Intramedullary Epidermoid Cyst and Tethered Cord
- 1. Department of Neurosurgery, BG clinics Bergmannstrost Hall, Germany
ABSTRACT
A Case report about an intramedullary epidermoid cyst and its association with an arrested ascent of the spinal cord, concomitant the neurological deficits, the surgical treatment and the clinical progress after one year. Epidermoid cysts are rare in the spinal cord, less than 1% of all spinal tumors. A 40-year-old woman described hypesthesia in the right left foot and back pain since one year. The MRI provided the evidence of an intramedullary epidermoid cyst at the level of L1/2 and revealed an arrested ascent of the cord opposite vertebra L3. With total compression of the spinal cord so we decided to operate on her. Intraoperative the intramedullary tumor proved to be an epidermoid cyst with typical pearly appearance and the presence of hair. The surgical removal including capsule was uncomplicated done under neurophysiological monitoring. The hypoesthesia was obviously regressive in the following postoperative days, as well as severe back pain. The MRI after 12 months revealed a fractional cystic alteration. The patient maintained no complaints up to lightly hypesthesia in the right foot. The total resection of epidermoid cyst to avoid recurrence is the main treatment. Neurophysiological monitoring is mandatory.
KEYWORDS
• Epidermoid cyst
• Intramedullary lesion
• Magnetic resonance image
• Arrested ascent of spinal cord
• Neurophysiological monitoring
CITATION
Tews J, Sanchin L, Meisel HJ, Hohaus C (2016) Intramedullary Epidermoid Cyst and Tethered Cord. J Surg Transplant Sci 4(6): 1043.
ABBREVIATIONS
MRI: Magnetic Resonance Image
INTRODUCTION
The epidermoid cyst is a rare tumor in the spinal canal, less than 1% of all spinal tumors [1]. It was firstly described by Hans von Chiari in 1883. The pearly tumor is typically located intradural and extra medullar. Intra medullary localization is very rarely. Only 60 cases are published [2-4]. Epidermoid cysts can be congenital or acquired (e.g., after lumbar puncture or meningocele repairs) [5]. Principal therapy is surgical removal. Achieving curative treatment the tumor must be removed completely [6].
