The Relationship of Restech Ph Probe Results with Laryngopharyngeal Reflux Symptomatology and Examination Findings
- 1. Department of Otolaryngology—Head & Neck Surgery, University of Kentucky College of Medicine, USA
- 2. Department of Otolaryngology—Head & Neck Surgery, Medical University of South Carolina, USA
- 3. Department of Otolaryngology—Head & Neck Surgery, Indiana University School of Medicine, USA
ABSTRACT
Objectives/Hypothesis: To determine the utility of the new Restech pH-probe in diagnosis of laryngopharyngeal reflux by showing that patients with higher Reflux Symptom Indices and Reflux Finding Scores will have positive Restech studies.
Study design: Retrospective study.
Methods: The charts of all patients with suspected laryngopharyngeal reflux who presented between 1/2007 and 4/2008 to the Indiana University Clinic for Swallowing and Voice Disorders and underwent Restech evaluations were reviewed. Initial Reflux Symptom Indices and Reflux Finding Scores were recorded, as well as initial Restech findings. The association between abnormal Restech findings and elevated scores and indices were then determined, with student t-test used to determine statistical significance.
Results: Twenty patients were included in the study. Of these, thirteen patients (65%) had positive pH events during Restech evaluation. Sixteen patients (80%) of patients had Reflex Symptom Index of 10 or greater. Eighteen patients (90%) had Reflux Finding Scores of 7 or greater. There was a trend toward a higher scores and indices in the patients (n=9) with the abnormal Restech results, but this difference did not reach significance when all patients were included. When those patients who had diffusely elevated review of systems (greater than 10 complaints) were excluded, those patients with abnormal Restech (n=6) had significantly higher scores and indices (p=0.047 and p=0.030, respectively) than those patients with normal studies (n=10).
Conclusion: The Restech pH-probe may be a useful diagnostic tool for patients with laryngopharyngeal reflux in correlation with symptoms and examination findings.
KEYWORDS
• Transplantation
• Homologous
• Laser therapy
• Low-level
• Cryopreservation
CITATION
de Moreno LCA, Oyer SL, Halum SL (2014) The Relationship of Restech Ph Probe Results with Laryngopharyngeal Reflux Symptomatology and Examination Findings. J Surg Transplant Sci 2(1): 1005.
INTRODUCTION
Laryngopharyngeal reflux is a common problem encountered among the patient population of otolaryngologists. Laryngopharygeal reflux commonly occurs in the presence of gastroesophageal reflux disease, or GERD, which is the movement of gastric contents into the esophagus without belching or vomiting. Laryngopharyngeal reflux, or LPR, occurs in the same manner except that gastric contents move into the larynx as well. LPR has been implicated in many otolaryngologic disorders, including chronic laryngitis, chronic dysphonia, laryngotracheal stenosis, head and neck carcinoma, cough, asthma, otitis media, dental cares and erosion, laryngeal papilloma, vocal fold granulomas and ulcers, laryngospasm, recurrent croup, and laryngomalacia. Current therapy is treatment with Proton Pump Inhibitors (PPIs) [1]. In order to gauge response to PPI treatment, laryngologists often use patient-generated questionnaires and findings on physical examination. Belafsky, Postma, and Koufman developed the Reflux Symptom Index (RSI), which is a questionnaire of nine questions given to patients to assess their symptomatology (Table 1) [2].
Table 1: Reflux Symptom Index (RSI).
|
Hoarseness or a problem with your voice |
|
Clearing your throat |
|
Excess throat mucus or postnasal drip |
|
Difficulty swallowing food, liquids, or pills |
|
Coughing after you have eaten or after lying down |
|
Breathing difficulties or choking episodes |
|
Troublesome or annoying cough |
|
Sensations of something sticking in your throat or a lump in your throat |
|
Heartburn, chest pain, indigestion, or stomach acid coming up |
Within the past month, how did the following problems affect you? Rank them from 0 (no problem) to 5 (severe problem).
