A comprehensive Case Report on Buschke-Lowenstein Tumor
- 1. Department of Urology B, Mohamed V University, Rabat, Morocco
- 2. Department of Dermatology, Mohamed V University, Rabat, Morocco
- 3. Department of Anatomopathology, Mohamed V University, Rabat, Morocco
Abstract
Buschke Lowenstein tumor (BLT) or giant condyloma acuminatum (GCA) is a sexually transmitted disease, of viral origin, essentially due to the human papillomavirus.
BLT is relatively common in males and occurs in 81-94% of cases in the penis and in 10-17% of cases in the anorectal region. Risk factors include poor hygiene, immunosuppression, smoking and STIs.
It is characterized by a more or less ulcerated budding lesion of the genital or perianal region, and the evolution is slow and can be associated with several complications including superinfection, fistulization to neighboring organs, necrosis, or hemorrhage.
A wide radical excision, followed by reconstructive surgery, seems to be the optimal therapeutic strategy for BLT management, however other treatments have been proposed in order to try to reduce the tumor and to limit surgical damage.
Keywords
• Buschke Lowenstein
• Condyloma
• Genital tumor
• Case repor
CITATION
Zineeddine O, Salim AL, Slaoui A, Eid CM, Derqaoui S, et al. (2024) A comprehensive Case Report on Buschke-Lowenstein Tumor. J Urol Res 11(2): 1151.
INTRODUCTION
Buschke Lowenstein tumor (BLT) or giant condyloma acuminatum (GCA) is a rare sexually transmitted disease, of viral origin, essentially due to the human papillomavirus, most often type 6 and or 11 and exceptionally type 16 and 18 [1]. This epithelial tumor has still poorly defined relationships with verrucous carcinoma, the histological aspect is benign, although its clinical aspect rather suggests the opposite. It affects men in particular and is characterized mainly by its deep extension, its degenerative potential and its recurrent character after treatment. Surgery is the treatment of choice [2].
CASE PRESENTATION
Mr M.S, 54 years old, married, with a history of depressive syndrome, without any notion of homosexuality or multiple partners, who consulted for a budding pubo?scrotal mass. The onset of the symptomatology dated back to 1 year with the progressive installation of a budding scrotal tumor causing tingling.
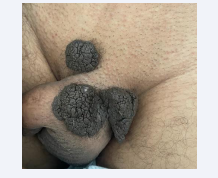
The physical examination found a cauliflower?like tumor with budding and vegetative lesions located on the pubis, the root of the penis, and the left scrotum [Figures 1,2].
Figure 1: Showing the operative view of BLT
Figure 2: Showing the anterior view of BLT.
The rest of the examination, i.e. the digital rectal examination and palpation of the lymph nodes, is within normal limits. The sexually transmitted infection tests (TPHA, VDRL, HIV, HVB, HVC) were negative.
Total removal of the tumor was performed [Figure 3]. The tumor was covered by the surrounding skin.
Figure 3: BLT after removal.
The study of the excision specimen showed 3 pieces of 2 cm for the smallest and 8 cm of long axis for the largest.
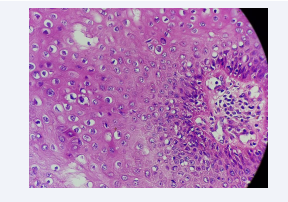
Anatomopathological study revealed a polyploid lesion lined by an ortho-keratotic hyperkeratosis. Koilocytes were found in the superficial layers of the epidermis [Figure 4].
Figure 4: Morphological aspect at high magnification showing koilocytes.
Concluding to a Buschke Lowenstein tumor.
The postoperative course was simple.
DISCUSSION
Nosology
Buschke?Löwenstein tumor or giant condyloma acuminatum is a pseudoepitheliomatous proliferation belonging to the group of verrucous carcinomas. The first description of giant condyloma acuminatum dates back to 1896. It was in 1925 that Buschke and Löwenstein made it a characterized entity [3]. It is distinguished from condyloma acuminatum by its more marked proliferation and deep penetration into the underlying tissues and from squamous cell carcinoma by the absence of histological invasion (respect of the basement membrane) and of metastasis. Human papillomavirus (HPV) 6 or 11 infection is frequently associated, although a few cases of HPV 16 or 18 infection have been described. These HPV 6 and 11 are low?risk oncogenic viruses, usually present in benign condyloma acuminatum but not in malignant lesions [4].
