Anastomotic Renal Sinus Haemangioma - A Case Report
- 1. Radiology Residency Program – University of Salerno, Italy
- 2. Radiology Unit, Azienda Ospedaliera Universitaria San Giovanni di Dio e Ruggi d’Aragona, Italy
- 3. Centro Radiologico Verrengia, Italy
- 4. Urology Unit, Azienda Ospedaliera Universitaria San Giovanni di Dio e Ruggi d’Aragona, Italy
- 5. Department of Medicine and Surgery, University of Salerno, Italy
Abstract
Background: Vascular tumours of the kidney are a heterogeneous group of lesions showing common characteristics with malignant neoplasms, making it significantly challenging the pre-operative diagnosis. Among these lesions, anastomotic hemangioma (AH) is a recently recognised variant of hemangioma of the genito-urinary tract characterized by a complex vascular structure.
Methods: We present the case of an 85-year-old patient with an incidental diagnosis of renal mass with no laboratory abnormalities. We performed radiological examinations (CT and MRI) that revealed a lesion with apparently malignant characteristics. The multidisciplinary team decided to proceed with nephrectomy.
Results: The subsequent histological result was benign, highlighting the uncertainty surrounding the preoperative evaluation of renal tumours.
Conclusion: This case highlights the importance of evaluation and multidisciplinary approach in the management of renal masses, particularly for rare lesions such as AH. Knowledge of these pathological entities is crucial for clinicians to avoid misdiagnosis and inappropriate treatment and to improve the quality of care in patients with renal tumours. Increasing awareness of these variants may also influence improvement in imaging strategies and diagnostic guidelines, promoting a more conservative approach in the presence of suspicious, but potentially benign, lesions.
Keywords: Anastomotic Hemangioma; Kidney; Ct scan; MRI; Radiology; Diagnosis
Introduction
Vascular tumours are a very small group of renal neoplasms with a mesenchymal origin [1,2]. In this category of tumor, the most frequent is the haemangioma which occurs frequently in the skin and subcutaneous tissues, whereas visceral forms are rare and are mainly found in the liver. Histologically, haemangiomas are generally classified into two main types: cavernous and capillary [3]. Montgomery and Epstein [4], firstly identified a particular variant of renal capillary haemangiomas, which had intermediate features of the sinusoidal and the hobnail hemangioma, which usually occurs in the skin and soft tissues. This neoplasm was named Anastomotic Hemangioma (AH) because of its peculiar histological structure showing anastomotic sinusoidal capillary vessels similar to splenic sinusoids. Although AH is considered characteristic of the genitourinary system, with a specific predilection for the kidneys, it has also been reported in other sites, including muscle, skin, adrenal gland, liver and gastrointestinal tract [2,5]. The similarity of AH with other vascular neoplasms is a crucial aspect to consider potentially leading to misdiagnosis and overtreatment. Indeed, the differential diagnosis of AH of the kidney mainly includes malignant vascular tumours such as angiosarcoma, intravascular papillary endothelial hyperplasia (PEH), Kaposi's sarcoma and angiomyolipoma [6]. The most frequent malignant neoplasm showing similarities with AH is angiosarcoma, occurring most frequently between the sixth and seventh decade of life [7]. this tumour has a strong tendency to early metastasize, mainly involving liver, lungs and bones. This tumour often shows an anastomising vascular pattern, hobnail endothelial cells and immunopositivity to endothelial cell markers, features similar to those of AH. In addition, the high cellularity and entrapment of renal tubules could be misinterpreted. Since it is a malignant neoplasm, angiosarcoma requires an early and radical approach. Thus, an inadequate management of an AH, misdiagnosed as an angiosarcoma, can lead to unnecessary aggressive treatment and psychological stress for the patient. Renal AH presents a distribution over a wide age range and a predilection for the male sex. Clinically, the manifestations are variable and mostly insignificant; occasionally haematuria or flank pain have been reported [5], which are common symptoms in the presence of malignant lesions. Overall, AH is usually incidentally detected by radiographic investigations performed for other unrelated reasons [5]. In the evaluation of masses in the genitourinary tract, Computed Tomography (CT) imaging, possibly supported by magnetic resonance imaging (MRI), plays a crucial role. CT images with and without Contrast Medium (CM) can provide valuable information on the vascularisation and architecture of the lesion. Thus, it is important to analyse how the AH presents radiologically, as the radiological features may be useful to guide the differential diagnosis. Considering difficulties in differentiating malignant lesions with respect to AH, the aim of our study is to report the behaviour of AH of the renal sinus. Particularly, in the case we detail the radiological features, histological findings and relevant clinical information., in order to supplement the information already available to improve the pre-operative diagnosis.
