected appendicitis [9,10]. This has been shown to reduce NAR worldwide [11-13].
However, the use of preoperative imaging to accurately diagnose appendicitis is debated, with guidelines often differing significantly from one another, for example the European Association of Endoscopic Surgery primarily advocating the use of ultrasound, In comparison to the American Radiology guideline which suggests the use of Computerised Tomography (CT) [9,10]. CT is reported to have a high sensitivity and specificity but exposes patients to radiation, whilst ultrasound, although cost effective and relatively harm free, is widely reported to have low sensitivity in the UK with high reported rates of inconclusive results; primarily as it is very much user dependent [13-17].
It is unclear if the use of preoperative imaging in patients with suspected appendicitis significantly alters the NAR in the UK population.
Our aim was to assess whether the use of preoperative imaging modalities used for suspected appendicitis reduced the NAR over a one-year period in a London District General Hospital.
METHODS
A Retrospective cohort study examining appendicectomies at a London District General Hospital; Queen Elizabeth Hospital Woolwich, (QEH) over a one-year period. The aim was to calculate the NAR at the hospital, whilst also investigating whether different modalities of preoperative imaging reduced this rate. Additionally, we calculated the sensitivity, positive predictive value and false discovery rate of the imaging modalities.
All patients who underwent an emergency appendicectomy from the 1st of March 2018 to the 15th of March 2019 were included. Cases involving interval appendicectomies were excluded. All age groups were included. This operation database was received from the hospitals theatre office who conducted a search on the surgical database for all appendicectomies. Data was collected regarding the type of operation using the hospital’s theatre database.
Following this, the patients’ hospital Medical Record Numbers were used to search for imaging conducted at the time of admission prior to operation.
Reports from investigations were read on PACS, the hospitals imaging system these images were either reported by radiographers or radiologists at QEH, or if happening out of normal office hours by radiologists from an outsourcing radiology reporting company - Telemedicine. All ultrasounds were either conducted by radiographers or radiologists at QEH.
No standard was used by radiologists to report scans; for that reason, when reading reports, the following classification was used in order to group the results into four categories (Table 1).
In order to calculate the NAR, histology reports from the appendix taken intraoperatively were viewed using Powerchart, the hospitals technology system. These histology reports were formulated by pathologists at QEH where they are all uploaded onto a patients Laboratory results page. As the reporting of histology varied descriptively, the following classification was used in order to assess tissue examined into four categories (Table 2). The NAR was calculated using this histological data; the total number of negative and ‘other’ histology reports was divided by the total number of appendicectomies to give a percentage.
Results were collected on Microsoft Excel where sensitivity, positive predictive value and false discovery rates were calculated. In order to calculate sensitivity of investigative modalities, inconclusive radiological reports were excluded from the calculation. Mean was used for reporting continuous variables with a standard deviation reported. An Unpaired T-test was used to compare the age difference between Groups. Fishers Exact Test was used to compare the different NAR between groups. GraphPad Prism (Version 8.3.0 for Windows) was used to conduct these statistical tests.
RG and RL conducted data collection and analysis. The data was collected as part of a local audit and therefore ethics approval was not sought.
RESULTS
In total, 291 operations were conducted between the 01/03/2018 and the 15/03/2019. Of these, 278 were emergency appendicectomies. 13 were excluded from our analysis as they were not emergency appendicectomies. 233 were recorded as laparoscopic and 45 were recorded as general (open) appendicectomies. Data was not available regarding laparoscopic converted to open operations due to coding issues. The figure for uptake of Laparoscopic operations was thus 83.81%.
Demographics
144 (51.80%) of patients underwent imaging prior to surgery and were grouped in Group A for analysis. The 134 (48.20%) who did not undergo preoperative imaging were classified in Group B. The population imaged (Group A) were statistically older than those not imaged (Group B). (p<0.001). Group A had statistically more females than Group B. (p=0.0119) (Table 3).