Epidemiology BLT is a rare tumor whose frequency is currently estimated at 0.1% of the general population. We do not have a prevalence in the Moroccan population probably because patients are recruited in different hospital services (urology, gastroenterology, dermatology, gynecology, infectious diseases).
Giant condyloma occurs at all ages with an average of 45 years. BLT is relatively common in males (77%). In men, BLT occurs in 81?94% of cases in the penis and in 10?17% of cases in the anorectal region. Risk factors include poor hygiene, immunosuppression, smoking and STIs [5].
The global incidence of HPV infection is rising, among young and sexually active individuals; as a result, in recent years these infections have also become increasingly conspicuous in urology practice, both as incidental fndings and primary complaints [6].
Clinic
Clinically, BLT often begins as small filiform or rounded lesions. In the state phase, it is characterized by a more or less ulcerated budding lesion of the genital or perianal region. In men, the tumor is most often located in the balanopreputial region, beginning as a condyloma and progressively extending to the glans, prepuce and sheath of the penis. In women, the most frequent location is vulvar, sometimes extending to the perianal area. A large, irregular, budding, cauliflower?like tumor that may exceed 10 cm in long axis may be seen, often with superficial ulcerations and superadded infectious lesions [7].
The presence of bleeding, infiltration of the base, or adenopathy should raise suspicion of malignant degeneration. Biopsy of the lesion allows histological confirmation and to look for sign of degeneration.
The main differential diagnoses include Bowen’s disease (its dyskeratotic condylomatous form), squamous cell carcinoma, as well as keratotic pseudoepitheliomatous balanitis [8].
Depending on the location, the evaluation may include, in addition to palpation of the lymph nodes, rectoscopy, gynecological examination, pelvic CT scan or nuclear magnetic resonance.
Recent meta-analysis and case-control studies demonstrated a significant relationship between the presence of HPV DNA and urothelial carcinoma of the bladder (UCB) [9].
Histology
It is a perfectly limited squamous tumor characterized by epithelial hyperplasia, sometimes pseudoepitheliomatous, hyperacanthosis, hyperpapillomatosis and koilocytes which are pathognomonic markers of HPV infection, however their presence is not constant. The basement membrane remains intact as evidence of the benignity of the tumor despite its malignant behavior. Careful histological examination is crucial to exclude transformation to SCC [10].
Evolution and prognosis
The evolution is slow and can be associated with several complications including superinfection, fistulization to neighboring organs, necrosis, or hemorrhage. Malignant transformation is one of the evolutionary risks. It has been reported in 30% to 56% of cases [11].
Treatment
A wide radical excision, followed by reconstructive surgery, seems to be the optimal therapeutic strategy for BLT management; it must be early and as extensive as possible to avoid tumor recurrence which is very frequent. The interventions are often mutilating. The completeness of the surgical removal of TBL must be confirmed by anatomopathological examination of the surgical specimen. If the surgical excision is incomplete, revision surgery is indicated. For tumors localized in the glans, the classic procedure consists of a partial penectomy with a safety margin of 2 cm, or even a total penectomy if the tumor is more extensive. Some authors propose a more limited procedure that appears to be satisfactory from a carcinological point of view and achieves a satisfactory aesthetic and functional result.
Other treatments have been proposed in order to try to reduce the tumor and to limit surgical damage: podophyllin and 5?fluorouracil, systemic bleomycin associated with cisplatin and methotrexate, with poor results. Cryotherapy and laser destruction are often insufficient and do not allow histological examination of the excisional part. However, the CO2 laser has the advantage of allowing hemostasis and immediate sterilization of the wound, with better healing than with traditional surgical techniques. The use of radiotherapy is controversial. It is used preoperatively to reduce the tumour mass, or as a last resort for non?operable tumours [12].
CONCLUSION
Buschke?Lowenstein tumor is a rare tumor that requires early and extensive surgical treatment with regular post?surgical, clinical and histological surveillance. The functional and vital prognosis can be engaged, hence the interest of STI prevention by protected intercourse and sexual education of young people.
REFERENCES
2. El Amrani F, Hassam B. Buschke-Löwenstein tumor. Pan Afr Med J. 2013; 14: 94.
5. Mzyiene M, Ziba J, Ahsaini M, Mellas S, El Ammari J, Tazi M, et al. Étude descriptive des tumeurs génitales Buschke-Lowenstein. Progrès en Urologie. 2021; 31: 857-858.