Does Intensivist Management of Organ Donors with Death by Neurological Criteria Result in Increased Organ Yield?
- 1. Department of General Surgery, University of Missouri-Kansas City School of Medicine, USA
- 2. Department of Psychiatry, Christiana Care, USA
- 3. Department of Occupational Medicine, University of Missouri-Kansas City School of Medicine, USA
- 4. Department of General Surgery, Mercy Iowa City, USA
- 5. Department of Bariatric Surgery, Dartmouth Hitchcock Medical Center, USA
- 6. Organ Procurement Services, Midwest Transplant Network, USA
- 7. Wound Care and Hyperbaric Medicine Center, Ascension Via Christi, USA
- 8. Department of General Surgery, Wesley Medical Center, United States
- 9. Office of the Senior Associate Dean for Clinical Affairs, University of Missouri Health Care, usa
- 10. Department of Internal Medicine, University of Kansas Health System, United States
- 11. School of Science and Engineering, University of Missouri-Kansas City, United States
- 12. School of Medicine, University of Missouri-Kansas City, USA
Abstract
Objective: To determine whether intensivist management of donors increases the number of organs available for transplantation from organ donors with death by neurological criteria.
Setting: The Midwest Transplant Network from January 2003 – October 2018.
Interventions : Intensivist physicians engaged in donor management. Comparison of total number of donors, donor age, and organs transplanted of all organ types before and after intensivist management. Analysis using ANOVA and 2 sample t-tests used to compare organ donations before and after intensivist management with a p-value of <0.05 deemed statistically significant.
Results : The number of organs transplanted showed a statistically significant increase after intensivist management for most organs. The number of organs transplanted increased by 38% (p-value=0.009) and the number of donors increased by 28% (p-value=0.026) following intensivist management. Donor age was significantly higher post-intensivist management (35.83 ±18.79 vs. 38.89 ± 22.86, p-value=0.0007). The number of organs transplanted per donor increased significantly after intensivist management (2.76 ± 1.82 vs 2.94 ± 1.89, p-value=0.038).
Conclusion: Our data suggest an increase in organs transplanted per donor may be associated with the involvement of a critical care specialist. Future research should explore the exact patient-centered implications.
Keywords: Brain Death; Intensivist; Organ Donation; Quality and Patient Safety; Transplantation
Abbreviations: OPO: Organ Procurement Organization; MTN: Midwest Transplant Network; IRB: Institutional Review Board; CCTF: Critical Care Task Force; DSA: Donor Service Area; OPC: Organ Procurement Coordinators; DCD: Donation After Circulatory Death; DMG: Donor Management Goal; MAP: Mean Arterial Pressure; CI: Cardiac Index; IM: Intensivist Management; SRTR: Scientific Registry for Transplant Recipients; ANOVA: Analysis of Variance
Introduction
The demand for solid organ transplantation has increased substantially over the last few decades, despite comparatively gradual increases in the rate of donation [1]. The number of patients on the waiting list for transplantation has doubled over the last 25 years, with the largest increase noted in the 50–64-year-old age bracket [2]. Further, as the duration of diminished organ function prolongs, so does the likelihood of developing comorbid diseases, complications, and death. According to the United States Department of Health and Human Services, there are about 104,234 patients awaiting transplantation at this time, yet only 42,888 transplant surgeries were performed in the year 2022 [3]. Many of the patients currently waiting will progress to complete organ failure without transplantation and die as a result. According to the Health Resources and Services Administration, approximately 17 patients die every day while waiting for an organ, as of April 2023. In order to meet the demand, various strategies have been employed by the medical community and organ procurement organizations (OPO) to utilize what were previously considered marginal organs. Physicians with critical care training may be able to offer valuable expertise on donor management. This can be accomplished by employing evidence-based critical care management strategies, such as fluid resuscitation, aggressive treatment of sepsis, advanced ventilator strategies, triple hormone therapy, and prevention of cardiovascular instability through hemodynamic monitoring [2,4,5]. Through these strategies, organs may be managed in a way that increases organ viability for procurement. Previous studies have shown intensivist-led teams are able to increase the number of organs available for transplantation in a sample of potential organ donors with death by neurological criteria [6-10]. The purpose of our study is to determine whether intensivist-led management of donors increases the overall number of transplanted organs across a wide range of donor demographics. We hypothesize that donors managed with critical care involvement will demonstrate an increase in organs transplanted per donor and percent of organs transplanted.