CASE PRESENTATION
A 40-year-old woman presented with back pain and numbness in her right foot since one year. A bowel and bladder dysfunction werenot named. On physical examination there was a hypesthesia of the left lower leg and foot. The motoric function was completely retained. Indeed there was a difference in the proprioceptive reflex of her legs and a positive Babinski sign. The left side showed hypoactive reflexes, but not pathological. There were no lumbar punctures or spinal anesthesia in patient’s history.
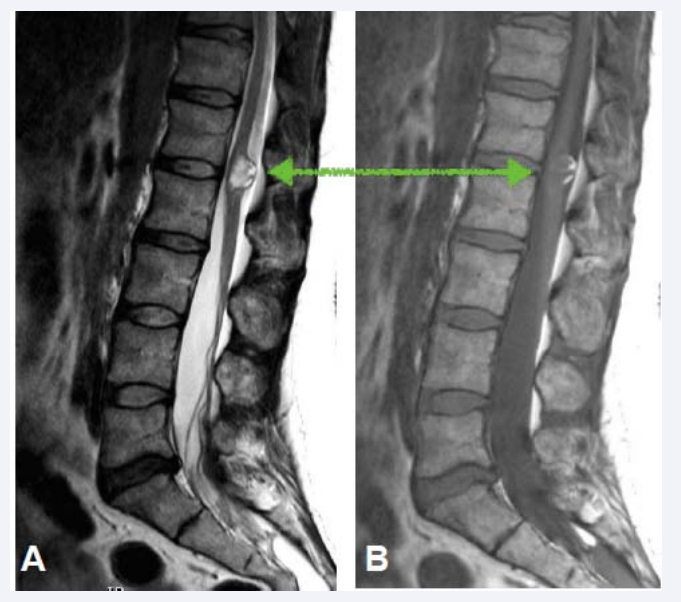
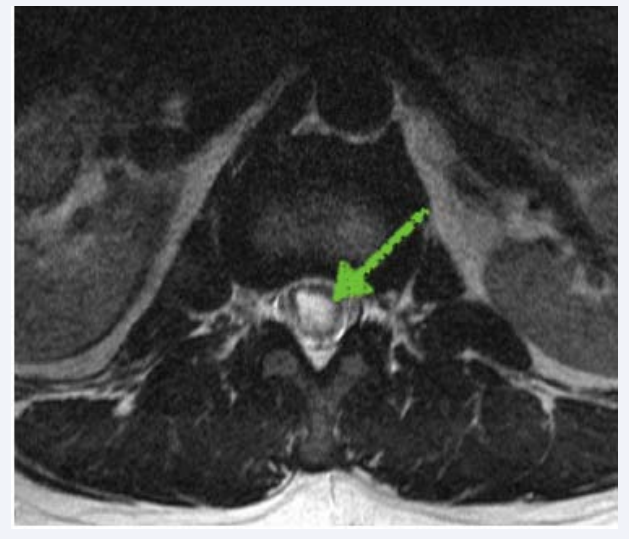
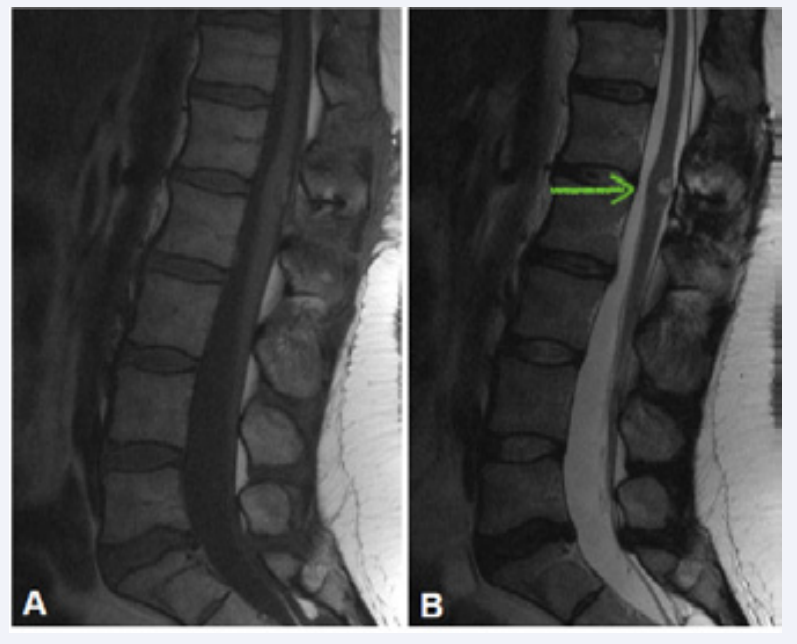
The magnetic resonance imaging (MRI) of lumbar spine revealed an intra medullary tumor at the vertebral level L1/L2 with a distinct shift of Conus medullaris. It was hyperintense on T2-weighted images and mixed iso- and hyperintense on T1- weighted images (Figure 1, 2).
Figure 1: Sagittal MRI of lumbar spine demonstrating intramedullary epidermoid cyst (green arrow) at the vertebral level L1/L2 with arrested ascent of the spinal cord. In T2-weighted image (A) it is hyperintense and in (B) T1-weighted image it is mixed iso- and hyperintense.
Figure 2: Spinal MRI axial demonstrating epidermoid cyst (green arrow) hyper-intense in T2- weighted imaging.
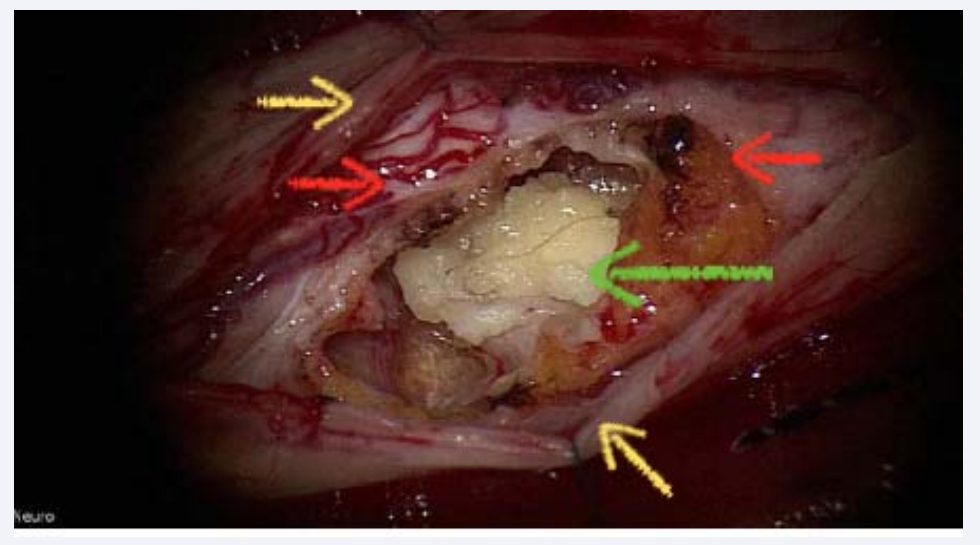
The patient underwent surgery under general anesthesia and neuro physiological monitoring. We performed a laminoplastia from L1 to L2. After opening the dura the tumor was identifiable.
After finding tumor edges we started preparation in the depth. At first a bright yellow gelatinous mass came into sight. This was pulled out and was send to histopathological examination. Afterwards some hair even appeared (Figure 3).