Case Description
We report a case of an AH originating in the left kidney of an 85-year-old Caucasian man with a history of stage IIIB chronic renal disease, hypertension and mixed dyslipidaemia. The patient was incidentally diagnosed with a left renal mass during an ultrasound examination of the abdomen performed for an elevation of transaminases, in the absence of significant genito-urinary symptoms.
CT Imaging
Following this finding, he underwent CT investigation without and with intravenous CM (Figure 1).
An axial CT scan showed an expansive formation with oval morphology in the left renal sinus outlining the organ with dimensions of about 32 x 30 mm, which tended to grow in the connective tissue of the renal sinus, slightly dislocating the inferior calyx group.
In non-enhanced acquisition (Figure 1.1), this formation presented a heterogeneous appearance with average values of HU of 19-20 HU, with negative values with adipose significance in some places, and peripheral areas values of 37-60 HU.
In the arterial phase scans (Figure 1.2), the periphery of the lesion showed a clearly annular and pseudonodular enhancement with a tendency to centripetal filling and densitometric values reaching 230 HU, thus demonstrating a highly representation of vascular tissue component.
In the venous phase (Figure 1.3), the lesion showed a tendency to homogeneous filling with average values up to 130 HU. The lesion showed homogeneously persistent enhancement in late scans (Figure 1.4), with HU values between 50 and 70.
Neither calico-pyelic dilatation was evident nor significant lymphadenopathy in the mesenteric, para-aortic and retroperitoneal stations.
RM Imaging
To better characterize the lesion, the patient underwent MRI examination of the upper and lower abdomen without and with intravenous CM (Figure 2).
MRI images showed T1-dependent signal hypointensity (Figure 2.1), inhomogeneous T2-dependent signal hyperintensity (Figure 2.3), and appears to have poor diffusion-weighted signal restriction (Figure 2.4, Figure 2.5). Overall, it is characterised by inhomogeneous contrast impregnation and has a greater axis of 32 x 23 x 26 mm (LL x AP x CC).
This technique confirms that the heteroformation did not generate compressive effects on the renal pelvis or vascular invasion. No significant mesenteric, para-aortic or retroperitoneal lymphadenopathy was evident.
Therapeutic Decision
Considering the patient's clinical profile and given the localised nature of the lesion, with no extra-organic extension but located in the surgical risky region of the renal sinus, the decision of the multidisciplinary oncological group was to propose radical nephrectomy to the patient.
Histological Results
Figure 3 describes the macroscopical and microscopical characteristics of the operatic specimen.
Macroscopically, the nodule of 3.5×2.5x2.5 cm was located at the renal sinus. It resulted to be circumscribed but without a recognizable capsule and with a translucent red cut surface, which was extensively sampled (Figure 3.1).
The described sinus nodule had the histological features of AH. The epicentre of the lesion was in the renal sinus and microscopic contiguity with the apex of a renal pyramid is observed (Figure 3.2, Figure 3.3, Figure 3.4).
Immunohistochemical Results
Immunohistochemistry of the nephrectomy specimen confirmed positivity for CD34 and CD31. Immunostains for smooth muscle antibody and CD34 highlighted the orderly vasoformative architecture of this lesion. Positivity CD31 confirmed the presence of endothelial cells in immunohistological tissue sections.
