Factors that affect the Incidence of Obstetric Sphincter Injuries in a Rural Hospital, Ireland
- 1. Department of Obstetrics and Gynecology, Cork University Maternity Hospital, Ireland
- 2. Department of Obstetrics and Gynaecology, University College Cork, Ireland
- 3. Mayo University Hospital, Mayo Medical Academy, Ireland
Abstract
Aim: To describe the incidence of Obstetric anal sphincter injuries OASIs and factors that affect its pattern in a rural maternity unit.
Methods: Records on women who suffered third- and fourth-degree perineal tear after vaginal delivery from January 1st, 2008 to December 31st, 2017 were electronically retrieved. These cases were identified by the national coding system HIPE. Their age, maternal and fetal birth weight, ethnicity, parity, use of episiotomy, analgesia, and mode of vaginal delivery were analyzed. All women diagnosed with obstetric sphincter injury in the selected time frame were included in this study and women who suffered OASI more than once were counted as two different cases, but the previous history noted.
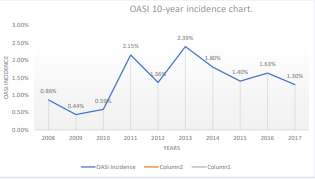
Results: A total of 11974 vaginal births, of which 163 cases of Obstetric sphincter injuries were recorded over the 10-year period (i.e 16.3 cases of OASI/year). The overall incidence in this unit was 1.3%, although if calculated from 2011 onwards the incidence was 1.7%. The highest annual cases (n=28), occurred in 2011. We found a higher rate of OASIs in women who suffered shoulder dystocia 6.1%. Overweight and obese mothers who had OASI were 48% (n=78) while the majority of the OASI cases were first-time mums 76% (n=124). There was the same frequency of Type 3a and 3b third-degree tears 38.7 % (n=63), and only one case of buttonhole tear. The mean age in the OASI patients was 30.6 years and similarly at 31.6 years in all women who had vaginal delivery within the study period.
Conclusion: The incidence of OASI rose sharply in the year 2011, that first peak coincides with the release of the first draft version of the Irish Institute of obstetrics and gynecology guideline on diagnosis and management of Obstetric sphincters, also there was training of maternity staff in December 2010 in clinical assessment and examination of all patients following vaginal delivery. We suspect this pattern of incidence was due to improvement in diagnoses rather than changes in risk factors. In this study, there wasn’t a clear pattern in maternal age and weight to suggest an association with the incidence of OASI. Clear management guidelines and hands-on training can improve the diagnosis and management of obstetric sphincter injuries.
Keywords
• OASIs
.• Third - fourth-degree tear
.• Perineal tear
• Obstetric sphincter injuries
Citation
Aina AD, Meaney S, Bhuinneain MN (2025) Factors that affect the Incidence of Obstetric Sphincter Injuries in a Rural Hospital, Ireland. Med J Obstet Gynecol 13(2): 1196.
INTRODUCTION
Obstetric anal sphincter injuries (OASIs) are perineal lacerations that extend to the anal sphincter and/or anal mucosa during vaginal delivery. These injuries represent a severe complication of vaginal birth, necessitating prompt diagnosis and comprehensive management to prevent long-term sequelae. The incidence of OASIs is approximately 3-5% of all vaginal deliveries, often leading to significant long-term issues such as pelvic floor dysfunction, anal incontinence, and sexual health problems [1]. While perineal lacerations are common during vaginal deliveries and typically heal with minimal or no long-term complications, those involving the anal sphincter and/or anal mucosa require immediate recognition and repair, as well as multifaceted management to mitigate potential morbidity. Unrecognized or improperly managed OASIs can result in anal incontinence, sexual dysfunction, and chronic perineal pain, substantially impacting the physical and emotional quality of life for affected women.
Interestingly, the reported incidence of OASIs has increased globally over the past decade, despite a decline in the overall number of vaginal deliveries. Studies suggest that this rise may be attributed to improved recognition and reporting practices rather than a true increase in occurrence. However, recent data indicate that rising rates of interventional procedures (e.g., episiotomy, forceps, and vacuum delivery), particularly during the second stage of labor, could also contribute to this trend [2]. Additionally, changes in maternal risk factors, such as increasing maternal age and weight, have been implicated [3].
