Study on Infestation Level of GIT Parasites and Antihelmentic Drug Resistance of Sheep in Horro District Community Based Breeding Program, Western Ethiopia
- 1. Dairy Animal Health at Bako Agricultural Research Center, Oromia Agricultural Research Institute, Ethiopia
Abstract
Parasites remain a major threat to the health and welfare of animals all over the globe. The impact is greater in Africa in general and in Ethiopia in particular due to the availability of a wide range of agro-ecological factors suitable for diversified hosts and types of helminthes. Therefore, the objectives of the experiment were to estimate the infestation level of parasites, to know the associated risk factors and to identify the presence antihelmentic drug resistance. In the present study both fecal sedimentation and floatation techniques were used for trematode and nematode eggs identification, respectively. As well as two types of drugs namely Albenda-qk 600 mg and Flukash Sheep (Oxyclozanide 340 mg) were used to distinguish the existence of antihelmentic drug resistance and STATA (version 13) statistical software used to analysis the associated risk factors. As the study result indicated the prevalence of nematode and trematode during pre-treatment period were 66% and 29%, respectively, whereas the prevalence of nematode and trematode during post-treatment period 7% and 3%, respectively. As multivariable logistic regression model analysis result showed that age and stage of deworming were statistically significant association with both nematode and trematode positivity (P < 0.05). Even though, there was statistically significant variation (P < 0.05) of both nematode and trematode parasite positivity between pre-treatment and post-treatment period there were still small group of sheep flocks have been developed resistance. Therefore, to prevent further the development of anthelmintic drug resistance intervention activities such as strategic and integrated antihelmentic drug application, avoidance of under dosage of animal treatment and application of antihelmetic drugs rotation and anthelmintic efficacy test should also be practiced regularly.
Keywords
• Gastro-intestinal parasite
• Prevalence
• Risk factors
• Antihelmentic drug resistance
CITATION
Cherinnat TM (2024) Study on Infestation Level of GIT Parasites and Antihelmentic Drug Resistance of Sheep in Horro District Community Based Breeding Program, Western Ethiopia. J Vet Med Res 11(2): 1267.
ABBREVIATIONS
GIP: Gastro-Intestinal Parasite; RF: Risk Factors; ADS: Antihelmentic Drug Resistance
BACKGROUND AND JUSTIFICATION
Among many diseases that affect small ruminant, gastrointestinal parasite is the major in our country Ethiopia. Gastrointestinal parasites are a world-wide problem in livestock as well as in agricultural sector and responsible for major economical losses. Parasites remain a major threat to the health and welfare of animals all over the globe. Infections with gastro- intestinal helminthes have detrimental effect on animal health [1], Economic losses associated with parasites occur in the form of morbidity, mortality, and reduced feed conversion rate (FCR), inefficient production, reduced weight gain, retarded growth, decreased fertility and cost incurred on their treatment [2]. Thus, the economic impact of these parasites in animals industry is great. The impact is greater in Africa in general and Ethiopia in particular due to the availability of a wide range of agro-ecological factors suitable for diversified hosts and types of helminthes [3,4].
Therefore, the strategic control of parasites is essential to minimize the production losses by reducing transmission of parasites and sustaining reproduction and optimum livestock productivity, but, total dependence on a single method of control has proved to be non-sustainable and cost ineffective in the long term [5,6]. A combination of treatment and management is necessary to control parasitism so that it will not cause economic loss to producer [7,8]. Hence, in order to become practically and ecologically sustainable, parasitic control schemes need to be based on strategic and integrated control [6-8]. However, nowadays anthalmentic efficacy against nematodes is reducing due to rise of parasitic resistance [9]. The anthelmentic resistance has been almost reported in different parts of countries including our country Ethiopia. Actually there are factors that associated with parasitic anthlementic resistance such as maturity stage of parasite, sexual phase of parasite, immune response of host which can be age related and history of infected animal and distribution of worms.
Therefore, the objectives of this experiment were to estimate the infestation level of parasites of sheep, to know the associated risk factors and to identify the presence of antihelmentic drugs resistance in the community based sheep breeding program of the study area.