Materials and Methods
A retrospective review was completed by Midwest Transplant Network (MTN) on all organ donors whose death was declared by neurological criteria from January 2003 to October 2018. Primary data analyzed included number of organs procured and transplanted per donor, percent of organs donated, and transplant outcomes. Secondary data analyzed included donor demographics, OPO yield calculations, and organ type. Organ types included heart, lung, liver, kidney, pancreas, and intestine. The protocol was reviewed by the University of Missouri-Kansas City’s Institutional Review Board (IRB) and was approved as Non-Human Subjects protocol. A Critical Care Task Force (CCTF) was developed in 2005, shortly after MTN became involved in the Organ Donation and Transplantation Breakthrough Collaborative. This task force consisted of critical care physicians from major donor hospitals in the MTN donor service area. In addition, a variety of specialties were represented including trauma and acute care surgery, pulmonary medicine, anesthesia, infectious disease, and pediatrics. As a result of this initiative, a number of critical care and evidenced-based strategies were employed to the management of the brain-dead organ donor as seen in Table 1. This eventually led to the development of a 24/7 critical care call schedule beginning 1/1/2006 in which a member of the CCTF was consulted to guide donor management of all patients after death was declared and authorization was obtained for donation. The CCTF had several meetings with abdominal and thoracic transplant surgeons to determine exactly what makes an organ acceptable for transplantation and what contraindications may lead a surgeon to refuse an organ. This resulted in an established trust between MTN donor service area (DSA), transplant surgeons, and the CCTF to allow them the ability to do what was needed to maximize organ function and suitability. In addition, collaboration stretched across DSA boundaries to programs outside the MTN area, particularly with pulmonologists and lung transplant surgeons in order to ensure their input and strategies were considered. Donors included in the analysis were declared deceased according to neurological criteria by the primary treatment team and were cared for by organ procurement coordinators (OPC) after authorization was obtained for organ donation. Authorization was obtained either via the first-person authorization state registry or authorization by the donors’ legal next of kin. Donation after circulatory death (DCD) was excluded from the study analysis, as intensivist management by the OPO does not occur prior to pronouncement of death. After authorization was obtained, an initial phone consultation was made to the intensivist on call by the OPC assigned to care for the donor at the bedside. The intensivist was provided a standardized report regarding the current medical condition of the donor, as well as pertinent medical history. An evidenced-based treatment plan was developed with the OPC to improve and maximize organ function. Regular communication between the OPC and the intensivist occurred throughout the donor case to ensure progress was being made or to determine if changes in the plan needed to occur. Throughout the medical management phase, the OPC utilized agreed upon donor management guidelines prescribed for fluids, vasopressors, blood products, ventilator strategies, electrolytes, hormonal therapy, and infection. A standardized list of donor management goals (DMGs) (Table 3), was developed, and the goal was to hit these targets within twelve hours of authorization. These DMGs included a Mean Arterial Pressure (MAP) of > 60mmHg, a Cardiac Index (CI) > 2.5L/min/m2, Urine Output of 0.5-3cc/kg/hr, pH of 7.30-7.45, and a P/F Ratio of >300 if the donor is over 60 years old and >350 if the donor is less than 60 years old. Our analysis was broken down into two groups; donors before intensivist management (IM) (prior to 2006) and after intensivist management (IM) (from 2006 and onwards). Primary outcome measures included: number of organs procured and transplanted per donor, percent of organs donated, and transplant outcomes. Secondary outcome measures included donor demographics, transplant yield calculation, and individual organ types. Data from January 2003 to December 2005 was included in the group prior to IM. Data prior to 2003 was deemed unable to be analyzed given lack of information available. 2003 marked a period of time where robust measures were taken to focus on data collection and accuracy and thus marked the beginning of this study. Data from January 2006 to October 2018 was included in the group after IM. In order to correct for data inflation in years between the two groups, a comparison was done as average per year and individually compared across each time period. To further ensure data was not due to differences between intensivists, but rather actually due to management strategies employed by the OPO, we investigated the average number of hours spent per intensivist per year from 2016 to 2020 (only years this data was available). The expected versus observed values for organ yield were calculated utilizing an OPO yield calculator developed by the Scientific Registry for Transplant Recipients (SRTR). De-identified data was analyzed statistically using ANOVA, Chi-Squared, Fisher-Exact and 2 sample t-tests. P-values less than 0.05 were considered statistically significant. A statistician assisted with data analysis.