In order to grade the severity of physical findings in patients with LPR, Belafsky and colleagues also developed the Reflux Finding Score (RFS), which is made of eight findings and graded on a severity that can yield a score from 0 to 26 (Table 2) [3].
Table 2: Reflux Finding Score (RFS).
|
Pseudosulcus |
0, absent; 2, present |
|
Ventricular obliteration |
0, none; 2, partial; 4, complete |
|
Erythema/hyperemia |
0, none; 2, arytenoids only; 4, diffuse |
|
Vocal fold edema |
0, none; 1, mild; 2, moderate; 3, severe; 4, polypoid |
|
Diffuse laryngeal edema |
0, none; 1, mild; 2, moderate; 3, severe; 4, obstructing |
|
Posterior commissure hypertrophy |
0, none; 1, mild; 2, moderate; 3, severe; 4, obstructing |
|
Granuloma/granulation |
0, absent; 2, present |
|
Thick endolaryngeal mucus |
0, absent; 2, present |
Continuous dual pH probe monitoring studies are currently the gold standard study for diagnosis of LPR. Dual pH probes include acid-detecting probes located in the lower esophagus and at or superior to the upper esophageal sphincter. While the dual pH probe study is highly sensitive (80% or higher) in detecting acid reaching the laryngopharynx, the test is very uncomfortable, which limits is clinical applicability. Based on dual pH probe criteria, an RSI of 10 and a RFS of more than 7 is associated with a high likelihood of having a dual-channel pH probe study that is positive for LPR (upper probe acid exposure) [4]. Because of the patient discomfort involved in dual pH testing, many studies omit pre-therapeutic and/or post-therapeutic pH testing and use ‘empiric therapy’ models, thereby adding confusion in the LPR literature. Recently a single pharyngeal pH probe test has been developed by Restech (Respiratory Technology Corporation, San Diego, CA), which, in preliminary studies, has been suggested to have validity and reliability consistent with that of the upper probe in a dual pH study. The probe is designed to detect aerosolized particles and to record pH [5-8]. Due to its location above the hypopharynx and epiglottis, the swallowing mechanism is not disrupted. Because the probe has no esophageal component, it is extremely well tolerated by patients with virtually no discomfort, thereby being conducive to a study with pre and post-therapeutic pH testing. It is hypothesized that, in patients with Restech-probe proven LPR, patients will demonstrate higher pre-therapeutic RFS on examination and higher RSI on questionnaire compared to patients who do not have LPR. If confirmed with patient data, the validity of the Restech probe as a diagnostic test for LPR would be supported.
METHODS
After obtaining approval from the International Review Board at Indiana University School of Medicine, the charts of all patients previously undergoing Restech probe testing were reviewed to determine if those patients with abnormal Restech probes had increased RFS and RSI relative to those patients with normal Restech studies. Patients were de-identified. A retrospective chart review was performed on patients who had been previously seen and treated at the Indiana University Clinic for Swallowing and Voice Disorders from January 2007 to April 2008. Patients were excluded if they had any underlying neurologic disorders causing throat-related symptoms, dysphagia related to previous head and neck chemoradiation, an RSI with a score less than 5 (indicating an incomplete survey), or incomplete data (RFS or RSI) in their charts.
As is standard in the Indiana University Clinic for Swallowing and Voice Disorders, all new patients presenting to the clinic completed a RSI, and were assigned an initial RFS based on videostroboscopy examination at their initial visit. In patients with presumed LPR, Restech pH probe studies were ordered diagnostically as is standard practice in the clinic. Patients had probes in clinic through one naris and positioned in the oropharynx, just posterior to the uvula, and confirmed with direct visualization. The patients wore the probes for 24 hours before removal. Results were then reviewed by an IUSM gastroenterologist or the senior author (SLH). Any events with a pH <6 were recorded, excluding those that coincided with meals as a false positives.