MATERIAL AND METHODS
Study area
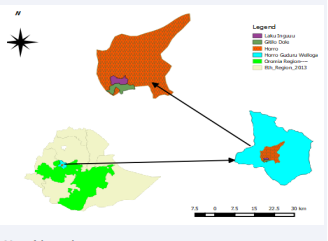
The experiment was carried out in Horro district (Gitlo-Dole and Laku-Ingu kebeles) which is found in Horro-Guduru Wollega zone of Oromia regional state, Western Ethiopia. Horro District is located about 310 kms distance West of Addis Ababa.
Map of the study areA
Study Animals
The study animals were sampled Sheep population which kept under extensive husbandry systems in the community based sheep breeding program of Horro District and comprised history of non treated animal for a minimum of 6 months ahead and consecutive follow up was made based their ear-tag identification number, accordingly.
EXPERIMENTAL DESIGNS AND METHODS
In this study the study population was has been kept under the same management system and equal sample size was considered for the two kebeles. To obtain reliable information, the same expert was conducted during pre and post deworming of laboratory fecal sample analysis. The purpose of the study was fully explained to owners before conducting the study to have owners’ agreement and understanding. On each study flock, two visits have been done. Firstly; during pre-deworming stage (before intervention) fecal samples were taken in order to identify the status of small ruminant GIT parasites in the study site. Secondly, post-deworming stage (after intervention) after three weeks fecal sample collection was conducted once again with the objective of identifying the status parasite as well as to know the impact of drugs on GIT parasites in the study area.
SAMPLE SIZE AND ANTHELMINTICS DRUGS USED
A total sample size of 400 fecal samples were examined during pre and post deworming stage and of the aforementioned sample size 200 samples were tested for nematode and fecal floatation technique used whereas 200 were tested for trematodes and fecal sedimentation technique used. And from each PA 100 fecal samples (50 for nematode and 50 for trematodes) were examined during pre-deworming stage. As well as from each PA 100 fecal samples (50 for nematode and 50 for trematodes) were examined during post-deworming stage. In conclusion, 200 fecal samples were taken from each PA during pre and post deworming stage, which gives a total sample size of 400. In this experimental study type of anthelmintic drugs used were ALBENDA-QK 600 mg to deworm nematode parasite and FLUKASH SHEEP (Oxyclozanide 340 mg bolus) for deworming of faciola (trematode parasite).
DATA COLLECTION
Fecal samples of sheep were collected for parasitic eggs test. Therefore, from each sampled animal about 5gm of feces was collected. The collected samples were properly labeled and transported to Bako Agricultural Research Center animal health laboratory with an ice box and laboratory analysis was conducted, accordingly.
DATA ANALYSIS
The fecal sample test result data was stored on Microsoft Excel spread sheet and analysis was done using SPSS ver. 20 and STATA (version 13) statistical softwares. GIT parasite prevalence was analyzed using SPSS ver. 20 descriptive statistics (crosstabs) while degree of associations between the outcome variable and its potential risk factors were analyzed using STATA using logistic regression model. Microscopic feces result was considered as the dependent variable whereas the risk factors like PA, sex, age, BCS and stage of deworming were grouped as independent variables (Tables 1-5).
Table 1: Shows prevalence of nematode parasite during Pre-deworming stage.