Table 1
Table 1: Progression of Strategies for Organ Donor Management with Death by Neurological Criteria
Table 2
Table 2: Baseline Characteristics of Patients
Table 3
Table 3: Standard List of Donor Management Goals
Figure 1
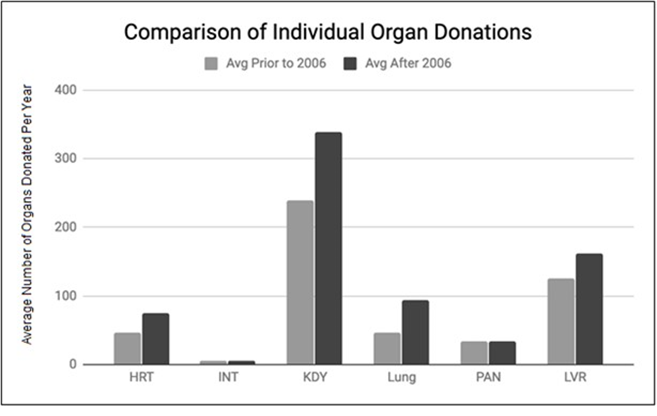
Figure 1: Histogram of Number of Organ Donations for Intensivist versus Traditional Management
Results
A total of 3,568 donors were included in the analysis; 550 donors prior to 2006 (before IM) and 3018 donors after 2006 (post-IM). Donor demographics are demonstrated in Table 2. Donor gender and race remained homogenous between the two groups. Donor age was significantly higher post-IM (35.83 ±18.79 (prior) vs. 38.89 ± 22.86 (post), p-value=0.0007). The causes of death changed significantly, with a notable increase in anoxia as a cause post-IM (Table 2). The number of organs transplanted significantly increased after IM for all organs except the intestine and pancreas, as seen in Figure 1. The total number of donors per year increased by 28% (p-value=0.026), while the total number of organs transplanted per year increased by 38% (p-value=0.009) following IM. The number of organs transplanted per donor increased significantly after IM (2.76 ± 1.82 vs 2.94 ± 1.89, p value=0.038). The average hours spent per intensivist per year from 2016 to 2020 was 1.26. The expected value for organs transplanted was 5295 and the observed value with IM was 5893 The observed/expected value is 1.12.
Discussion
Our data suggests that intensivist management of organ donors with death by neurological criteria may lead to an increase in donors and organs available for transplantation. We suspect that due to the small sample size, changes in pancreas and intestine organ transplants were not statistically significant. Pancreas and Intestine transplants are performed less frequently compared to other organ types. This could be due to the overall fewer number of pancreas and intestine programs. The increase in donor age post-IM may reflect improved conditioning of previously marginal organs by intensivists and liberation of criteria by transplant centers of such organs. The number of organs transplanted per donor increased significantly, from 2.76 to 2.94 after the implementation of IM. The observed versus expected value shows a 12% increase indicating that 12% more organs were transplanted than expected. This may further be evidence that management strategies employed may have contributed to the increase seen. Our team further statistically discerned whether each intensivist differed in outcomes by measuring average number of hours spent per intensivist with available data from 2016 to 2020. Our data showed consistently equal hours spent by each intensivist which equaled roughly 1.26 hours on average for each case by each clinician. This may indicate that strategies among intensivists did not skew as much from one another. This study is retrospective in nature and includes several consecutive management strategies implemented by the CCTF. It does not pinpoint specific contributing factors of intensivist-directed care to increased organ donation numbers. Contributions may include improved medical management of complex and critically ill patients by critical care-trained doctors, better communication between intensivists and the OPO staff, as well as the increase in registered donors in the MTN service areas. There are no nationally established guidelines for the medical management of organ donors, however, the MTN CCTF, now a fully executed Critical Care Committee of the MTN Advisory Board, utilized their expertise in collaboration with MTN clinical experts and transplant programs to set up a standardized set of guidelines in caring for organ donors with death by neurological criteria. As strategies evolved, they were able to be implemented in the standard MTN donor management guidelines. Donor management was then largely directed by protocols established between the OPO and the CCTF. One potential confounding factor in our study is the inability to discern exactly when certain changes in donor management were implemented that ultimately may have impacted outcomes. However, these changes were made at the direction of the CCTF. MTN’s results are similar to the findings of Singbartl et al., who also noted a significant overall increase in transplanted organs when dedicated intensivists were added to an organ donor support team. They observed an increase in available organs for transplantation of 13% one year after adding an intensivist, as well as an increase in the number of organs transplanted per donor. In their study, lung transplantations