Correlation of Prostate Specific Antigen with Levels of Prolactin in Mexican Elderly with Prostate Cancer
- 1. Coordination of Investigation in Health IMSS, Mexico
- 2. Center for Educational Research and Teacher Training, Mexico
- 3. General Hospital Zone No. 2 IMSS, México, Mexico
- 4. Faculty of Medicine UASLP
- 5. Central Hospital Dr. Ignacio Morones Prieto, México
Abstract
Introduction: Prostate cancer is one of the most common cancer in men and increases with the aging. Having 87.6% of the deaths occurred in the population over 65 years of age. Nevertheless, many aspects remain unclear or controversial.
Materials and methods: Observational, analytical and transversal study. Men older than 60 years with prostate cancer diagnosed for the first time in the service of Urology in the General Hospital of Zone 50 SLP Mexico with a total sample of 50 patients, were it was taken the determination of FSH, LH, PSA and PRL. The statistical tests used with P ≥0.05were Mean, Standard Deviation, Analytical Student T and Pearson correlation.
Results: In our study population in patients with prostate cancer with a mean age of 72 years there were no differences in the levels of PSA, PRL, LH, FSH in both groups. However, we found a slightly greater difference in the over 80s. Which we believe is due to the physiopathology of the testicular deficiency.
Conclusion: Serum hormones determined in this study LH, FSH and PRL were not found to influence prostate specific antigen levels in elderly patients with prostate cancer, although PSA levels were not associated with prolactin levels. This finding allows you to know that there is no direct relationship of PRL and PSA.
Keywords
Prostate specific antigen; Prolactin; Elderly; Prostate cancer
Citation
Miguel Ángel MR, Lourdes MR, María Cleofás RA, Francisco Javier LE, Gonzalo GG, et al. (2018) Correlation of Prostate Specific Antigen with Levels of Prolactin in Mexican Elderly with Prostate Cancer. J Urol Res 5(1): 1098.
ABBREVIATIONS
FSH: Follicle Hormone; LH: Luteinizing Hormone; PSA: Prostate Specific Antigen; PRL: Prolactin; GH: Growth Hormone; PCa: Prostate Cancer
INTRODUCTION
Prostate cancer occupies the fourth place of all cancer diseases and is the second most common among men. Seventy percent of prostate cancer cases occur in men from developed countries.
The highest incidence rates occur in Austria and North America (111.6 and 97.2 cases per 100,000 men). While the lowest rates occur in Asian countries (4.5 to 10.5 cases per 100,000 men) [1]. The possible contribution of physical and chemical carcinogens associated with environmental pollution and negative lifestyle changes should not be forgotten either. The mortality rate for prostate cancer remains stable, with a slight decline in recent years [2]. In light of recent advances in genetics and molecular medicine, have been clarifying the mechanisms of sensitivity and resistance to anti-hormonal therapy and complex biological mechanisms of disease progression and metastasis, which have forced change attitudes and management approaches, both in diagnosis, evolution or progression to metastatic disease and even for preventive therapy [3].
Recent studies show an inverse relationship between testosterone levels and PCa. The usefulness of hormonal patterns in PCa diagnosis is controversial. Sex hormones, particularly androgens, have been implicated in prostate carcinogenesis. Overall, however, prospective studies have reported no association between circulating levels of sex hormones and the risk of prostate cancer. Yet there has so far been no conclusive evidence, despite 34 studies, that levels of circulating testosterone in individuals developing prostate cancer are higher than in controls [4-6].
GH can affect the growth and survival of prostate cancer cells, but the effect of GH on prostate cancer cell motility is unknown. In the present study, the potential for exogenous and autocrine GH to directly affect prostate cancer cell motility was addressed. Antagonists of hypothalamic growth hormone-releasing hormone (GHRH) inhibit growth of various malignancies, including androgen-dependent and independent prostate cancer, by suppressing diverse tumoral growth factors, especially GHRH itself, which acts as a potent autocrine/paracrine growth factor in many tumors [7,8].
Autocrine and/or paracrine prolactin may also contribute to the pathogenesis of prostate cancer; for example,prostatic hyperplasia is seen in mice that overexpress prolactin in the prostate, and these changes may progress to intraepithelial neoplasia and even to adenocarcinoma of the prostate [9].
The prostate is a hormone-dependent organ and the most important factors in its development, growth and differentiation are androgens and prolactin. The discovery of the new complex STAT-5-AR could be identified in patients with prostate cancer and create new lines of treatment in those patients who it results positive.
There is significant evidence of paracrine and autocrine action of Prolactin, showing expression of the same in 50% to 60% progression of prostate cancer hormone refractory and metastasis. This study provides strategies for therapeutic support based on inhibiting the PRL - JAK 2 - STAT 5 signaling pathway [10,11].