|
Risk factors |
No Tested |
No of positive |
% (95% CI) |
|
PA(kebele) |
|
|
|
|
Laku |
50 |
31 |
62(0.47-0.75) |
|
Gitlo |
50 |
35 |
70(0.55-0.82 ) |
|
Sex |
|
|
|
|
Female |
80 |
53 |
66.2 (0.55-0.76) |
|
Male |
20 |
13 |
65( 0.41-0.85) |
|
Age |
|
|
|
|
Young |
25 |
19 |
76(0.55-0.91) |
|
Adult |
75 |
47 |
62.7(0.51-0.74 ) |
|
BCS |
|
|
|
|
Good |
17 |
10 |
58.8(0.33-0.82) |
|
Medium |
45 |
30 |
66.7(0.51-0.80) |
|
Poor |
38 |
26 |
68.4(0.51-0.82) |
|
Total |
100 |
66 |
66(0.56-0.75) |
Table 2: Shows prevalence of nematode parasite during Post-deworming stage
|
Risk factors |
No Tested |
No of positive |
% (95% CI) |
|
PA(kebele) |
|
|
|
|
Laku |
50 |
5 |
10(0.03-0.21) |
|
Gitlo |
50 |
2 |
4(0.005-0.14) |
|
Sex |
|
|
|
|
Female |
80 |
4 |
5(0.01-0.12) |
|
Male |
20 |
3 |
15(0.03-0.38) |
|
Age |
|
|
|
|
Young |
25 |
4 |
16(0.05-0.36) |
|
Adult |
75 |
3 |
4(0.01-0.11) |
|
BCS |
|
|
|
|
Good |
17 |
3 |
17.6(0.04-0.43) |
|
Medium |
45 |
3 |
6.7(0.01-0.18) |
|
Poor |
38 |
1 |
2.6(0.001-0.14) |
|
Total |
100 |
7 |
7(0.03-0.14) |
Table 3: Shows prevalence of trematodes parasite during pre-deworming stage
|
Risk factors |
No Tested |
No of positive |
% (95% CI) |
|
PA(kebele) |
|
|
|
|
Laku |
50 |
12 |
24(0.13-0.38) |
|
Gitlo |
50 |
17 |
34(0.21-0.49) |
|
Sex |
|
|
|
|
Female |
77 |
23 |
29.9(0.20-0.41) |
|
Male |
23 |
6 |
26.1(0.10-0.48) |
|
Age |
|
|
|
|
Young |
19 |
3 |
15.8(0.03-0.40) |
|
Adult |
81 |
26 |
32.1(0.22-0.43) |
|
BCS |
|
|
|
|
Good |
14 |
3 |
21.4(0.05-0.51) |
|
Medium |
55 |
16 |
29.1(0.18-0.43) |
|
Poor |
31 |
10 |
32.3(0.17-0.51) |
|
Total |
100 |
29 |
29(0.20-0.39) |
Table 4: Shows prevalence of trematodes parasite during Post-deworming stage
|
Risk factors |
No Tested |
No of positive |
% (95% CI) |
|
PA(kebele) |
|
|
|
|
Laku |
50 |
1 |
2(0.0005-0.11) |
|
Gitlo |
50 |
2 |
4(0.005-0.14) |
|
Sex |
|
|
|
|
Female |
77 |
1 |
1.3(0.0003 0.07) |
|
Male |
23 |
2 |
4(0.0107-0.28) |
|
Age |
|
|
|
|
Young |
19 |
1 |
5.3(0.0013- 0.26) |
|
Adult |
81 |
2 |
2.5(0.003 0.09) |
|
BCS |
|
|
|
|
Good |
14 |
1 |
7.1(0.002-0.34) |
|
Medium |
55 |
2 |
3.6(0.004-0.13) |
|
Poor |
31 |
0 |
0(0.001-0.17) |
|
Total |
100 |
3 |
3(0.006-0.09) |
Table 5: Multivariate logistic regression degree of association analysis of prevalence of nematode parasite
|
Significant Parameters |
Total |
% (95% CI) |
|
Report of odds ratios |
P-value |
|
|
|
|
OR (95% CI) |
Std. Err. |
|||
|
Age |
|
|
|
|
|
|
|
Young |
50 |
46(0.32-0.61) |
1 |
|
|
|
|
Adult |
150 |
33.3(0.26-0.41) |
0.4(0.16-0.98) |
0.18 |
0.045* |
|
|
Sample Type |
|
|
|
|
|
|
|
Post- deworming |
100 |
7(0.03-0.14) |
1 |
|
|
|
|
Pre- deworming |
100 |
66(0.56-0.75) |
28.5(11.6-70.5) |
13.2 |
0.000*** |
|
RESULT
That age and time of deworming were statistically significant association with both nematode and trematode positivity (P < 0.05). Such as the likelihood of positivity with nematode parasite in pre-deworming stage (OR=28.5, 95%CI: 11.6-70.5), p=0.000) was 25.5 times more likely than post-deworming stage and the likelihood of positivity with trematodes parasite of non- dewormed sheep (OR=13.2, CI95%:3.87-45.1, P=0.000) were thirteen times positive than dewormed sheep (Table 6).