Evaluating the true incidence and patterns of OASIs presents challenges due to significant variations in obstetric practices across different maternity units and countries. Scrutinizing established risk factors and their changes over time may be essential for plotting trends and standardizing research in this area. One study demonstrated the importance of a single risk factor in influencing incidence rates and patterns, reporting a significant reduction in OASIs from 5.4% to 1.3% over a tenyear period, linked to a decrease in the routine episiotomy rate from 31% to 3.5% during the same timeframe [4].
Several risk factors have been well-studied, achieving international consensus: primiparity, operative vaginal delivery (especially forceps), operative vaginal delivery without episiotomy, birth weight over 4 kg, and Asian ethnicity are all associated with an increased risk of OASIs [1,5,6]. Identifying key risk factors is crucial not only for monitoring incidence and guiding research but also for educating and managing at-risk patients to reduce the occurrence of OASIs, particularly the modifiable factors. While maternal age and weight have been examined in relation to OASIs, findings have been inconsistent. Most studies suggest a linear association between age and OASI risk, while others found no correlation [4,7]. One study explained the age-OASI association through increased internal anal sphincter muscle thickness, hypothesizing that diameter increases with age, thereby elevating incontinence risk even in the absence of obstetric injury, although comparisons were primarily between younger women and those around 60 years [8].
Standardized classifications for maternal age and weight remain lacking, complicating result comparisons.
Obesity represents a global health challenge, and the obstetric population in Ireland and worldwide is increasingly affected. The consequences of unhealthy diets and sedentary lifestyles contribute to multiple health risks. Notably, some studies suggest that higher maternal weight might be protective against OASIs, though conflicting reports are emerging. Research from Sweden consistently indicates that a higher body mass index (BMI) serves as a protective factor for OASIs, whereas studies from nonScandinavian countries have reported contrary findings [9,10]. A clinical trial further suggested that increased anovaginal distance in obese women may account for this protective effect against OASIs [11]. This study investigates modifiable risk factors, specifically weight and age, and examines the incidence of OASIs in a local rural population in Ireland over a tenyear period, considering contributing factors to observed patterns.
MATERIALS AND METHODS
This study was conducted in a rural hospital with an average annual birth rate of 1,700 live births. We retrieved records of deliveries complicated by third- or fourthdegree tears from January 1, 2008, to December 31, 2017, using HIPE coding. All cases were included. We reviewed electronic records of OASI cases, gathering information on age, ethnicity, booking weight, birth weight, parity, instrumental delivery, episiotomy, and type of OASI.
We categorized maternal age into three groups: “less than 25 years,” “25 to 35 years,” and “more than 35 years,” using ranges consistent with literature [12,13]. Maternal booking weight was evaluated by BMI and grouped according to the World Health Organization (WHO) classification. Data were collected in Excel and analyzed using IBM SPSS Statistics software. Deliveries were attended by midwives, trainee obstetricians, or consultant obstetricians, with all operative vaginal deliveries performed by a doctor. During the study period, consultant obstetricians remained consistent, while trainee obstetricians changed yearly due to training rotations, resulting in varying levels of experience; however, inexperienced trainees (less than three years on the labor ward) were supervised during deliveries.
RESULTS
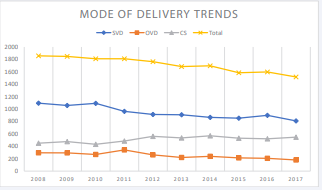
During the ten-year period, 11,974 women underwent vaginal deliveries, of which 163 experienced OASIs, resulting in a mean of 16.3 cases per year. The overall incidence was 1.3%, with an average of 1,197 vaginal deliveries annually. The number of vaginal deliveries ranged from 1,390 in 2008 to 989 in 2017. The highest number of sphincter injuries (n=28) occurred in 2011, with another peak in 2013 (n=27); episiotomy rates were also elevated during these years. Approximately 66% of women in the OASI group were aged 26 to 35, with the remaining participants nearly evenly split between the “less than 25” and “above 35” age groups. The average age of women in the OASI group was 30.6 years, compared to an average maternal age of 31.6 years for all women who delivered during the study period.
About 50% of the OASI group had a normal BMI of less than 25, while only 2.5% were classified as severely obese (BMI > 35). OASIs were associated with shoulder dystocia in 6.1% of cases, and 31% (n=50) had a baby weighing more than 4 kg. The distribution of third-degree tears was equal between types 3a and 3b.