Patients’ demographic information including height, weight, age, and gender were recorded. In addition, comorbities, medications, itemized RSI and RFS were noted. None of the patients were taking PPIs at the time of the Restech study; however, if they were taking PPIs at the time of initial presentation, this was recorded. The number of positive system complaints self-reported by the patients on review of systems (ROS) questionnaire was also noted. There were a total of 15 systems that patients could report experiencing symptoms, and those patients with greater than 10 system complaints were considered to have diffusely elevated ROS for the purposes of this study. Statistical analysis was done using student t-test, with a p value of <0.05 determining significance.
RESULTS
The charts of 20 patients who met inclusion criteria were reviewed. Ages ranged from 16 to 79. There were 15 females (75%) and 5 males (25%). Weights ranged from 103.7 pounds to 347 pounds. Basal mass indices (BMI) could be calculated for 11 patients based on chart information; two of these patients (18%) were overweight based on their BMI [9]. Nine patients had previously been on either once daily (n=4) or twice daily (n=5) PPI therapy. Four patients had diffusely elevated ROS (more than 10 of 15 system complaints). These same four patients reported difficulties with anxiety, and were the only patients in the series taking anxiolytic medications.
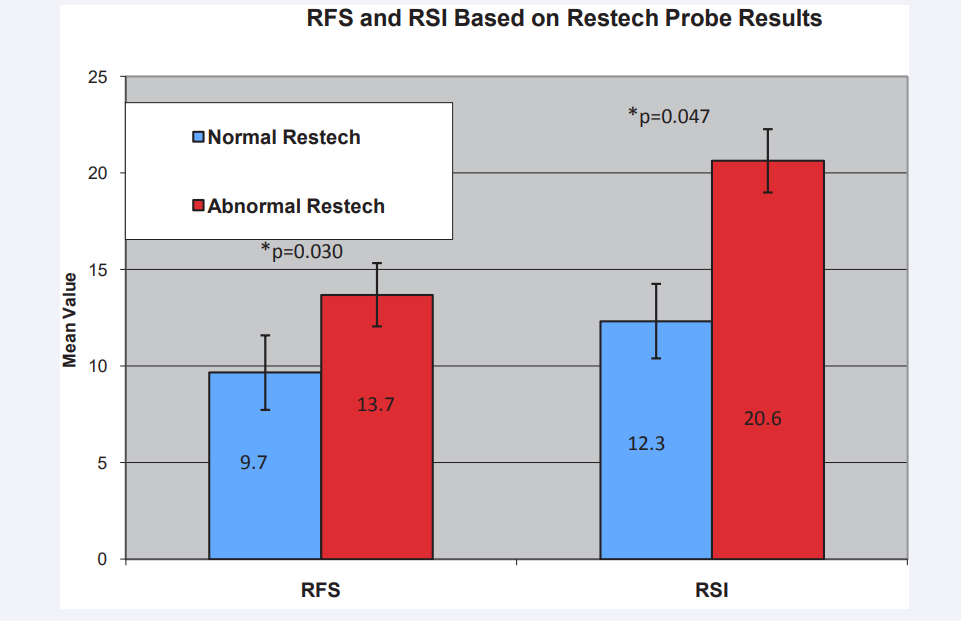
Thirteen patients (65%) had abnormal Restech pH evaluations, as defined by two or more acidic pH events (pH <6) during the 24 hour evaluation. These patients had a mean RFS of 13.7 and RSI of 20.6, while those with negative Restech studies had a mean RFS of 12 and RSI of 18.1 (p= 0.25 and p=0.20, respectively). Interestingly, when the four patients with diffusely elevated ROS were excluded, the mean RFS and RSI were 13.7 and 20.6, respectively, for those patients with abnormal Restech studies (n=10). These values were significantly higher than the mean RFS of 9.7 and mean RSI of 12.3 in those patients with normal Restech studies [(p=0.030 and p=0.047, respectively) see (Figure 1)].