showed a nearly 2.5-fold increase in donation compared to the year prior. Though our results show a smaller 1.94-fold increase, intensivists appear to have a large impact on the number of organs available for transplantation. Potential shortcomings of our study include that this is a retrospective study analyzing three years prior to IM in comparison with 13 years after IM. Due to the design of the study being a retrospective review of longitudinal quality improvement data, there was no adjusting or “washout” period. Ideally, we would have liked an adjustment period for study purposes, however, due to changing practices, a switch in evidence-based practices simply took place instead in donor care. Given the nature of OPO care, staff was trained prior to initiation date of any new protocols to ensure 100% compliance was maintained with new practice therefore eliminating the need for an adjustment period. Regarding study analysis, we were unable to employ a proper difference-on-difference comparison with other facilities. While a difference-on-difference design would be ideal, it is nearly impossible to find a direct control group. To appropriately examine if the intensivists were solely responsible for the increase, the OPO would have to independently implement critical care management strategies without utilizing intensivists. Since this design was not feasible, we instead used our own OPO, prior to the addition of intensivists, to establish a baseline. The Organ Donation and Transplantation Breakthrough Collaborative increased best practices among donor hospitals, OPOs and transplant centers. In addition, the donor designation rates are increasing in this country with the focus on promotion and education to the community about the importance of donation. According to the most up to date data calculated by MTN, 81% of adults in Missouri and 78% of adults in Kansas are registered in their respective state’s first-person donor registries, which could also contribute to the increased number of donors.
Conclusions
It is important to increase donor and organ availability to close a growing gap between transplant organ demand and supply. Based on this study, intensivist oversight may be beneficial for optimal donor management. The next step in validating and further exploring the implications of this study is a randomized multicenter controlled trial comparing intensivist to traditional OPO management of the organ donor population. It would also be important to elucidate the specific factors of intensivist-directed donor management that specifically leads to increased organ availability in order to replicate those findings and further develop tools that will optimize organ donor care, which in turn will save more lives.
References
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008; 61: 344-349.
- DuBose J, Salim A. Aggressive organ donor management protocol. J Intensive Care Med. 2008; 23: 367-375.
- Singbartl K, Murugan R, Kaynar AM, Crippen DW, Tisherman SA, Shutterly K, et al. Intensivist-led management of brain-dead donors is associated with an increase in organ recovery for transplantation. Am J Transplant. 2011; 11: 1517-1521.
- Wojda TR, Stawicki SP, Yandle KP, Bleil M, Axelband J, Wilde-Onia R, et al. Keys to successful organ procurement: An experience-based review of clinical practices at a high-performing health-care organization. Int J Crit Illn Inj Sci. 2017; 7: 91-100.
- Salim A, Martin M, Brown C, Rhee P, Demetriades D, Belzberg H. The effect of a protocol of aggressive donor management: Implications for the national organ donor shortage. J Trauma. 2006; 61: 429-433;
- Mascia L, Mastromauro I, Viberti S, Vincenzi M, Zanello M. Management to optimize organ procurement in brain dead donors. Minerva Anestesiol. 2009; 75: 125-133.
- Rosendale JD, Kauffman HM, McBride MA, Chabalewski FL, Zaroff JG, Garrity ER, et al. Hormonal resuscitation yields more transplanted hearts, with improved early function. Transplantation. 2003; 75: 1336-1341.
- Wheeldon DR, Potter CD, Oduro A, Wallwork J, Large SR. Transforming the "unacceptable" donor: outcomes from the adoption of a standardized donor management technique. J Heart Lung Transplant. 1995; 14: 734-742.
- Health Resources & Services Administration. Organ Donation Statistics. 2019.
- Mendez MA, Fesmire AJ, Johnson SS, Neel DR, Markham LE, Olson JC, et al. A 360° Rotational Positioning Protocol of Organ Donors May Increase Lungs Available for Transplantation. Crit Care Med. 2019; 47: 1058-1064.








































































































