DISCUSSION
The fertility rate, as indicated by live births, decreased from 2008 to 2017, mirroring a similar trend in vaginal deliveries. In contrast, the operative vaginal delivery rate remained stable over this period. The overall incidence of OASIs in this study (1.3%) is significantly lower than the 3-5% rates typically reported in international studies [1], although rates as low as 1% have been documented [4,14]. Factors such as missed diagnoses and under-reporting, particularly in earlier years when documentation and classification of perineal injuries were less stringent, may contribute to the lower incidence rates observed. A study conducted in another Irish hospital reported an OASI incidence rate of 1.7% among 20,000 women with vaginal deliveries in 2003.
The pattern of OASIs in this study indicated a steady increase until 2011, followed by sharp increases in 2014, before returning to a steady rise. Given the decline in overall deliveries and vaginal deliveries during this period, it is unlikely that these peaks were incidental. Although multiple factors influence the incidence of OASIs-such as changing risk factors, increasing maternal weight and age, and evolving obstetric practices driven by a litigious climate-the notable increase in 2011 may stem from other influences. The practices at our unit remained largely unchanged, including second-stage interventions like operative deliveries and as-needed episiotomies (all right mediolateral) (Table 1).
Table 1: OASIs risk factors and OASIs degree.
|
Factors |
3a |
3b |
3c |
4 |
BH |
Total |
||||||
|
|
n |
(%) |
n |
(%) |
n |
(%) |
n |
(%) |
n |
(%) |
n |
(%) |
|
AGE |
||||||||||||
|
≤25 |
13 |
(20.7) |
10 |
(15.9) |
1 |
(9.1) |
2 |
(22.2) |
0 |
(0) |
26 |
(17.7) |
|
26-35 |
43 |
(68.3) |
41 |
(65.1) |
8 |
(72.7) |
5 |
(55.6) |
1 |
(100) |
98 |
(66.7) |
|
≥36 |
7 |
(11.1) |
12 |
(19.0) |
2 |
(18.2) |
2 |
(22.2) |
0 |
(0) |
23 |
(15.6) |
|
BMI |
||||||||||||
|
<18.5 |
0 |
(0.00) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
|
18.5-25 |
31 |
(50.8) |
37 |
(58.7) |
6 |
(54.5) |
3 |
(33.3) |
0 |
(0) |
77 |
(53.1) |
|
26-30 |
25 |
(40.9) |
18 |
(28.6) |
5 |
(45.5) |
4 |
(44.4) |
1 |
100 |
53 |
(36.6) |
|
31-35 |
4 |
(6.6) |
6 |
(9.5) |
0 |
(0) |
1 |
(9.1) |
0 |
(0) |
11 |
(7.6) |
|
36-40 |
1 |
(1.6) |
2 |
(3.2) |
0 |
(0) |
1 |
(9.1) |
0 |
(0) |
4 |
(2.8) |
|
>40 |
0 |
(0.0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
|
PARITY |
||||||||||||
|
Primigravida |
45 |
(72.6) |
48 |
(76.2) |
8 |
(72.7) |
8 |
(88.9) |
1 |
(50) |
110 |
(74.8) |
|
Para 1 |
12 |
(19.4) |
10 |
(15.9) |
2 |
(18.3) |
0 |
(0) |
0 |
(0) |
24 |
(16.3) |
|
Para 2-4 |
5 |
(8.1) |
4 |
(6.3) |
1 |
(9.0) |
1 |
(11.1) |
1 |
50 |
12 |
(8.2) |
|
Para >4 |
0 |
(0) |
1 |
(100) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
1 |
(0.7) |
|
EPISIOTOMY |
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
32 |
(49.2) |
29 |
(46) |
4 |
(36.4) |
5 |
(55.6) |
0 |
(0) |
72 |
(48.3) |
|
No |
31 |
(50.8) |
34 |
(54) |
7 |
(63.6) |
4 |
(44.4) |
1 |
(100) |
77 |
(51.7) |
|
MOD* |
||||||||||||
|
SVD |
29 |
(46) |
32 |
(50.8) |
7 |
(63.6) |
3 |
(33.3) |
1 |
(100) |
72 |
(49.6) |
|
Kiwi |
13 |
(20.6) |
11 |
(17.5) |
0 |
(0) |
1 |
(11.1) |
0 |
(0) |
25 |
(17.2) |
|
Forceps |
11 |
(17.5) |
10 |
(15.9) |
3 |
(27.3) |
4 |
(44.4) |
0 |
(0) |
28 |
(19.3) |
|
Kiwi+Forceps |
9 |
(14.3) |
9 |
(14.3) |
1 |
(9.1) |
1 |
(11.1) |
0 |
(0) |
20 |
(13.7) |
|
Metal Cup |
1 |
(1.6) |
1 |
(1.6) |
0 |
(0) |
0 |
(0) |
0 |
(0) |
2 |
(1.3) |
|
Fetal BW* |
||||||||||||
|
< 4kg |
49 |
(77.7) |
42 |
(66.7) |
5 |
(45.5) |
4 |
(44.4) |
1 |
(100) |
101 |
(68.7) |
|
≥4kg |
14 |
(22.2) |
21 |
(33.4) |
6 |
(54.6) |
5 |
(55.6) |
0 |
(0) |
46 |
(31.3) |
First, in January 2011, the Irish Institute of Gynecology released a draft guideline on diagnosing and managing obstetric sphincter injuries, the first national guideline on this subject. While most obstetricians were likely familiar with the British version of the guideline, its national focus may have shifted daily practices, improving diagnoses and reporting. The second peak in 2014 coincided with the release of the full version of this guideline, following a national study [15] (Figure 1).