Figure 1
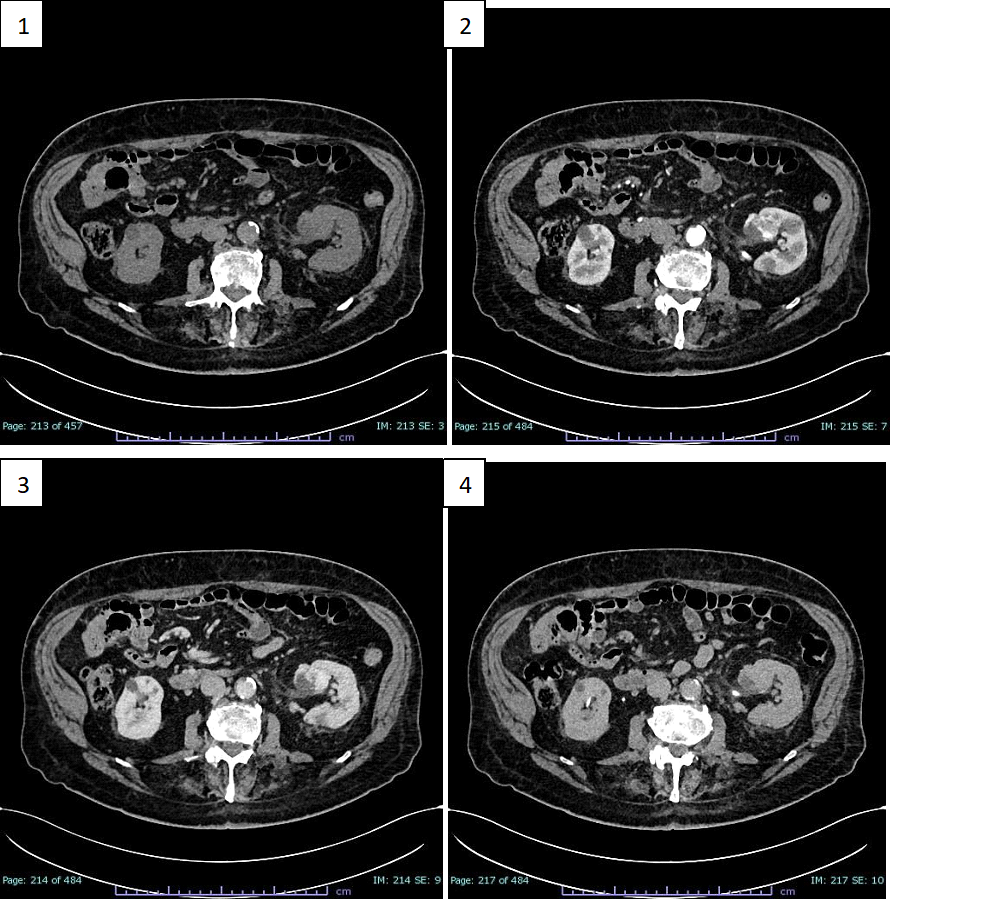
Figure 1: CT scans before and after enhancing with CM. 1) Non enhanced axial CT scan: a
hypodense expansive formation is seen in left renal sinus (32 x 30 mm). 2) Axial CT with CM early arterial phase: the formation shows peripheral annular and pseudonodular enhancement. 3) Axial CT with CM venous phase: the formation shows tendency to homogeneous filling. 4) Axial CT whit CM late phase: the formation shows homogeneously persistent enhancement.
Figure 2
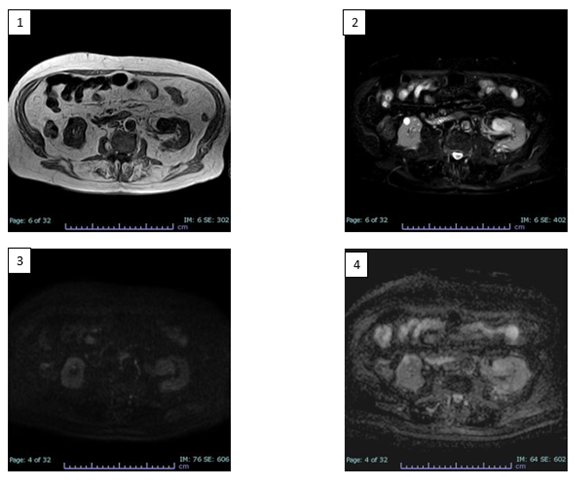
Figure 2: RM scans before and after enhancing with CM. 1) Axial T1 TFE MRI sequence: heteroformation of the left renal sinus showing T1-dependent signal hypointensity. 2) Axial SPAIR T2 MRI sequence: inhomogeneous T2-dependent signal hyperintensity. 3) Axial DWI sB750 MRI sequence: poor diffusion-weighted signal restriction. 4) Axial ADC MRI sequence.