Twelve patients underwent more than one form of imaging investigations prior to operation, of these two underwent a CT first prior to an ultrasound; in both of these cases the CT was reported as negative and the ultrasound was also negative. These two cases underwent operation based on clinical decision alone and on histology were confirmed appendicitis.
Of those that underwent ultrasound first, six went on to have a CT and four underwent repeated ultrasound. Of the twelve that underwent further imaging six (50%) were confirmed appendicitis upon histological examination.
Histology reports
Of the 278 samples sent to the histology laboratory 65 (23.38%) were analysed as being severe appendicitis in nature. 48 (17.27%) of all samples sent to the histology laboratory were of normal appendicular tissue (Table 4).
Negative appendicectomy rate
The total negative appendicectomy rate of our hospital over this one-year period was calculated at 25.54% (Figure 1).
Figure 1: Total NAR across all groups. The NAR for females is statistically higher than males. No difference was seen between the preoperative imaged grouped and non-imaged group.
However, this reduced to 17.27% when the definition of NAR was changed to include ‘Other’ pathology as a successful removal. Females included in the study had a statistically significant increase in NAR in comparison with the males. (35.82% Vs 15.97%) (p<0.05) (Table 5).
NAR did not decrease significantly whilst using preoperative imaging in comparison to clinical judgement alone. (p=0.8908).When further analysing Group A, the population who underwent CT had a statistically significant reduction in NAR in comparison with the population who underwent ultrasound (p=0.0105). There was not a significant reduction in NAR when comparing CT with the non-imaged population (p=0.1714). Only 16 (19.40%) of women underwent a CT scan prior to operation.
Group A did not have a statistically increased number of severe appendicitis on histology in comparison with Group B. (p=0.5713).
The NAR for operations undertaken laparoscopically was calculated as 27.77% in comparison to 13.64% for open procedures.
Inconclusive reports
In total 21.53% of imaging reports were reported as inconclusive; of these the majority were ultrasound reports; with 41.03% of all ultrasound reports inconclusive in comparison to just 3.95% of CT reports.
Of these inconclusive reports 61.29% of patients who went on to have an appendicectomy were found to not have appendicitis upon histological examination.
Sensitivity of imaging modalities
The sensitivity of CT for predicting appendicitis was calculated as 0.97, the positive predictive value was 0.86 with a false discovery rate of 0.14.
The sensitivity of ultrasound for predicting appendicitis was calculated as 0.78, the positive predictive value was 0.91 with a false discovery rate of 0.09.
This is in comparison to clinical judgement alone that had a positive predictive value of 0.75, with a false discovery rate of 0.25.
Table 1: Radiological classification used to assess CT and ultrasound reports.
| Radiological classification | Description |
| Confirmed | Reporting person stated that a diagnosis of appendicitis was clear |
| Probable | Reporting person stated that a diagnosis of appendicitis was likely but advised clinical correlation. |
| Inconclusive | Reporting person neither confirmed or denied a diagnosis of appendicitis |
| Negative | Reporting person stated that the appendix appeared normal or failed to mention the appendix in the report. |
Table 2: Histological classification used to group histology reports of appendicular tissue sent to laboratory intraoperatively.
| Histology classification | Description |
| Confirmed mild | diagnosis of appendicitis confirmed on histology with no features of the severe classification reported in the report |
| Confirmed severe | diagnosis of appendicitis confirmed on histology with additional comments commenting on the assessed tissue being gangrenous, necrotic or perforated. |
| Negative | reported by histology as being normal appendicular tissue |
| Other | Pathology reported in the histology report but no evidence of appendicitis |
Table 3: Demographics of cases investigated. The group that underwent preoperative imaging were statistically older and included more females. Uptake of laparoscopic surgery was 83.31%.