Figure 1 Incidence pattern of OASI over a 10-year period.
Secondly, in 2010, all midwifery and obstetric staff received training on sphincter examination using the pinrolling method after every vaginal delivery, regardless of whether a perineal lesion was present. This initiative was prompted by an isolated clinical finding of a defective sphincter in a patient previously thought to have a minimal perineal tear. The synergistic effects of these guidelines and clinical training likely contributed to the reported increase in incidence in subsequent years.
Improved diagnosis, reporting, and changes in routine obstetric practices are two key factors that likely influenced the incidence pattern in this small obstetric unit. Changes in maternal age and weight also warrant consideration as potential contributors to the rising incidence of OASIs [16]. Maternal age in Ireland, as well as in the developed world, is increasing, as is maternal weight. Therefore, we examine these factors and their potential impact on the risk of OASIs.
The maternal age steadily increased over the tenyear period in our unit, consistent with the global trend of women delaying childbirth. The mean age in the OASI group was 30.6 years, compared to the general obstetric population, which averaged 31.6 years. There was no overrepresentation of older women in the OASI group. In 2015, the national average age for a woman entering pregnancy was 32 years, with approximately 55% of women aged between 25 and 34-similar to the OASI group in this study [17]. This finding aligns with studies demonstrating no correlation between maternal age and the risk of OASIs [6,18].
Regarding maternal weight, about 50% of women who experienced OASIs were overweight or obese (BMI > 25). Although this finding is not directly compared to general obstetric population data, a study of the Irish population reported that 44% of women are either overweight or obese at the start of pregnancy [19]. While direct inferences cannot be drawn from this data, the figures suggest no significant BMI skew in the study group, with the weight distribution among these women resembling that of the broader pregnant population in the country. As previously noted, research on BMI as a risk factor for OASIs remains inconclusive, and this study did not provide evidence to suggest otherwise (Figure 2).
Figure 2 Trends in the mode of deliveries over the 10-year period.
Shoulder dystocia complicates approximately 1.4% to 1.9% of all vaginal deliveries and is associated with a threefold increased risk of OASIs [20]. In our study, about 6% of women with sphincter injuries also experienced shoulder dystocia, slightly higher than reported in the literature. This finding may further explain the low incidence of OASIs in our study, potentially indicating underdiagnosis, as there is typically a heightened awareness for sphincter injuries following shoulder dystocia.
CONCLUSIONS
The low incidence of obstetric sphincter injuries in this rural hospital aligns with national rates, including those from larger obstetric units in Ireland. The spike observed in 2011 is likely attributable to heightened awareness following the introduction of new guidelines and improved diagnostic practices through local training and clear protocols. The association of shoulder dystocia with increased rates of OASIs corroborates previous findings and emphasizes the importance of thorough examinations for women experiencing shoulder dystocia. While maternal age and weight are rising modifiable factors within the global pregnant population, these factors do not appear to influence the incidence of OASIs in our institution over the past decade, despite a steady increase in mean maternal age
REFERENCES
- Meister MRL, Cahill AG, Conner SN, Woolfolk CL, Lowder JL. Predicting obstetric anal sphincter injuries in a modern obstetric population. Am J Obstet Gynecol. 2016; 215: 310.