Figure 3
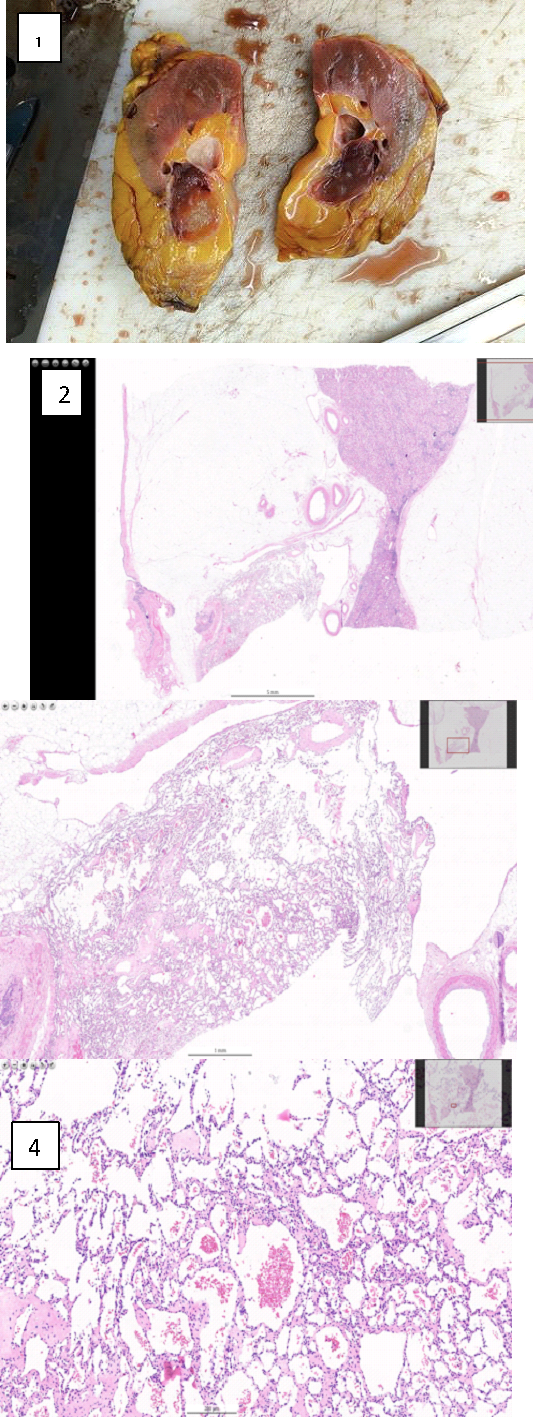
Figure 3: Macroscopical and microscopical findings. 1) Macroscopic appearance of the AH of the renal
sinus. 2) Magnification 10x. 3) Magnification 40x. 4) Magnification 200x.