Figure 1: * = significant difference (p<0.05) between normal and abnormal Restech patients. Data excludes patients with diffusely elevated ROS.
DISCUSSION
LPR remains an elusive entity to diagnose. Physical examination alone appears insufficient for diagnosis. Even asymptomatic individuals have signs of posterior laryngeal irritation on endoscopic examination as shown by Milstein [10]. Furthermore, Park demonstrated that RSI and RFS, when used independently for LPR diagnosis, have suboptimal validity [11]. Meta-analysis has shown that the upper probe alone on dual pH probe testing demonstrates a significant difference in amount of Within the past month, how did the following problems affect you? Rank them from 0 (no problem) to 5 (severe problem).
acid exposure time compared to normal subjects, supporting its current role as the gold standard for LPR diagnosis [12].
Recently the Restech pH probe has emerged as a more comfortable probe for patients due to its positioning in the oropharynx. However, there are no previous studies investigating the relationship between Restech pH probe results and the LPR symptomatology/examination findings. This is a difficult relationship to assess for several reasons. First, while the current standard is for any two or more events (pH <6.0) to be considered a positive Restech study, no studies have actually established how many positive pH events are needed to stand as a positive study. Additionally, since the RSI is a subjective rating on the part of the patient, the results depend on the patient’s perception of their degree of “impairment” and this is unlikely to correlate with objective test results in some patients. Regarding inflated RSI ratings, we found a highly elevated ROS (greater than 10 positive systems) was a strong predictor of an unusually inflated RSI. Furthermore, all of the patients with this diffusely elevated ROS were on anxiolytic medications, suggesting a possible relationship between anxiety and diffusely elevated ratings on subjective self-assessment tools such as ROS and RSI. Surprisingly, the RFS was also elevated in some of these patients, possibly reflecting physician bias related to the physician knowing the RSI at the time of the videostroboscopy examination. Regardless, when the patients with diffusely elevated ROS were excluded from the analysis, those patients with abnormal Restech pH probe studies had significantly higher RFS and RSI than those patients with normal Restech studies. Thus, this data supports a positive association between the RSI, RFS and Restech probe results, which helps support the validity of the Restech probe as a diagnostic tool for LPR.
Future studies involving larger patient numbers will be necessary to help validate the Restech system as a diagnostic test for LPR. Additionally, investigating the positive predictive value of the Restech test (for predicting a positive response to PPI therapy) will be helpful in establishing it as a clinically useful diagnostic test, and such studies are currently underway at our institution.
Table 1: Reflux Symptom Index (RSI).
| Hoarseness or a problem with your voice |
| Clearing your throat |
| Excess throat mucus or postnasal drip |
| Difficulty swallowing food, liquids, or pills |
| Coughing after you have eaten or after lying down |
| Breathing difficulties or choking episodes |
| Troublesome or annoying cough |
| Sensations of something sticking in your throat or a lump in your throat |
| Heartburn, chest pain, indigestion, or stomach acid coming up |
Table 2: Reflux Finding Score (RFS).
| Pseudosulcus | 0, absent; 2, present |
| Ventricular obliteration | 0, none; 2, partial; 4, complete |
| Erythema/hyperemia | 0, none; 2, arytenoids only; 4, diffuse |
| Vocal fold edema | 0, none; 1, mild; 2, moderate; 3, severe; 4, polypoid |
| Diffuse laryngeal edema | 0, none; 1, mild; 2, moderate; 3, severe; 4, obstructing |
| Posterior commissure hypertrophy | 0, none; 1, mild; 2, moderate; 3, severe; 4, obstructing |
| Granuloma/granulation | 0, absent; 2, present |
| Thick endolaryngeal mucus | 0, absent; 2, present |
CONCLUSION
The Restech probe is evolving as an effective test in diagnosing LPR. It has a positive association with RSI and RFS results, especially in patients without a previous history of anxiety.