- Tyagi V, Perera M, Guerrero K, Tyagi V, Perera M, Guerrero K. Trends in obstetric anal sphincter injuries over 10 years Trends in obstetric anal sphincter injuries over 10 years. 2013; 36: 844-849.
- E. B, L.M. I, P.E. B, S. R. Trends in risk factors for obstetric analsphincter injuries in Norway. Obstet Gynecol. 2010; 116: 25-33.
- Kudish B, Sokol RJ, Kruger M. Trends in major modifiable risk factors for severe perineal trauma, 1996-2006. Int J Gynecol Obstet. 2008;102: 165-170.
- Edozien LC, Gurol-Urganci I, Cromwell DA, Adams EJ, Richmond DH, Mahmood TA, et al. Impact of third- and fourth-degree perineal tears at first birth on subsequent pregnancy outcomes: A cohort study. BJOG An Int J Obstet Gynaecol. 2014; 121.
- Samarasekera DN, Bekhit MT, Preston JP, Speakman CTM. Risk factors for anal sphincter disruption during child birth. Langenbeck’s Arch Surg. 2009; 394: 535-538.
- Dahl C, Kjølhede P. Obstetric anal sphincter rupture in older primiparous women: A case-control study. Acta Obstet Gynecol Scand. 2006; 85: 1252-1258.
- Huebner M, Margulies RU, Fenner DE, Ashton-Miller JA, Bitar KN, DeLancey JOL. Age effects on internal anal sphincter thickness and diameter in nulliparous females. Dis Colon Rectum. 2007; 50: 1405- 1411.
- Blomberg M. Maternal body mass index and risk of obstetric anal sphincter injury. Biomed Res Int. 2014; 2014.
- Hjertberg L, Uustal E, Pihl S, Blomberg M. Maternal Body Mass Index and Anovaginal Distance in Active Phase of Term Labor. 2018; 2018: 1532949
- Dietz HP, Simpson JM. Does delayed child-bearing increase the risk of levator injury in labour? Aust New Zeal J Obstet Gynaecol. 2007; 47: 491-495.
- Rahmanou P, Caudwell-Hall J, Kamisan Atan I, Dietz HP. The association between maternal age at first delivery and risk of obstetric trauma. Am J Obstet Gynecol. 2018; 215: 451.e1-451.e7.
- Baghestan E, Irgens lorentz M, Bordahl PE, Rasmussen S. Trends in risk factors for obstetric anal sphincter injuries in Norway. Obstet Gynecol. 2010; 16: 25-34.
- Guideline CP, Of M, Anal O, Injury S. CLINICAL PRACTICE GUIDELINE MANAGEMENT OF OBSTETRIC ANAL SPHINCTER INJURY Institute ofObstetricians and Gynaecologists and Directorate of Clinical Strategyand Programmes. 2014; 8: 1-20.
- Tyagi V, Perera M, Guerrero K. Trends in obstetric anal sphincter injuries over 10 years. J Obstet Gynaecol (Lahore). 2013; 33: 844-849.
- Health Service Executive. Perinatal Statistics Report 2013. 2014.
- Dahl C, Kjølhede P. Obstetric anal sphincter rupture in older primiparous women: A case-control study. Acta Obstet Gynecol Scand. 2006; 85: 1252-1258.
- E. K, V. O, C. F, N. F, C. O, M.J. T. Correlation between birth weight and maternal body composition. Obstet Gynecol. 2013; 121: 46-50.
- Gauthaman N, Walters S, Tribe IA, Goldsmith L, Doumouchtsis SK. Shoulder dystocia and associated manoeuvres as risk factors for perineal trauma. Int Urogynecol J. 2016; 27: 571-577.
- Gurol-Urganci I, Cromwell DA, Edozien LC, Mahmood TA, Adams EJ, Richmond DH, et al. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: Time trends and risk factors. BJOG An Int J Obstet Gynaecol. 2013; 120: 1516-1525.