Table 6: Multivariate logistic regression degree of association analysis of prevalence of faciola
|
Significant Parameters |
Total sample |
% (95% CI) |
|
Report of odds ratios |
P-value |
|
|
|
|
OR (95% CI) |
Std. Err. |
|||
|
Sample Type |
|
|
|
|
|
|
|
Post- deworming |
100 |
3(0.01-0.09) |
1 |
|
|
|
|
Pre- deworming |
100 |
29(0.20-0.39 ) |
13.2(3.87-45.1) |
8.27 |
0.000*** |
|
CONCLUSION AND RECOMMENDATION
Small ruminant GIT parasite resistance against broad spectrum anthelmintics is repeatedly reported in different parts of Ethiopia. The distribution pattern of anthelmintics resistance is great concern as country. Frequent use of the same drug, the use of under dose of drugs, poor regulation of drug marketing and professionally unsupervised drug use tend to increase the risk of multiple antihelmintic resistance development in different areas of the country. In the presence study the prevalence of nematode and trematode during pre-treatment were 66% and 29%, respectively whereas during post-treatment the prevalence were 7% and 3% for nematode and faciola, respectively. As the result revealed even though small groups of flock were positive after drug treatment there was no significant level of GIT parasite resistance development to ALBENDA-QK 600 mg for deworming of nematode parasite and FLUKASH SHEEP (Oxyclozanide 340 mg bolus) to treat faciola. Therefore to prevent further the development of anthelmintic drug resistance in the present study area the following practices such as avoidance of frequent usage of anthelmintics drugs, application of strategic and integrated antihelmentic drugs, avoidance of under dosage of animals treatment application of antihelmetic drugs rotation and anthelmintic efficacy test were recommended.
REFERENCES
- Lüscher A, Häring DA, Heckendorn F, Scharenberg A, Dohme F, Maurer V, et al. Use of tanniferous plants against gastrointestinal nematodes in ruminants. In: Köpke U, Niggli U, Neuhoff D, Cor-nish P, Lockeretz W, Willer H (eds) Researching sustainable systems. In: Proceedings of the first scientific conference of the international society of organic agriculture research (ISOFAR), 21–23, Adelaide, South Australia. Frick:Forschungsinstitutfürbiolo-gischenLandbau FIBL, 660 Parasitol. 2005; 29: 41-47.
- Perry BD, Randolph TF. Improving the assessment of the economic impact of parasitic diseases and of their control in production animals. Vet Parasitol. 1999; 84: 145–168.
- Sahoo N, Mohanty TN, Sambal S. Prevalence of gastrointestinal helminthic infection among grazing and stall fed cattle in rainfed district of Orissa. J Vet Parasitol. 2002; 16: 61-62.
- Nitin Padwal, Atul Humbe, Swati Jadhav, SN Borde. Seasonal variation of intestinal Trichuris sp. in sheep and goats from Maharashtra State. Int Multidiscip Res J. 2011; 1: 17-18.
- FAO. Sustainable approaches for managing haemonchosis in sheep and goats. In: FAO Animal Production and Health Paper. 2001; 90.
- Maqbool I, Wani ZA, Shahardar RA, Shah MM. Integrated parasite management with special reference to gastro-intestinal nematodes. J Parasit Dis. 2017; 41: 1-8.
- Scarfe AD. Approaches to managing gastrointestinal nematode parasites in small ruminants. 1993.
- Maqbool I, Wani ZA, Shahardar RA, Shah MM. Integrated parasite management with special reference to gastro-intestinal nematodes. J Parasit Dis. 2017; 41: 1-8.
- Sarginson ND, Jackson F, Scott PR. Multiple anthelmintic resistance in sheep. Vet Rec. 2001; 14: 778-779.