PSA is widely used in PCa detection, treatment outcome, and prognosis. PSA calibrates closely with disease status at its lower end, which enables PSA as a sensitive marker for early detection of PCa and a surrogate for recurrence and prognosis after radical treatment procedures such as radical prostatectomy, radiation, or minimally invasive treatment options [12].
Gao et al. performed a population-based screening of prostate cancer using serum PSA analysis and histological features of cancer, revealing that moderately differentiated carcinoma is the most common type of prostate cancer, the PSA value is associated with the Gleason score and tumor size [13].
It is important that the degree of differentiation, classification based on cell differentiation and the stromal-gland ratio of cancer be established in the report received from the pathologist. The Gleason scale goes from 2 to 10; being 2 the most benign cancer. In general, this scale is important because it determines the prognosis and evolution.
To date, there are no known alterations of FSH, LH and Prolactin in patients with malignant prostatic pathology. Because of this it is important to find out if PRL alterations are recorded [14].
Carboxypeptidase-D cleaves C-terminal arginine for conversion to nitric oxide (NO) by nitric oxide synthase. PRL and androgens stimulate CPD gene transcription and expression, which increases intracellular production of NO to promote viability of PCa cells in vitro [15].
Another non-steroidal factor that regulates the growth, development and differentiation of the prostate is PRL, which exerts its effect independently of androgens. It has been demonstrated that PRL has proliferative actions by a mechanism of signal transduction through PRL receptors. Other researchers also suggest that PRL promotes the growth and proliferation of prostatic cells in synergism with the androgens [16].
There is not enough information of the correlation of the PSA with the prolactin. Only having a proceeding exploratory analysis has shown that FSH was significantly correlated to and predicted by PSA in a prostate cancer population [17]. Highlighting the importance of this study because of the correlation of PSA/PRL.
MATERIAL AND METHODS
Observational, analytical and transverse study. In 50 Men older than 60 years with prostate cancer diagnosed for the first time in the service of Urology in the General Hospital of Zone 50 from November 2010 to February 2011.
Patients with medical treatment interfering with laboratory results in Prolactin Levels and PSA were excluded meanwhile patients who did not attend their laboratory appointment for sampling did not participate in the study.
In the service of urology, the intentional search of the patients with Prostate Cancer, without surgical or pharmacological treatment, with a complete clinical file, were informed about the study, provided the informed consent sheet, were questioned for the filling their registration card and cited the following day for the determination of LH, FSH , PRL, PSA, from the basilic vein using tourniquet and using 10 ml vacuum tubes and 9x38 gauge needles both Vacutainer, once the sample was obtained, cold centrifugation was carried out and the serum in freezing at -4 °C until the processing of samples by radioimmuno assay by a Chemistry, Department of Hormones, in the Laboratory of the General Hospital of Zone 1 with the Cobas Kit (Roche Diagnostics GmbH, Mannheim), containing the MODULAR ANALYTICS E170 self-analyzer (Cobas, Roche Diagnostics Indianapolis, IN)
Normal determination in men of LH: 1.7 - 8.6 mUI / mL .FSH: 1.5 - 12.4 mUI / mL.PRL:4.04 - 15.2 ng / Ml.PSA: 0.57 - 4.4 ng / m L for those over 60 years.
Histopathological results of prostate biopsy were obtained, which were previously sent to the Pathology Laboratory, obtained by direct puncture.
The statistical tests that were used with p ≥0.05: Mean, Standard Deviation and Analytical Student T and Pearson correlation. Three groups were classified in the Gleason Scale: Grade I, Grade II and Grade III. Comparing the four groups of hormone levels: PRL, PSA, LH, FSH, and compared the association of the four groups of hormone levels with grade of malignancy using the Chi square. The data obtained were statistically analyzed (SPSS 20.0 for Windows, Chicago, USA).
RESULTS
The average age of the patients was 72.3 years, as shown in Table 1, which states the range and Standard Deviation of the variables studied in the patients.