Figure 3: Intraoperative image - after opening the dura (yellow arrow) and the spinal cord (red arrow) and preparation in the depth a bright yellow gelatinous tumor appeared with hair (green arrow).
A complete microsurgical resection of the tumor was achievable. During operation electrophysiological signals were in normal range.
The results of the histopathological examination confirmed our suspicion of an epidermoid cyst. During the hospitalization the patient described a decrease of numbness. No motoric deficits or dysfunction of bowel and bladder were detectable.
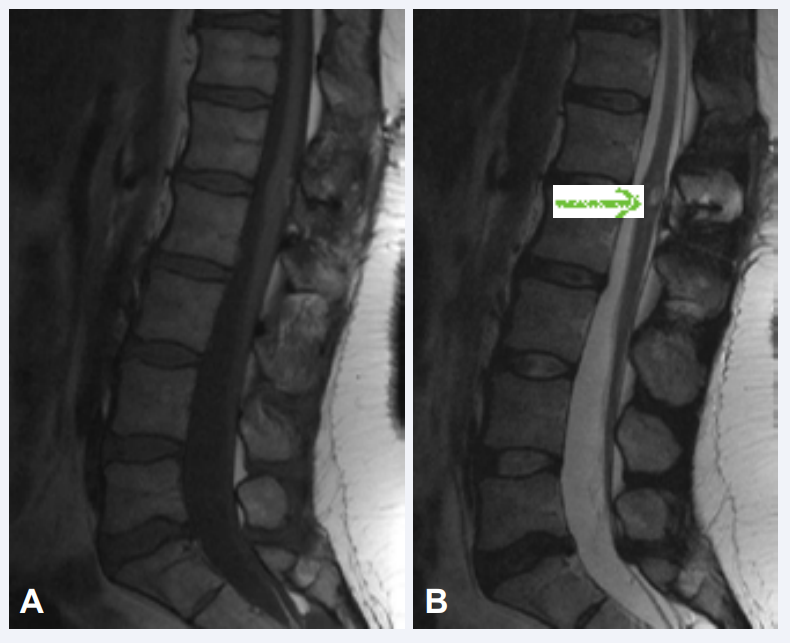
We started follow-up examinations and MRI-controls after three and twelve months. The patient still described the slightly numbness and occasional back pain. The MRI revealed a small cyst in the former operational area without progression or alteration (Figure 4, 5).
Figure 4: Sagittal MRI of lumbar spine 3 months after surgery. (A) T1- and (B) T2-weighted Figure imaging demonstrating a small cyst (green arrow) in the former operational area. The patient described a slightly numbness in her right foot and occasional back pain.
Figure 5: Spine MRI sagittal - 12 months after surgery. (A) T1- and (B) T2-weighted imaging demonstrating no progression or alteration of the small cyst (green arrow).
Abbreviations: MRI: Magnetic Resonance Imaging
DISCUSSION
The patient had only a minor manifestation of symptoms. She was young and without any lumbar puncture in history. The MRI shows a spinal abnormality, namely arrest ascent of the spinal cord. Congenital epidermoid cysts are mostly associated with other abnormalities, for example dermal sinus or hemivertebrae [4,7]. For that reason we assumed that the epidermoid cyst in our case is congenital.
MRI is the first and important diagnostic tool finding the organic reason of patients neurological deficits [4,8]. In the ast twenty years the MRI made great progress in diagnosis of intramedullary tumors. The intensity of signals is different between various phases. So Epidermoid cysts usually appear hyperintense on T2-weighted images and hypointense on T1- weighted images. One cyst can have different signal intensity because of the various lipid and protein contents. In our case the epidermoid cyst appeared hyperintense on T2 and mixed iso- and hyperintense on T1. Other important criterions are no parenchymal surrounding edema, distinct tumor limits and calcification. Except for calcification our case fulfilled the stated criteria of Vion-Dury et al. [4,9].
Epidermoid cysts are benign. However the location in the spinal cord is the proper therapeutic challenge. Mainstay of therapy is the excision of the tumor and its capsule [2,3,10]. Our aim was a complete resection without causing any further neurological deficit.
We operated with assistance of neurophysiological monitoring, which shows intraoperative a normal signal without loss of signals. In macroscopic assessment the excision was successful.
Schaller declared that tumor entity or rather the tumors WHO-Classification, its location in the spinal cord, patients age and duration of symptoms before surgery are important for the postoperative neurological outcome in spinal tumor surgery [11]. These are major facts but intraoperative neurophysiological monitoring is an important and mandatory tool to reduce preoperative morbidity. Our patient did not have any motoric or new sensory deficit, no bladder or bowel dysfunction. Our follow up examinations and MRI-controls were satisfying. Until now we have no long-term results to be confident that the woman is without recurrence.