| Total N (% of total) | Mean Age (standard deviation) | |
| Total | 278 | 31.32 (15.68) |
| Total Females | 134 (48.20%) | 30.84 (13.03) |
| Total Males | 144 (51.80%) | 31.77 (17.83) |
| Total Laparoscopic | 233(83.81%) | |
| Group A | Total N (% of total in group) | |
| Imaged | 144 | 37.36 (17.52) |
| Imaged females | 80 (55.56%) | 33.69 (13.94) |
| Imaged males | 64 (44.44%) | 41.95 (20.37) |
| Group B | Total N (% of total in group) | |
| Not imaged | 134 | 24.84 (10.00) |
| Not imaged females | 54 (40.30%) | 23.64 (9.69) |
| Not imaged males | 80 (59.70%) | 26.61 (10.30) |
Table 4: Histological data collected intraoperatively examined at hospitals pathology laboratory. 8.27% of appendicular tissue examined was classified as other upon histological examination. With 3% of the total being Enterobius Vermicularis invasion.
| Pathology | Total | Percentage of total (%) |
| Severe | 65 | 23.38 |
| Mild | 142 | 51.08 |
| Negative | 48 | 17.7 |
| Other | 23 | 8.27 |
| Enterobius Vermicularis | 7 | 2.52 |
| Pelvic Inflammatory Disease | 3 | 1.08 |
| Diverticulitis | 3 | 1.08 |
| Inflammatory Bowel Disease | 2 | 0.72 |
| Endosalpingiosis | 2 | 0.72 |
| Neuroendocrine Tumour | 2 | 0.72 |
| Lymphoma | 1 | 0.36 |
| Plant Seed | 1 | 0.36 |
| Omental Necrosis | 1 | 0.36 |
| Adenoma | 1 | 0.36 |
Table 5: Change in definition of Negative Appendicectomy Rates. NAR when including ‘other’ pathology as a positive finding.
| Group | Negative Appendicectomy Rate excluding ‘Other’ |
| Total | 17.27 |
| Imaged (A) | 18.75 |
| Not Imaged (B) | 15.67 |
DISCUSSION
Our NAR is comparable with other studies across the United Kingdom [3,4,14]. We, like many others, demonstrated that the NAR in the female population is significantly higher in comparison to males [1-4]. With a change in the definition of NAR which included the removal of ‘other’ pathology as a positive intraoperative finding the NAR reduced. However, although comparable with the UK population the reported NARs are higher in the UK in comparison with other European countries [18].
A high NAR, as reported here, is associated with significant postoperative morbidity, increased financial burden on hospitals and rarely death [4,8]. A worldwide accepted NAR has not formally been agreed, however, an acceptable target has been suggested at 15% in order to decrease the morbidity associated with appendicectomies whilst also avoiding the complications of untreated appendicitis [4]. However, numerous studies state that this is too low in a female population due to the increased number of differential diagnosis [3,5,6,19]. Our NAR, even when using the alternative definition, is higher than this 15%.
We additionally see a higher rate of NAR in the population who underwent laparoscopic appendicectomies, this may be a result of a proportion of these being diagnostic laparoscopies. The introduction of diagnostic laparoscopies as an investigative modality has increased the NAR at some centres as it is felt that removing normal appendicular tissue is a positive as it means that a patient will not then suffer from appendicitis however these procedures are associated with their own morbidities.
We demonstrate that there is not a significant reduction in NAR when using preoperative imaging. Worldwide lower NAR have been reported, often as strict guidelines are followed and operations only undertaken if appendicitis has been confirmed by imaging [9,11,12].
Interestingly we again highlight the significant difference in NAR between males and females, like a recently published UK study, that has been discussed in national newspapers, nearly a third of all females who underwent an appendicectomy did not have appendicitis upon histological examination [18]. These authors suggested that using CT preoperatively could be the best way to reduce this rate in females and we agree with this suggestion as only 19.40% of females underwent CT investigation in our study.