Table 1: Range, Average and Standard Deviation of the variables studied in the patients.
|
Table 1: Range, Average and Standard Deviation of the variables studied in the patients.. |
||||
|
n=50 |
Minimum |
Maximum |
Average |
Standard deviation |
|
AGE |
60 |
93 |
72.3 |
8.18 |
|
PSA |
1.4 |
20 |
8.5 |
3.88 |
|
PROLACTIN |
2.8 |
23.2 |
10 |
4.77 |
|
LH |
0.1 |
18.9 |
4.0 |
4.49 |
|
FSH |
1.4 |
40.1 |
5.6 |
5.81 |
|
GLEASON SCORE |
2 |
10 |
5.9 |
2.5 |
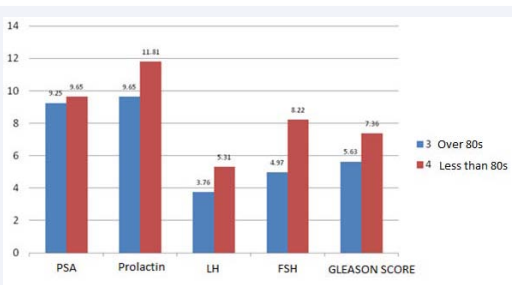
Prostate Specific Antigen, Prolactin, LH and FSH levels, as well as the Gleason score in the groups of the third and fourth age, although they were higher in the second group, did not reach a significant difference after the analysis in the Student’s T test, as shown in Figure 1.
Figure 1 The levels of prostate specific antigen, prolactin, LH and FSH, as well as the score of Gleason in both groups.
p ≥0.05 n=50
Patients with abnormal PSA results were 82% and 18% normal, Prolactin levels were abnormal in 12% and normal in 88% of the patients studied, LH levels were normal in 44% of patients and Abnormal in 56% and with FSH normal 82 % and abnormal 18%.
The averages of the hormones FSH, LH and PRL of the patients with and without familiar history of prostate cancer did not have a significant difference in any of them, neither in prostate antigen nor age, but there was a significant difference of means in the score of both groups of the Gleason classification. It was found an association by Chi square between 22 patients with a family history of prostate cancer and the histopathological grade of Gleason II, as shown in Table 2.
Table 2: Association by Chi square between 22 patients with a family history of prostate cancer and the histopathological grade of Gleason II.
|
Table 2: Association by Chi square between 22 patients with a family history of prostate cancer and the histopathological grade of Gleason II. |
|||
|
n=50 |
Familiar antecedent positive(N=22 |
Familiar antecedent negative(N=28) |
p<0.05=Significance |
|
PRL |
11.1 |
9.1 |
* NS |
|
LH |
5.0 |
3.0 |
*NS |
|
FSH |
5.7 |
5.7 |
*NS |
|
AGE |
72.2 |
70.1 |
*NS |
|
PSA |
8.5 |
8.0 |
*NS |
|
GLEASON SCORE |
7.0 |
4.3 |
0.000 |
|
*NS: No Significance |
|||
When performing the Pearson correlation tests, we only found positive and significant correlation <0.05 with age and the degree of Gleason score.
DISCUSSION
In elderly men, the incidences of PCa and BPH (Benign Prostate Hypertrophy) are increasing, but the pathogenesis of PCa and BPH is still poorly understood. Sex hormones and stromal–epithelial interactions are key factors involved in prostate growth, development and differentiation [20].
It was no found direct relation between PSA and PRL, it does not clears but it proves it does not exist. Unlike Patients with increased FSH levels with related lower levels of Testosterone, which was associated with high grade cáncer [21].
A large number of publications have established prostate cancer prognoses, the Gleason grade has statistically significance association, which we found between the family history of prostate cancer and the degree of differentiation of Gleason which may express a potential utility for clinical applications.
On the contrary it had been published that Gleason differentiation levels are independent factors of the Specific Prostate Antigen, but have found direct correlation. As a result of our analysis, the elderly studied showed a higher degree of Gleason score in relation to age, which agrees with other authors. Being relevant for the following discovery; increasing age was associated with an increased risk of PCa mortality only in Gleason score 6 [22].
CONCLUSION
Cancer is primarily a disease of older people, with incidence rates increasing with age for most cancers. Prostate Cancer not being the exception.
This finding allows to know that there is no direct correlation between PSA and PRL, nevertheless it is related to prostate cancer. Being possible to be used as a prognostic tool as marker but it is required more studies.
There is an association between Gleason Score and Familiar antecedent of Prostate Cancer. Patients with familiar antecedent will have higher Gleason Score than those who do not present.
Only a large-scale trial involving a large number of patients over 60 years of age, where serum levels of a panel of hormones may respond to many questions raised in this study, but will provide us with the unique opportunity to study the influence hormone in the pathophysiology of the prostate.
ACKNOWLEDGEMENTS
To Gerardo-Hernández Hector and Ortiz-Nesme Francisco Javier for his support and collaboration for the statistical analysis.
REFERENCES
- Cancer Today. UICC. 2017.
- Nesvadba M, Cmorej P, Mamova A, Slowik O. The incidence, mortality and risk factors of prostate cancer. 2017; 65: 211-214.