Discussion
The imaging features reported in the case presentation show a tendency towards heterogeneity, indeed, both methods lean towards a pre-operative diagnosis of malignant lesions. At the CT scan without CM, an inhomogeneous hypointense lesion is evident in the left renal pelvis, at the level of the lower third, which shows uneven density in all its points, varying from punctiform areas with adipose-like densitometric coefficients (from -10 HU to -2 HU), to more frankly solid areas (49-20 HU) and to sections suggesting the presence of vascular components (37-60 HU). These findings are confirmed in subsequent scans enhanced with CM and, in particular, the lesion shows a frank enhancement in the more caudal peripheral portion in the arterial phase (up to 230 HU). In the subsequent portal phase a more homogeneous contrastographic filling of the entire lesion, with values of around 130 HU, was noted confirming the presence of an important hypervascular tissue component. However, the lesion shows no frank signs of invasiveness or compression of the surrounding structures, in the absence of dilation upstream and downstream of the lesion. Furthermore, there are no signs of necrosis or calcifications within the lesion. MRI images also show characteristics of inhomogeneous signal intensity, reflecting its vascular nature, revealing signal hypointensity in T1 sequences, inhomogeneous signal hyperintensity in T2 and poor signal restriction in DWI, indicative of poor cellularity. In line with the literature, our experience confirms the complexity of discriminating against the dyskaryokinetic nature of such a complex lesion with CT investigations, even if supplemented by MRI acquisitions. Thus, even if there are many overlapping features among the entities placed in benign vs. malignant differential diagnosis from the anatomopathological perspective, this diagnostic difficulty appears even more evident to the radiologist's eye. Indeed, it is not surprising that AH is still treated with demolitive approaches, such as total or partial nephrectomy, or more rarely local excision, with the aim of clarifying the nature of the lesion. However, in support of the biologically indolent nature of AH, some limited evidence exists on a small group of patients brought to follow-up which showed no tendency for recurrence or metastasis [3,9].
Conclusion
Predicting the nature of such a complex rare renal lesion prior to a direct assessment is still a complex process. There is a clear need for careful analysis and a multidisciplinary approach in the management of renal masses, especially for those of rare onset such as AH. In this setting, our work takes part of this complex process by reporting imaging behaviour of an AH in order to enhance the awareness in the framing of such lesions. This could also stimulate improved imaging strategies and diagnostic guidelines, favouring more conservative approaches in suspected and eventually benignant lesions by avoiding demolishing treatments.
Informed Consent Statement
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent form is available in his paper clinical medical record for review by the Editor-in-Chief of this journal.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Disclosure Statement
We would like to thank the entire team of the Urogenital Radiology section of “San Giovanni di Dio e Ruggi D’Aragona” Hospital, Salerno – Italy.
The case-report has been read and approved by all named authors.
Our case-report complies with the Declaration of Helsinki.
References
- Brown, Jeffrey G, Folpe Andrew L, Rao Priya, Lazar Alexander J, Paner Gladell P, Gupta Ruta, et al. Primary vascular tumors and tumor-like lesions of the kidney: a clinicopathological analysis of 25 cases. Am J Surgical Pathol luglio. 2010; 34: 942-949.
- Mehta V, Ananthanarayanan V, Antic T, Krausz T, Milner J, Venkataraman G, et al. Primary benign vascular tumors and tumorlike lesions of the kidney: a clinicopathologic analysis of 15 cases. Virchows Arch. 2012; 461: 669-676.
- Lin, Jingmei, Grande Jeremy, Ulbright Thomas, Montgomery Elizabeth. Emangioma anastomizzante del fegato e del tratto gastrointestinale: Una variante insolita che imita istologicamente l'angiosarcoma. Am J Surgical Pathol. 2013; 37: 1761-1765.
- Montgomery E, Epstein JI. Anastomosing hemangioma of the genitourinary tract: a lesion mimicking angiosarcoma. Am J Surg Pathol. 2009; 33: 1364-1369.
- Tao LL, Dai Y, Yin W, Chen J. A case report of a renal anastomosing hemangioma and a literature review: an unusual variant histologically mimicking angiosarcoma. Diagn Pathol. 2014; 9: 159.
- Omiyale AO. Anastomosing hemangioma of the kidney: a literature review of a rare morphological variant of hemangioma. Ann Transl Med. 2015; 3: 151.
- Leggio L, Addolorato G, Abenavoli L, Ferrulli A, D'Angelo C, Mirijello A, et al. Primary renal angiosarcoma: a rare malignancy. A case report and review of the literature. Urol Oncol. 2006; 24: 307-312.








































































































