Unlike our study, there are multiple reports that have demonstrated that preoperative imaging significantly reduces the NAR [11,12,20]. These studies however conduct almost mandatory preoperative imaging on patients prior to operating, whereas in our hospital imaging is not routinely undertaken and is often only conducted in patients where an alternative diagnosis is highly suspected. Additionally, our imaged population group were statistically older and included more females with both of these population groups known to have higher NAR values. One plausible reason for this difference in our study variables is that current guidelines, including the European Association of Endoscopic Surgery state, that patient over the age of fifty should have imaging conducted prior to an operation due to the higher incidence of pathology other than appendicitis causing right iliac fossa pain [9]. This may also explain why more females were imaged as the likelihood of a differential diagnosis is higher in this population [1].
US, guidelines state that CT is the imaging modality of choice when investigating right iliac fossa pain [10], which could explain why the NAR is lower in studies across the United States in comparison to our study and others across Europe, as CT is known to have high sensitivity and specificity when investigating appendicitis [13,17,20,21]. We again highlight the high sensitivity of CT in this study. CT is not the imaging modality of choice in the United Kingdom primarily as the radiation exposure is seen as a risk. Recently low dose radiation CT has been shown to be as good at diagnosing appendicitis [22]. Perhaps this could be used more frequently in hospitals as an alternative to normal CT and ultrasound.
Low NAR has been seen in the Netherlands as a result of using almost mandatory preoperative ultrasound [11]. In these studies, the operators conducting ultrasound are highly trained. We demonstrate a worryingly high rate of inconclusive ultrasound reports in this study with the majority of these patients going on to have normal appendicular tissue removed intraoperatively.
We did not investigate who was reporting the ultrasounds in this study; this is something that should be investigated in the future. Perhaps to reduce this high rate of inconclusive reports we should better train specific users or use consultant radiologists with a specialist interest in abdominal ultrasound as this has been shown to increase the sensitivity of ultrasound whilst also decreasing the NAR [14,16,23]. Recently it has been shown that training surgical trainees to conduct ultrasound abdomens at the bedside to investigate appendicitis could be beneficial and both cost and time effective [24,25]. This needs further investigating but could be used to reduce the number of inconclusive reports whilst also aiding diagnosis as having the clinician undertake the investigation has been shown to be beneficial in reducing NAR [25].
To our knowledge no clear guideline regarding the secondary care management of suspected appendicitis in the United Kingdom is followed routinely in hospitals. Due to the high variability of reported NAR in the United Kingdom a national guideline that incorporates preoperative imaging for certain population groups is needed.
Limitations
As this study was retrospective in nature, we were unable to assess how many patients were referred to surgeons with suspected appendicitis and the results of these referrals. We were therefore unable to calculate the specificity and sensitivity of clinical judgement alone. We did not collect data regarding the number of ultrasounds or CTs that successfully ruled out appendicitis whilst being undertaken for right iliac fossa pain; as a result of this we were unable to calculate the specificity of these imaging modalities. A study examining all of requests for imaging that included a query for appendicitis and their subsequent results would be beneficial. Additionally, we did not consider variables such as body habitus and their effects on the choice of imaging modality. We also did not consider diagnostic laparoscopies that were conducted and did not proceed to appendicectomy. It would be of interest to conduct a study investigating the effects of diagnostic laparoscopy on NAR and to also investigate whether variables such as lymphocyte count had an effect on the choice of investigation used.
CONCLUSION
NAR is not significantly affected by any form of preoperative imaging in our centre; this may be attributed to the high number of inconclusive ultrasound reports in this trust. Specific training is needed for certain ultrasound user in order to reduce this rate, this could be achieved by training surgical trainees to undertake these scans which would have the added benefit of them having undertaken the clinical examination which has been shown to increase specificity and sensitivity. More research is needed to investigate the value of surgeon performed ultrasound. By reducing these inconclusive rates, the NAR could be reduced. Additionally, a United Kingdom specific guideline is needed for the secondary care management of appendicitis as the variability between centres is high; this guideline should include the use of CT as we again demonstrate that this is the most successful modality at reducing NAR.
CONTRIBUTIONS
The Authors would like to thank the theatre office staff at Queen Elizabeth Hospital who retrieved the data from the hospitals theatre database.