- Salas F, Rada F, Kobashigawa A, Torres C, Milla P, Aliaga C, et al. Consideraciones generales en el manejo del Cáncer de Próstata resistente a la castración. Carcinos. 2014; 4: 37-47.
- García-Cruz E, Carrión Puig A, García-Larrosa A, Sallent A, Castañeda-Argáiz R, Alcaraz A, et al. Higher sex hormone-binding globulin and lower bioavailable testosterone are related to prostate cancer detection on prostate biopsy. Scandinavian Journal of Urology. 2012; 47: 282-289.
- Sawada N, Iwasaki M, Inoue M, Sasazuki S, Yamaji T, Tsugane S, et al. Plasma testosterone and sex hormone-binding globulin concentrations and the risk of prostate cancer among Japanese men: a nested case-control study. Cancer Sci. 2010; 101: 2652-2657.
- Slater S, Oliver R. Testosterone: Its Role in Development of Prostate Cancer and Potential Risk from Use as Hormone Replacement Therapy. Drugs & Aging. 2000; 7: 431-439.
- Nakonechnaya A, Shewchuk B. Growth hormone enhances LNCaP prostate cancer cell motility. Endocr Res. 2015; 40: 97-105.
- Rick FG, Schally AV, Szalontay L, Block NL, Szepeshazi K, Nadji M, et al. Antagonists of growth hormone-releasing hormone inhibits growth of androgen-independent prostate cancer through inactivation of ERK and Akt kinases. Proc Natl Acad Sci U S A. 2012; 109: 1655-1660.
- O'Sullivan C, Bates S. Targeting Prolactin Receptor (PRLR) Signaling in PRLR-Positive Breast and Prostate Cancer. The Oncologist. 2016; 21: 523-526.
- Mendoza-Romo MA, García-Peña E. The role of prolactin in prostatecancer. Revista Mexicana de Urología. 2010; 70: 55-60.
- Hung-Cheng K, Chen-Pang H, Yu-Hsiang L, Ke-Hung T, Phei-Lang C, Chien-Lun C. Prognosis of prostate cancer with initial prostate-specific antigen >1,000 ng/mL at diagnosis. Onco Targets Ther. 2017; 10: 102943-2949.
- Gao HW, Li YL, Wu S, Wang YS, Zhang HF, Pan YZ, et al. Mass screening of prostate cancer in Chinese population: the relationship between pathological features of prostate cancer and serum psortate specific antigen. Asian J Androl. 2005; 7: 159-163.
- Epstein JI. An update of the Gleason grading system. J Urol. 2010; 183: 433-440.
- Thomas L, Merrimen J, Bell D, Rendon R, Too C. Prolactin- and testosterone-induced carboxypeptidase-D correlates with increased nitrotyrosines and Ki67 in prostate cancer. The Prostate. 2015; 75: 1726-1736.
- Rodríguez-López MR, Baluja-Conde IB, Bermúdez-Velásquez S. Patologías benignas de la próstata: prostatitis e hiperplasia benignaRevBiomed 2007; 18: 47-59.
- Porcaro A, Migliorini F, Petrozziello A, Sava T, Romano M, Comunale L, et al. Follicle-stimulating hormone and the pituitary-testicular-prostate axis at the time of initial diagnosis of prostate cancer and subsequent cluster selection of the patient population undergoing standard radical prostatectomy. Urologia Internationalis. 2013; 90: 45-55.
- Campos-Salcedo JG, Torres-Salazar JJ, Aragón-Flores M, Ricardez-Espinosa AA, Pacheco-Bouthillier DJ. Correlaciónclínico histopatológica del cáncer de próstata clínicamente localizado ylaangiogénesis. Rev Sanid Milit Mex. 2007; 61: 13-17.
- Goffin V, Bernichtein S, Touraine P, Kelly PA. Development and Potential
Clinical Uses of Human Prolactin Receptor Antagonists. Endocr Rev.
2005; 26: 400-422. - Jiang Q, Han B, Zhao F, Hong Y, Xia S. The differential effects of prostate stromal cells derived from different zones on prostate cancer epithelial cells under the action of sex hormones. Asian J Androl. 2011; 13: 798-805.
- Porcaro A, Siracusano S, de Luyk N, Corsi P, Sebben M, Artibani W, et al. Simultaneous Measurements of Follicle Stimulating Hormone and Total Testosterone and Associations in Clinically Localized Prostate Cancer. Current Urology. 2017; 10: 174-181.
- Russo A, Chen M, Aizer A, Hattangadi J, D'Amico A. Advancing age within established Gleason score categories and the risk of prostate cancer-specific mortality (PCSM). BJU International. 2012; 110: 973-979.